Monday Poster Session
Category: IBD
P3205 - Patients With Inflammatory Bowel Disease Have Increased Risk of Complications on Dual Antiplatelet Therapy After Percutaneous Coronary Intervention
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- UB
Umesh Bhagat, MD
Cleveland Clinic Foundation
Cleveland, OH
Presenting Author(s)
Umesh Bhagat, MD1, Ankit Agrawal, 2, Bala Pushparaji, MD3, Jean-Paul Achkar, MD, FACG2
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic, Cleveland, OH; 3Case Western Reserve University / MetroHealth, Cleveland, OH
Introduction: Dual antiplatelet therapy (DAPT) following percutaneous coronary intervention (PCI) in patients with acute coronary syndrome (ACS) remains a cornerstone in preventing thrombotic events. Data on the safety and long-term effects of antiplatelet use in patients with inflammatory bowel disease (IBD) who may be at higher risk of complications are limited. This study aimed to assess the outcomes of DAPT use in patients with IBD.
Methods: We conducted a retrospective cohort study using the multi-institutional TriNetX research network to evaluate the risk of adverse outcomes in patients who underwent PCI and were prescribed DAPT (aspirin and clopidogrel). These patients were divided into two cohorts with and without IBD. One-to-one propensity score matching was performed based on demographics and PCI-related risk factors. Outcomes were reported as adjusted odds ratios (aOR) with 95% confidence intervals (CI).
Results: A total of 3,696 patients with IBD and 196,662 patients without IBD who underwent PCI and were started on DAPT were compared. At one-month post-PCI, patients with IBD had lower odds of all-cause hospitalization (aOR 0.62, 95% CI: 0.40–0.98, p < 0.04), but there were no significant differences in all-cause mortality, acute heart failure, deep vein thrombosis (DVT), stroke or gastrointestinal (GI) bleeding compared to non-IBD controls (Table 1). At 6 months post-PCI, IBD patients had significantly higher odds of all-cause mortality (aOR 1.36, p < 0.01), acute heart failure (aOR 1.24, p < 0.01), DVT (aOR 1.32, p < 0.01), and GI bleeding (aOR 1.47, p < 0.01). At 12 months post-PCI, these trends persisted, with increased odds of all-cause mortality (aOR 1.50, p < 0.01), acute heart failure (aOR 1.32, p < 0.01), DVT (aOR 1.46, p < 0.01), and GI bleeding (aOR 1.61, p < 0.01). No significant differences were observed in stroke or all-cause hospitalization at 6 or 12 months (Tables 2, 3).
Discussion: While DAPT is essential following PCI, patients with IBD may experience significantly higher long-term risks of adverse outcomes. These risks become more apparent at 6 and 12 months post-PCI including higher odds of mortality, DVT, heart failure and GI bleeding. There is likely an interplay between the underlying inflammation related to IBD and increased risk of anticoagulation leading to these findings. Clinicians should weigh the benefits of DAPT against bleeding and thrombotic risks in this population and consider personalized risk stratification and closer monitoring.
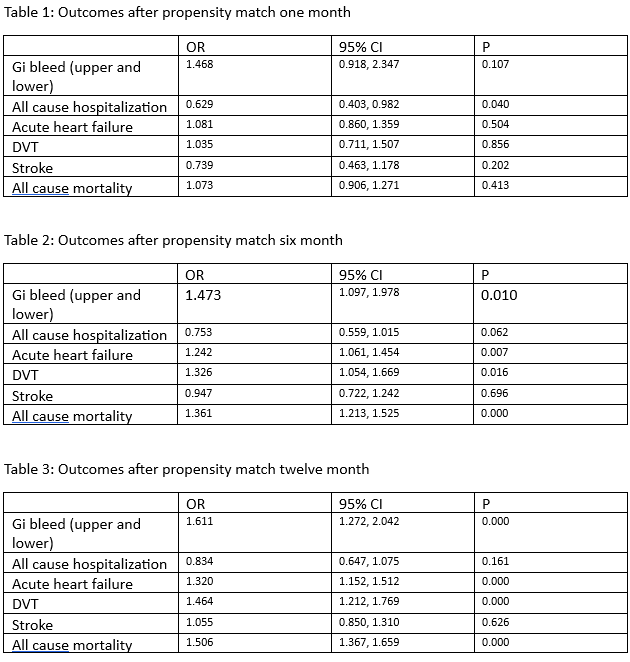
Figure: Outcomes in IBD witth use of DAPT therapy
Disclosures:
Umesh Bhagat indicated no relevant financial relationships.
Ankit Agrawal indicated no relevant financial relationships.
Bala Pushparaji indicated no relevant financial relationships.
Jean-Paul Achkar indicated no relevant financial relationships.
Umesh Bhagat, MD1, Ankit Agrawal, 2, Bala Pushparaji, MD3, Jean-Paul Achkar, MD, FACG2. P3205 - Patients With Inflammatory Bowel Disease Have Increased Risk of Complications on Dual Antiplatelet Therapy After Percutaneous Coronary Intervention, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic, Cleveland, OH; 3Case Western Reserve University / MetroHealth, Cleveland, OH
Introduction: Dual antiplatelet therapy (DAPT) following percutaneous coronary intervention (PCI) in patients with acute coronary syndrome (ACS) remains a cornerstone in preventing thrombotic events. Data on the safety and long-term effects of antiplatelet use in patients with inflammatory bowel disease (IBD) who may be at higher risk of complications are limited. This study aimed to assess the outcomes of DAPT use in patients with IBD.
Methods: We conducted a retrospective cohort study using the multi-institutional TriNetX research network to evaluate the risk of adverse outcomes in patients who underwent PCI and were prescribed DAPT (aspirin and clopidogrel). These patients were divided into two cohorts with and without IBD. One-to-one propensity score matching was performed based on demographics and PCI-related risk factors. Outcomes were reported as adjusted odds ratios (aOR) with 95% confidence intervals (CI).
Results: A total of 3,696 patients with IBD and 196,662 patients without IBD who underwent PCI and were started on DAPT were compared. At one-month post-PCI, patients with IBD had lower odds of all-cause hospitalization (aOR 0.62, 95% CI: 0.40–0.98, p < 0.04), but there were no significant differences in all-cause mortality, acute heart failure, deep vein thrombosis (DVT), stroke or gastrointestinal (GI) bleeding compared to non-IBD controls (Table 1). At 6 months post-PCI, IBD patients had significantly higher odds of all-cause mortality (aOR 1.36, p < 0.01), acute heart failure (aOR 1.24, p < 0.01), DVT (aOR 1.32, p < 0.01), and GI bleeding (aOR 1.47, p < 0.01). At 12 months post-PCI, these trends persisted, with increased odds of all-cause mortality (aOR 1.50, p < 0.01), acute heart failure (aOR 1.32, p < 0.01), DVT (aOR 1.46, p < 0.01), and GI bleeding (aOR 1.61, p < 0.01). No significant differences were observed in stroke or all-cause hospitalization at 6 or 12 months (Tables 2, 3).
Discussion: While DAPT is essential following PCI, patients with IBD may experience significantly higher long-term risks of adverse outcomes. These risks become more apparent at 6 and 12 months post-PCI including higher odds of mortality, DVT, heart failure and GI bleeding. There is likely an interplay between the underlying inflammation related to IBD and increased risk of anticoagulation leading to these findings. Clinicians should weigh the benefits of DAPT against bleeding and thrombotic risks in this population and consider personalized risk stratification and closer monitoring.
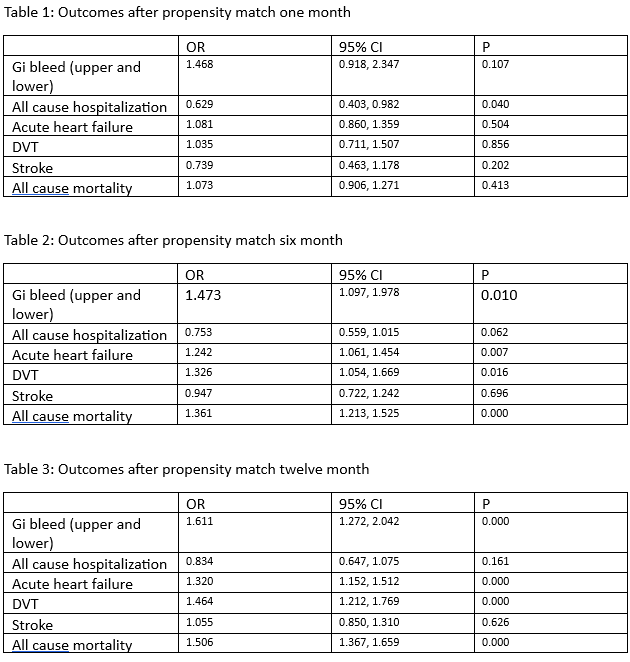
Figure: Outcomes in IBD witth use of DAPT therapy
Disclosures:
Umesh Bhagat indicated no relevant financial relationships.
Ankit Agrawal indicated no relevant financial relationships.
Bala Pushparaji indicated no relevant financial relationships.
Jean-Paul Achkar indicated no relevant financial relationships.
Umesh Bhagat, MD1, Ankit Agrawal, 2, Bala Pushparaji, MD3, Jean-Paul Achkar, MD, FACG2. P3205 - Patients With Inflammatory Bowel Disease Have Increased Risk of Complications on Dual Antiplatelet Therapy After Percutaneous Coronary Intervention, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
