Monday Poster Session
Category: GI Bleeding
P3115 - Checkpoint Chaos: Immune Checkpoint Inhibitor Mediated Massive Hemorrhagic Gastritis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Samreen Jawaid, MD
Indiana University School of Medicine
Indianapolis, IN
Presenting Author(s)
Samreen Jawaid, MD1, Ambar Godoy, MD2, Daniel Guifarro Rivera, MD3, Namra Pasha, MBBS4, Kashif Ali, MD5, Eleazar E.. Montalvan-Sanchez, MD6
1Indiana University School of Medicine, Indianapolis, IN; 2Indiana University, Indianapolis, IN; 3Cook County Health and Hospital Systems, Chicago, IL; 4Karachi Medical and Dental College, Karachi, Sindh, Pakistan; 5University of Texas Rio Grande Valley, Edinburg, TX; 6Yale University School of Medicine, New Haven, CT
Introduction: Immune-checkpoint inhibitors (ICI), which block the cytotoxic T lymphocyte antigen 4 (CTLA-4) or programmed cell death protein 1 (PD-1) pathways, are being increasingly used for treatment of various malignancies. However, they pose a serious risk of gastrointestinal (GI) immune-related adverse events (irAEs), although upper GI manifestations are rare. We present a unique case of delayed-onset ICI-induced erosive duodenitis complicated by massive hemorrhagic and gastric outlet syndromes.
Case Description/
Methods: A 57-year-old male with history of metastatic renal cell carcinoma previously failed treatment with Nivolumab and Ipilumab, followed limited response to Pembrolizumab. 3 months later, he presented with coffee ground emesis. CT chest showed increased lung metastasis with cavitation, concerning for hemoptysis and endoscopy was deferred. On day 3, he developed abdominal pain and vomiting with a rapid drop in hemoglobin from 14 to 10 g/dL. CT abdomen revealed gastric outlet obstruction due to superior mesenteric artery (SMA) syndrome (Figure 1). Endoscopy identified multiple duodenal ulcers. Biopsies showed erosive duodenitis with increased apoptotic bodies and extensive crypt dropout (Figure 2). A percutaneous endoscopic gastrostomy tube with jejunostomy tube (PEG-J) was placed for decompression and enteral nutrition. On day 21, he developed massive upper GI bleeding from PEG-J site requiring massive transfusion protocol. A bleeding duodenal ulcer was identified and treated with bipolar therapy. High dose steroids were started, and ICI therapy was discontinued.
Discussion: This case underscores three clinical aspects of ICI toxicity. First, GI irAEs may well present beyond the typical 3–6-week window after ICI initiation, necessitating vigilance throughout the treatment course. Second, histopathologic features like crypt dropout and apoptotic bodies highlight the extent of mucosal injury, suggesting a pathophysiological basis for hemorrhage through mucosal friability. While apoptotic bodies are a nonspecific finding also seen in viral, drug-induced, or autoimmune processes, their presence in this clinical context strongly supports immune-mediated injury. Third, the presence of SMA syndrome exacerbated the clinical course by impairing nutrition and delaying mucosal healing. Early PEG-J placement was key for both decompression and nutritional support. Therefore, prompt recognition, biopsy, and multidisciplinary management are critical to balancing immunosuppression with oncologic control.
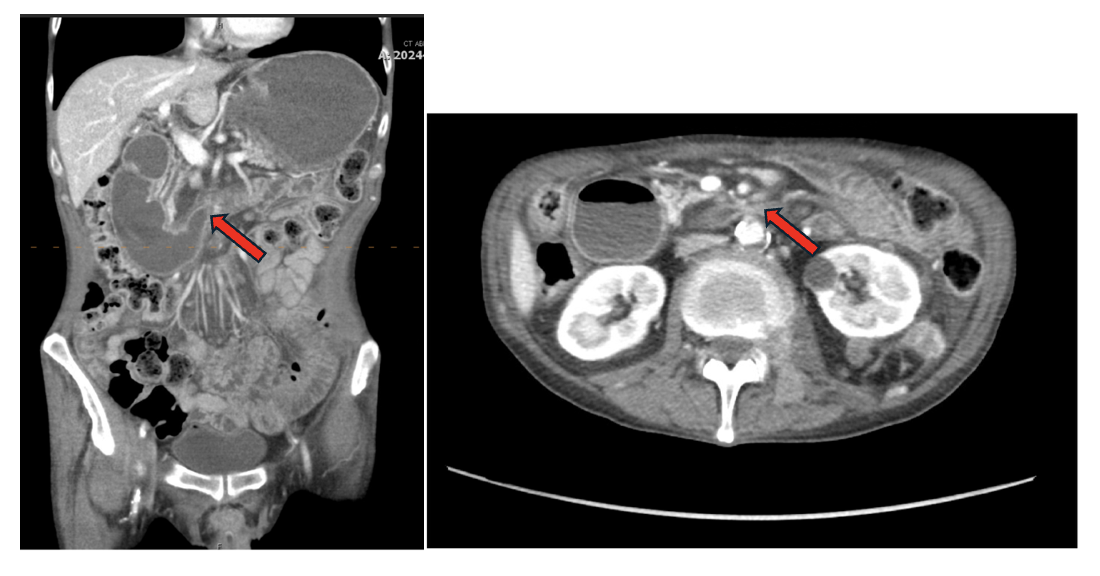
Figure: Figure 1: Gastric outlet syndrome from superior mesenteric artery.
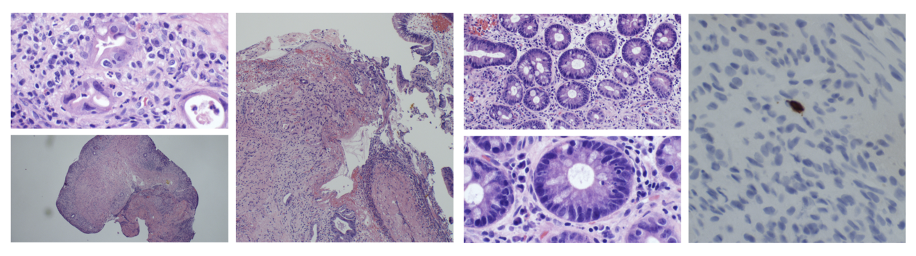
Figure: Figure 2: Erosive duodenitis with focal activity, increased apoptotic bodies and extensive crypt dropout. Stain for adenovirus negative.
Disclosures:
Samreen Jawaid indicated no relevant financial relationships.
Ambar Godoy indicated no relevant financial relationships.
Daniel Guifarro Rivera indicated no relevant financial relationships.
Namra Pasha indicated no relevant financial relationships.
Kashif Ali indicated no relevant financial relationships.
Eleazar Montalvan-Sanchez indicated no relevant financial relationships.
Samreen Jawaid, MD1, Ambar Godoy, MD2, Daniel Guifarro Rivera, MD3, Namra Pasha, MBBS4, Kashif Ali, MD5, Eleazar E.. Montalvan-Sanchez, MD6. P3115 - Checkpoint Chaos: Immune Checkpoint Inhibitor Mediated Massive Hemorrhagic Gastritis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Indiana University School of Medicine, Indianapolis, IN; 2Indiana University, Indianapolis, IN; 3Cook County Health and Hospital Systems, Chicago, IL; 4Karachi Medical and Dental College, Karachi, Sindh, Pakistan; 5University of Texas Rio Grande Valley, Edinburg, TX; 6Yale University School of Medicine, New Haven, CT
Introduction: Immune-checkpoint inhibitors (ICI), which block the cytotoxic T lymphocyte antigen 4 (CTLA-4) or programmed cell death protein 1 (PD-1) pathways, are being increasingly used for treatment of various malignancies. However, they pose a serious risk of gastrointestinal (GI) immune-related adverse events (irAEs), although upper GI manifestations are rare. We present a unique case of delayed-onset ICI-induced erosive duodenitis complicated by massive hemorrhagic and gastric outlet syndromes.
Case Description/
Methods: A 57-year-old male with history of metastatic renal cell carcinoma previously failed treatment with Nivolumab and Ipilumab, followed limited response to Pembrolizumab. 3 months later, he presented with coffee ground emesis. CT chest showed increased lung metastasis with cavitation, concerning for hemoptysis and endoscopy was deferred. On day 3, he developed abdominal pain and vomiting with a rapid drop in hemoglobin from 14 to 10 g/dL. CT abdomen revealed gastric outlet obstruction due to superior mesenteric artery (SMA) syndrome (Figure 1). Endoscopy identified multiple duodenal ulcers. Biopsies showed erosive duodenitis with increased apoptotic bodies and extensive crypt dropout (Figure 2). A percutaneous endoscopic gastrostomy tube with jejunostomy tube (PEG-J) was placed for decompression and enteral nutrition. On day 21, he developed massive upper GI bleeding from PEG-J site requiring massive transfusion protocol. A bleeding duodenal ulcer was identified and treated with bipolar therapy. High dose steroids were started, and ICI therapy was discontinued.
Discussion: This case underscores three clinical aspects of ICI toxicity. First, GI irAEs may well present beyond the typical 3–6-week window after ICI initiation, necessitating vigilance throughout the treatment course. Second, histopathologic features like crypt dropout and apoptotic bodies highlight the extent of mucosal injury, suggesting a pathophysiological basis for hemorrhage through mucosal friability. While apoptotic bodies are a nonspecific finding also seen in viral, drug-induced, or autoimmune processes, their presence in this clinical context strongly supports immune-mediated injury. Third, the presence of SMA syndrome exacerbated the clinical course by impairing nutrition and delaying mucosal healing. Early PEG-J placement was key for both decompression and nutritional support. Therefore, prompt recognition, biopsy, and multidisciplinary management are critical to balancing immunosuppression with oncologic control.
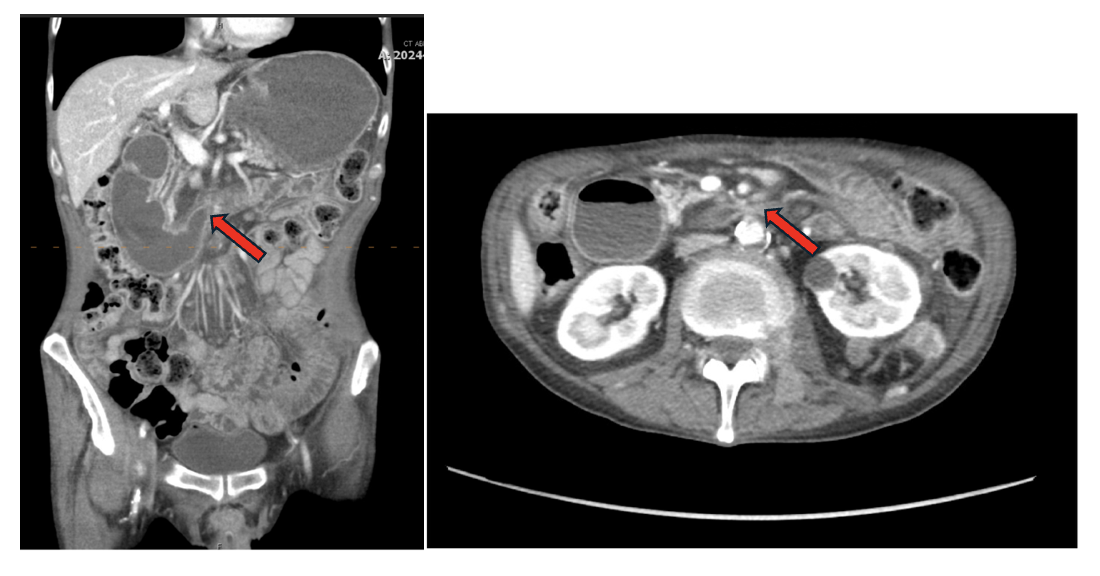
Figure: Figure 1: Gastric outlet syndrome from superior mesenteric artery.
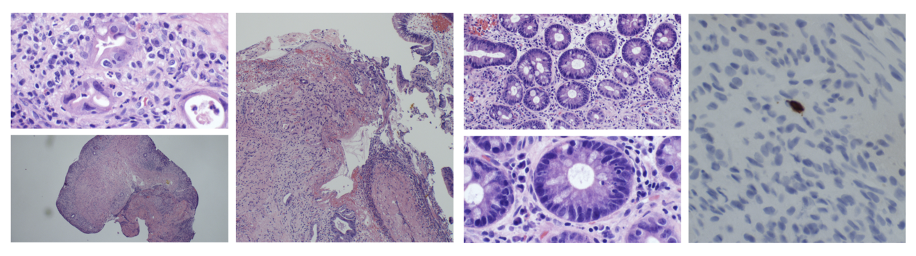
Figure: Figure 2: Erosive duodenitis with focal activity, increased apoptotic bodies and extensive crypt dropout. Stain for adenovirus negative.
Disclosures:
Samreen Jawaid indicated no relevant financial relationships.
Ambar Godoy indicated no relevant financial relationships.
Daniel Guifarro Rivera indicated no relevant financial relationships.
Namra Pasha indicated no relevant financial relationships.
Kashif Ali indicated no relevant financial relationships.
Eleazar Montalvan-Sanchez indicated no relevant financial relationships.
Samreen Jawaid, MD1, Ambar Godoy, MD2, Daniel Guifarro Rivera, MD3, Namra Pasha, MBBS4, Kashif Ali, MD5, Eleazar E.. Montalvan-Sanchez, MD6. P3115 - Checkpoint Chaos: Immune Checkpoint Inhibitor Mediated Massive Hemorrhagic Gastritis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
