Monday Poster Session
Category: IBD
P3200 - No Difference Seen in Disease Activity in Crohn's Disease and Ulcerative Colitis Patients With Normal Versus Elevated BMI
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Cindy Xin Fang, BS (she/her/hers)
Sidney Kimmel Medical College at Thomas Jefferson University
Philadelphia, PA
Presenting Author(s)
Cindy Xin Fang, BS1, Sanjna Shelukar, MD2, Bertilia Tavarez, MD2, Kevan Josloff, MD, MPH2, Vaishnavi Nara, BS1, Cuckoo Choudhary, MD3, Patricia L. Kozuch, MD2, Raina Shivashankar, MD2, Priya Sehgal, MD2
1Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA; 2Thomas Jefferson University Hospital, Philadelphia, PA; 3Thomas Jefferson University Hospital (Philadelphia, PA), Philadelphia, PA
Introduction: Emerging evidence suggests that obesity is associated with increased disease activity and a reduced time to flare in inflammatory bowel disease (IBD). Obesity in patients with IBD is associated with decreased rate of endoscopic remission and decreased time to flare through a hypothesized increase in proinflammatory adipokines. In this cross-sectional study, we aimed to evaluate the association between body mass index (BMI) and endoscopic disease activity in patients with IBD.
Methods: We conducted a cross-sectional study of patients with CD or UC who underwent colonoscopy at a tertiary care center from January to December 2024. Demographic and clinical data, including age, sex, race, BMI, IBD phenotype, comorbidities, IBD medications, and steroid use were extracted from the electronic health record. Patients on GLP-1RA therapy were excluded. Disease activity was assessed via Mayo endoscopic score (UC) and SEMA-CD score (CD), and categorized as remission (Mayo: 0, SEMA-CD: 0), mild (Mayo: 1, SEMA-CD: 1–4), moderate (Mayo: 2, SEMA-CD: 5–9), and severe (Mayo: 3, SEMA-CD ≥10). Disease activity was compared between patients with obesity, defined as BMI ≥30 kg/m2, and normal weight, defined as BMI 18.5–24.9 kg/m2 using t-test analysis. Multivariable linear regression was used to identify predictors of disease activity.
Results: A total of 399 IBD patients were included (CD 150, UC 248). Of these, 212 were female (53%) and 161 had obesity (BMI ≥ 30) while 238 had normal BMI (18.5 – 24.9). Mean disease activity scores were comparable between obese and normal BMI patients (mean difference 0.02, 95% CI: -0.18 to 0.22, p = 0.849). In the multivariable linear regression analysis, BMI was not a significant predictor of disease activity (β = 0.01, 95% CI: –0.01 to 0.02; p = 0.228). Duration of disease ≥ 5 years was associated with significantly lower disease activity compared to those with < 5 years (β = –0.42 to –0.45; p < 0.01). Other variables were not significantly associated with disease activity.
Discussion: No significant difference in disease activity was observed between obese and normal BMI in patients with CD or UC. These finding suggests that visceral adiposity, rather than BMI, may be a more relevant determinant of driving IBD disease activity. Future studies should evaluate visceral fat distribution on endoscopic outcomes in IBD.
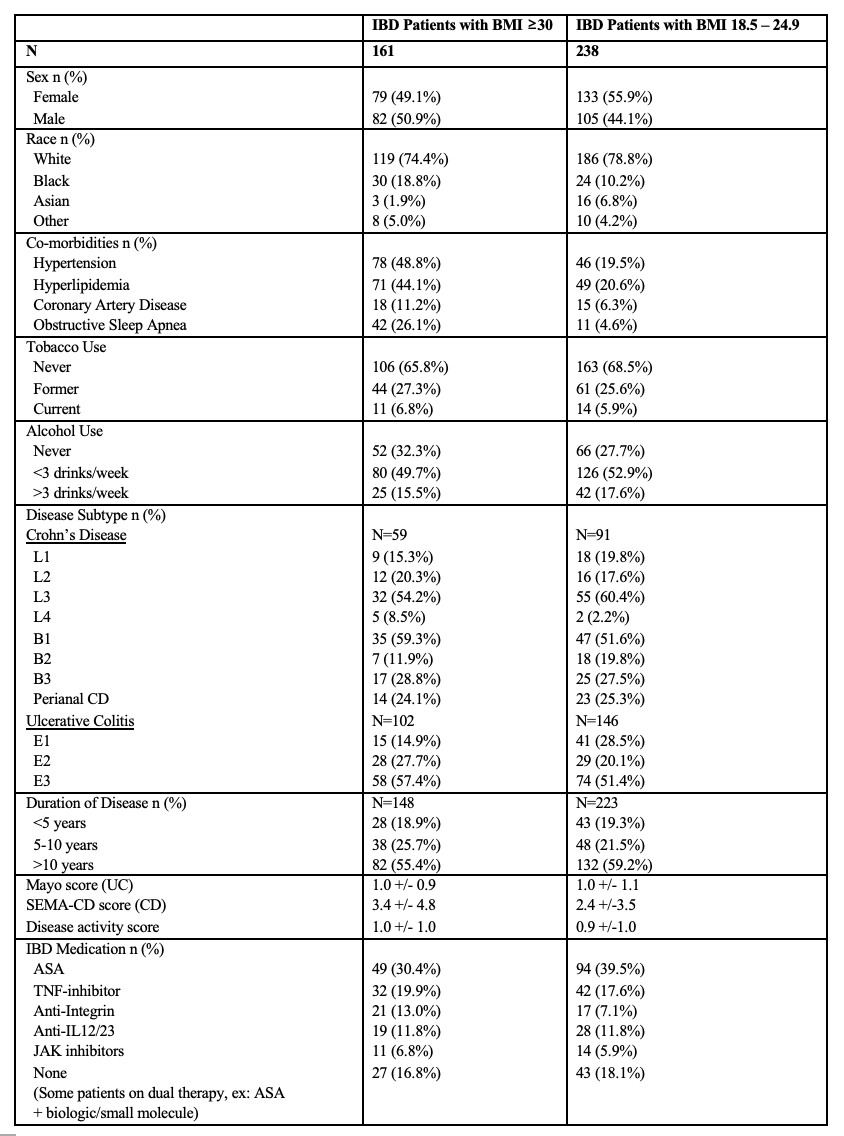
Figure: Table 1. Demographics and Clinical Characteristics of IBD Patients with BMI ≥30 and BMI 18.5 – 24.9
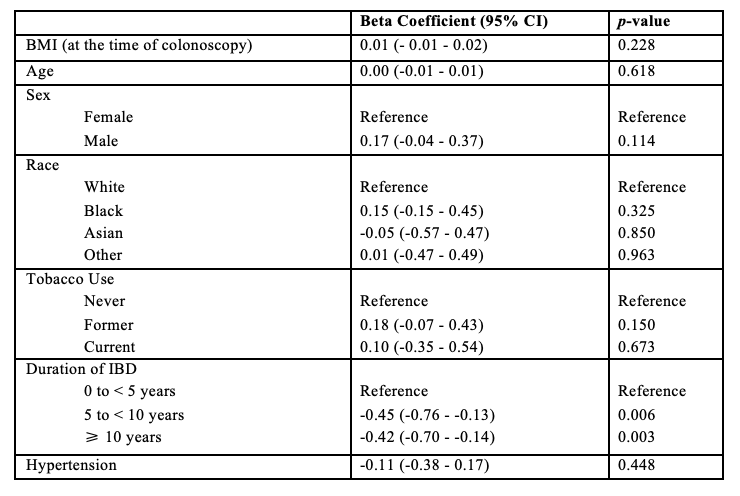
Figure: Table 2. Multivariable Linear Regression Identifying Predictors of IBD Disease Activity
Disclosures:
Cindy Xin Fang indicated no relevant financial relationships.
Sanjna Shelukar indicated no relevant financial relationships.
Bertilia Tavarez indicated no relevant financial relationships.
Kevan Josloff indicated no relevant financial relationships.
Vaishnavi Nara indicated no relevant financial relationships.
Cuckoo Choudhary indicated no relevant financial relationships.
Patricia Kozuch indicated no relevant financial relationships.
Raina Shivashankar: Abbvie – Speakers Bureau. BMS – Speakers Bureau. Janssen – Grant/Research Support. Pfizer – Consultant.
Priya Sehgal indicated no relevant financial relationships.
Cindy Xin Fang, BS1, Sanjna Shelukar, MD2, Bertilia Tavarez, MD2, Kevan Josloff, MD, MPH2, Vaishnavi Nara, BS1, Cuckoo Choudhary, MD3, Patricia L. Kozuch, MD2, Raina Shivashankar, MD2, Priya Sehgal, MD2. P3200 - No Difference Seen in Disease Activity in Crohn's Disease and Ulcerative Colitis Patients With Normal Versus Elevated BMI, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA; 2Thomas Jefferson University Hospital, Philadelphia, PA; 3Thomas Jefferson University Hospital (Philadelphia, PA), Philadelphia, PA
Introduction: Emerging evidence suggests that obesity is associated with increased disease activity and a reduced time to flare in inflammatory bowel disease (IBD). Obesity in patients with IBD is associated with decreased rate of endoscopic remission and decreased time to flare through a hypothesized increase in proinflammatory adipokines. In this cross-sectional study, we aimed to evaluate the association between body mass index (BMI) and endoscopic disease activity in patients with IBD.
Methods: We conducted a cross-sectional study of patients with CD or UC who underwent colonoscopy at a tertiary care center from January to December 2024. Demographic and clinical data, including age, sex, race, BMI, IBD phenotype, comorbidities, IBD medications, and steroid use were extracted from the electronic health record. Patients on GLP-1RA therapy were excluded. Disease activity was assessed via Mayo endoscopic score (UC) and SEMA-CD score (CD), and categorized as remission (Mayo: 0, SEMA-CD: 0), mild (Mayo: 1, SEMA-CD: 1–4), moderate (Mayo: 2, SEMA-CD: 5–9), and severe (Mayo: 3, SEMA-CD ≥10). Disease activity was compared between patients with obesity, defined as BMI ≥30 kg/m2, and normal weight, defined as BMI 18.5–24.9 kg/m2 using t-test analysis. Multivariable linear regression was used to identify predictors of disease activity.
Results: A total of 399 IBD patients were included (CD 150, UC 248). Of these, 212 were female (53%) and 161 had obesity (BMI ≥ 30) while 238 had normal BMI (18.5 – 24.9). Mean disease activity scores were comparable between obese and normal BMI patients (mean difference 0.02, 95% CI: -0.18 to 0.22, p = 0.849). In the multivariable linear regression analysis, BMI was not a significant predictor of disease activity (β = 0.01, 95% CI: –0.01 to 0.02; p = 0.228). Duration of disease ≥ 5 years was associated with significantly lower disease activity compared to those with < 5 years (β = –0.42 to –0.45; p < 0.01). Other variables were not significantly associated with disease activity.
Discussion: No significant difference in disease activity was observed between obese and normal BMI in patients with CD or UC. These finding suggests that visceral adiposity, rather than BMI, may be a more relevant determinant of driving IBD disease activity. Future studies should evaluate visceral fat distribution on endoscopic outcomes in IBD.
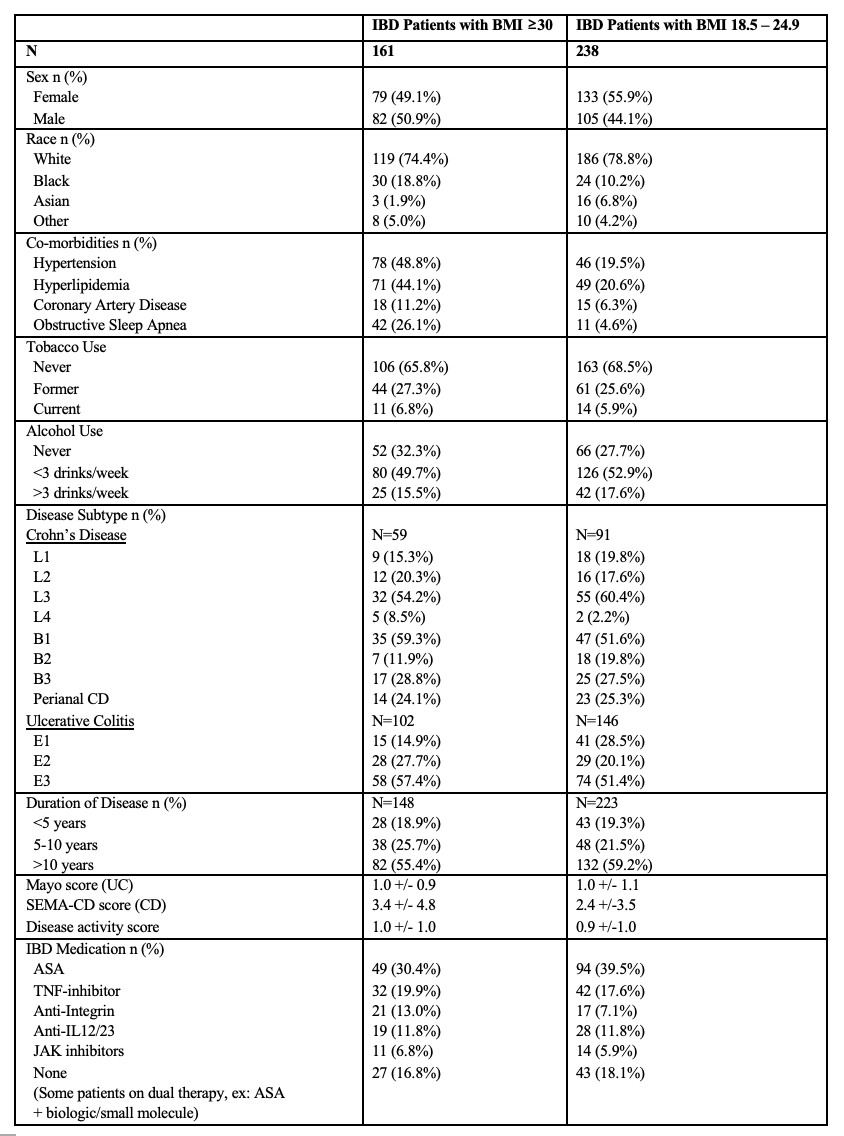
Figure: Table 1. Demographics and Clinical Characteristics of IBD Patients with BMI ≥30 and BMI 18.5 – 24.9
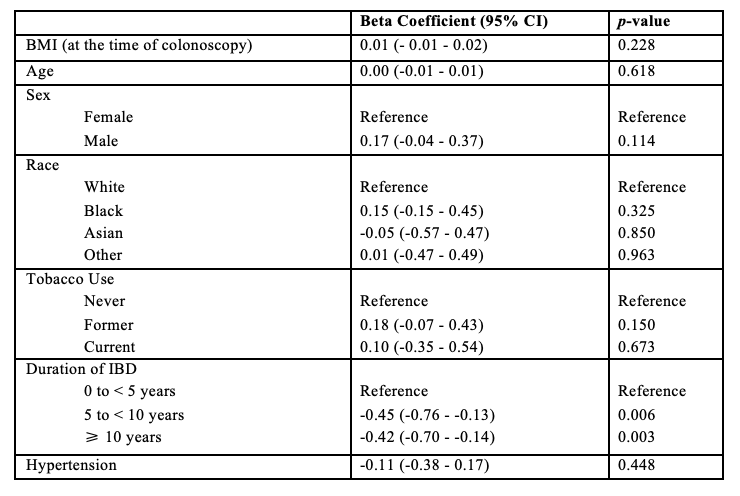
Figure: Table 2. Multivariable Linear Regression Identifying Predictors of IBD Disease Activity
Disclosures:
Cindy Xin Fang indicated no relevant financial relationships.
Sanjna Shelukar indicated no relevant financial relationships.
Bertilia Tavarez indicated no relevant financial relationships.
Kevan Josloff indicated no relevant financial relationships.
Vaishnavi Nara indicated no relevant financial relationships.
Cuckoo Choudhary indicated no relevant financial relationships.
Patricia Kozuch indicated no relevant financial relationships.
Raina Shivashankar: Abbvie – Speakers Bureau. BMS – Speakers Bureau. Janssen – Grant/Research Support. Pfizer – Consultant.
Priya Sehgal indicated no relevant financial relationships.
Cindy Xin Fang, BS1, Sanjna Shelukar, MD2, Bertilia Tavarez, MD2, Kevan Josloff, MD, MPH2, Vaishnavi Nara, BS1, Cuckoo Choudhary, MD3, Patricia L. Kozuch, MD2, Raina Shivashankar, MD2, Priya Sehgal, MD2. P3200 - No Difference Seen in Disease Activity in Crohn's Disease and Ulcerative Colitis Patients With Normal Versus Elevated BMI, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

