Monday Poster Session
Category: GI Bleeding
P3121 - ACG- a Forgotten Hematemesis Syndrome
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- BM
Bireera Muzaffar, MD (she/her/hers)
University of Oklahoma
Oklahoma City, OK
Presenting Author(s)
Sadia Ansari, MD1, Bireera Muzaffar, MD1, Katherine Janike, MD2, Alizay Khan, MD3, Ijlal Akbar. Ali, MD1
1University of Oklahoma, Oklahoma City, OK; 2Oklahoma University Health Sciences Center, Oklahoma City, OK; 3Ascension Saint Joseph Hospital, Chicago, IL
Introduction: Axon Clarke Gastropathy (ACG) is a rare gastrointestinal disorder involving gastric mucosal damage, commonly triggered by recurrent vomiting and retching. Symptoms like nausea, vomiting, and epigastric pain resemble cyclic vomiting syndrome (CVS) or functional dyspepsia (FD), complicating diagnosis. Severe cases may present with hematemesis or melena. Only 20–30% of cases are correctly diagnosed, and many remain unidentified until significant gastric injury occurs highlighting the need for early recognition.
First described by Axon and Clarke in 1975, ACG has been infrequently reported. It is often associated with psychiatric conditions (e.g., anxiety, depression) and chronic cannabis use. Hallmark endoscopic findings are erythema, hemorrhage, and mucosal prolapse help distinguish ACG from other GI disorders. Yet limited literature and lack of awareness delay diagnosis and treatment.
This case series presents two patients with recurrent vomiting and gastric injury, underscoring diagnostic challenges. We aim to expand the differential, encourage timely recognition, and support multidisciplinary care.
Case Description/
Methods: Case 1:
A 28-year-old man with ADHD, anxiety, depression, hyperlipidemia, and daily cannabis use presented with two days of intractable nausea, vomiting, and dark emesis, preceded by epigastric burning and decreased appetite. Hemoglobin fell from 14 g/dL to 7.2 g/dL, indicating GI bleeding. CT was unremarkable. Endoscopy showed hemorrhagic, erythematous, and prolapsing mucosa in the stomach body.
Case 2:
A 66-year-old man with GERD (on lansoprazole), treated Hepatitis C, and daily cannabis use had four days of nausea, vomiting, and hematemesis with clots. On presentation, he was stable (Hgb 13.1, platelets 268, INR 1.4). CT revealed diffuse gastric inflammation. Endoscopy showed erythematous mucosa with submucosal hematoma and old heme in the gastric body. Biopsies confirmed hemorrhage in the lamina propria and reactive gastropathy.
Discussion: Axon and Clarke initially described hematemesis and bright red gastric mucosa prolapsing into the esophagus. In our cases, damage was also concentrated in the proximal stomach, within 5 cm of the GE junction, often along the lesser curvature. This differentiates ACG from Mallory-Weiss tears. Early recognition helps guide treatment to control vomiting and prevent mucosal injury. Although bleeding is often self-limited, prompt diagnosis improves outcomes.
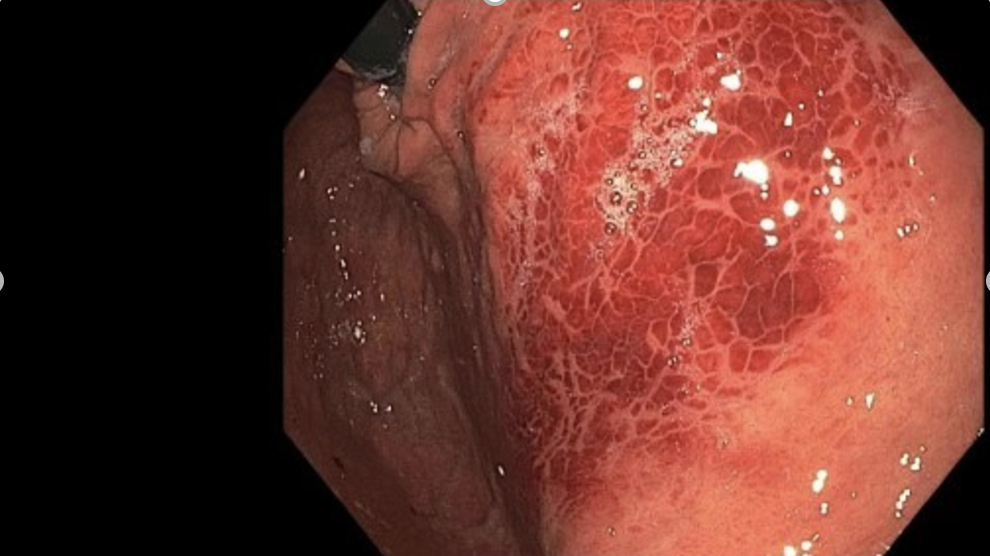
Figure: ACG
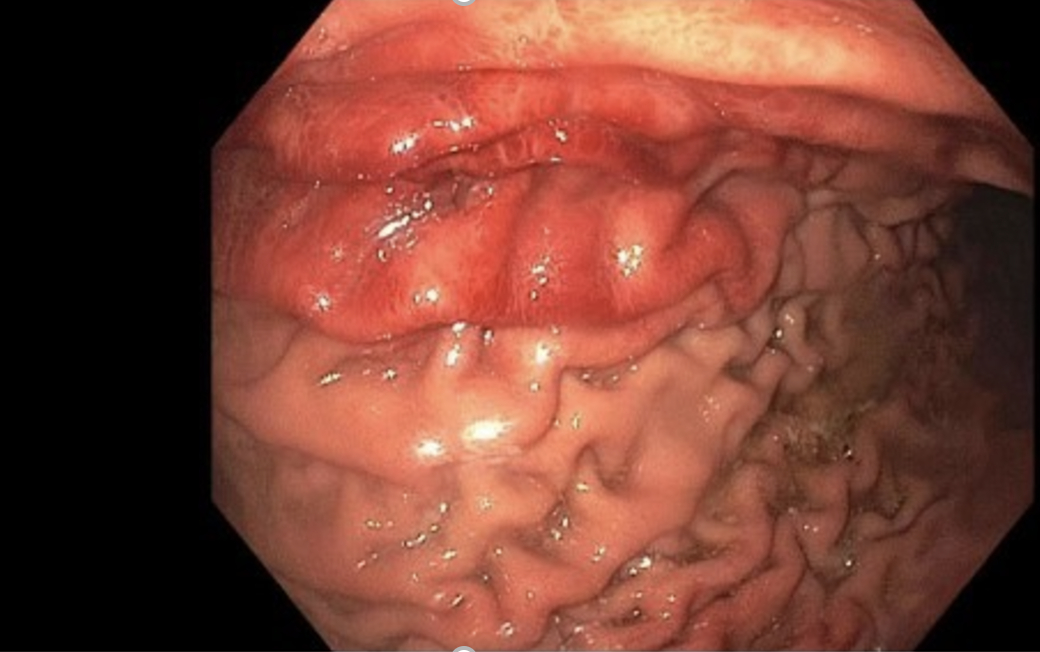
Figure: ACG
Disclosures:
Sadia Ansari indicated no relevant financial relationships.
Bireera Muzaffar indicated no relevant financial relationships.
Katherine Janike indicated no relevant financial relationships.
Alizay Khan indicated no relevant financial relationships.
Ijlal Ali indicated no relevant financial relationships.
Sadia Ansari, MD1, Bireera Muzaffar, MD1, Katherine Janike, MD2, Alizay Khan, MD3, Ijlal Akbar. Ali, MD1. P3121 - ACG- a Forgotten Hematemesis Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Oklahoma, Oklahoma City, OK; 2Oklahoma University Health Sciences Center, Oklahoma City, OK; 3Ascension Saint Joseph Hospital, Chicago, IL
Introduction: Axon Clarke Gastropathy (ACG) is a rare gastrointestinal disorder involving gastric mucosal damage, commonly triggered by recurrent vomiting and retching. Symptoms like nausea, vomiting, and epigastric pain resemble cyclic vomiting syndrome (CVS) or functional dyspepsia (FD), complicating diagnosis. Severe cases may present with hematemesis or melena. Only 20–30% of cases are correctly diagnosed, and many remain unidentified until significant gastric injury occurs highlighting the need for early recognition.
First described by Axon and Clarke in 1975, ACG has been infrequently reported. It is often associated with psychiatric conditions (e.g., anxiety, depression) and chronic cannabis use. Hallmark endoscopic findings are erythema, hemorrhage, and mucosal prolapse help distinguish ACG from other GI disorders. Yet limited literature and lack of awareness delay diagnosis and treatment.
This case series presents two patients with recurrent vomiting and gastric injury, underscoring diagnostic challenges. We aim to expand the differential, encourage timely recognition, and support multidisciplinary care.
Case Description/
Methods: Case 1:
A 28-year-old man with ADHD, anxiety, depression, hyperlipidemia, and daily cannabis use presented with two days of intractable nausea, vomiting, and dark emesis, preceded by epigastric burning and decreased appetite. Hemoglobin fell from 14 g/dL to 7.2 g/dL, indicating GI bleeding. CT was unremarkable. Endoscopy showed hemorrhagic, erythematous, and prolapsing mucosa in the stomach body.
Case 2:
A 66-year-old man with GERD (on lansoprazole), treated Hepatitis C, and daily cannabis use had four days of nausea, vomiting, and hematemesis with clots. On presentation, he was stable (Hgb 13.1, platelets 268, INR 1.4). CT revealed diffuse gastric inflammation. Endoscopy showed erythematous mucosa with submucosal hematoma and old heme in the gastric body. Biopsies confirmed hemorrhage in the lamina propria and reactive gastropathy.
Discussion: Axon and Clarke initially described hematemesis and bright red gastric mucosa prolapsing into the esophagus. In our cases, damage was also concentrated in the proximal stomach, within 5 cm of the GE junction, often along the lesser curvature. This differentiates ACG from Mallory-Weiss tears. Early recognition helps guide treatment to control vomiting and prevent mucosal injury. Although bleeding is often self-limited, prompt diagnosis improves outcomes.
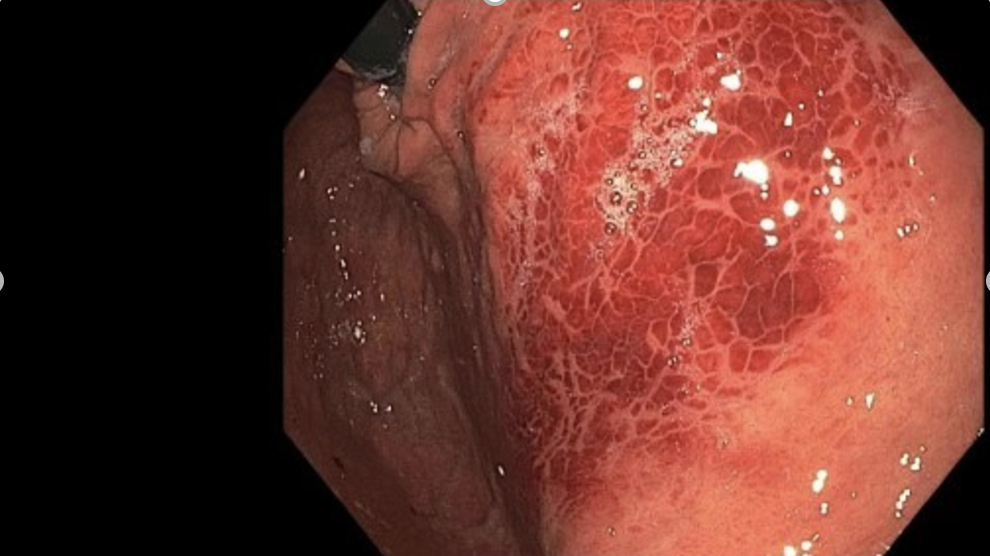
Figure: ACG
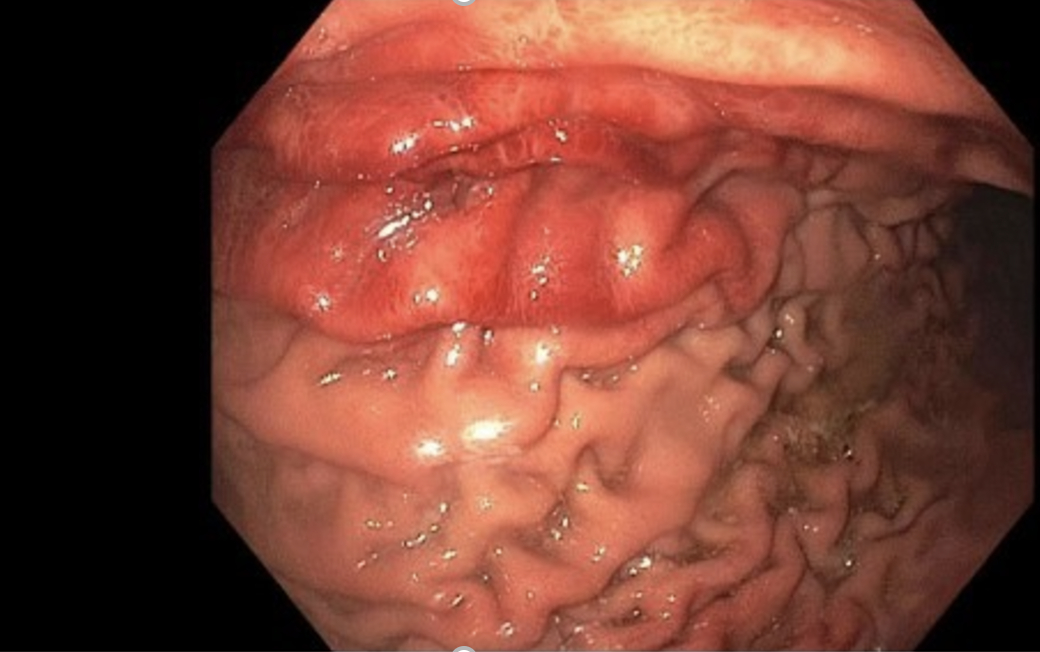
Figure: ACG
Disclosures:
Sadia Ansari indicated no relevant financial relationships.
Bireera Muzaffar indicated no relevant financial relationships.
Katherine Janike indicated no relevant financial relationships.
Alizay Khan indicated no relevant financial relationships.
Ijlal Ali indicated no relevant financial relationships.
Sadia Ansari, MD1, Bireera Muzaffar, MD1, Katherine Janike, MD2, Alizay Khan, MD3, Ijlal Akbar. Ali, MD1. P3121 - ACG- a Forgotten Hematemesis Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
