Monday Poster Session
Category: IBD
P3294 - Is the Use of Systemic Corticosteroid Associated With Increased Risk of Colorectal Cancer in Inflammatory Bowel Diseases: A Large Retrospective Cohort Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Joelle Sleiman, MD
Staten Island University Hospital, Northwell Health
Staten Island, NY
Presenting Author(s)
Joelle Sleiman, MD1, Battoul Fakhry, MD2, Reem Dimachkie, MD1, Ryan Njeim, MD1, Uday Sankar Akash Vankayala, MBBS1, Liliane Deeb, MD1
1Staten Island University Hospital, Northwell Health, Staten Island, NY; 2Lerner Research Institute, Cleveland Clinic, Cleveland, OH
Introduction: Chronic inflammation in inflammatory bowel disease (IBD) is a well-established risk factor for colorectal cancer (CRC). While immunosuppressive and biologic therapies have been studied for their potential favorable impact on CRC risk, the role of systemic glucocorticoids remains unclear, and the published data show conflicting results. We aim to investigate the association between the use of systemic glucocorticoids and CRC risk in the IBD population.
Methods: We conducted a retrospective, multi-center cohort study at Northwell Health between 2008 and 2023. Among 11,325 patients with IBD (ulcerative colitis (UC) and Crohn’s disease (CD)), we excluded patients under 18 years, and if they had indeterminate colitis, or history of cancer prior to IBD diagnosis (n=370). Demographics and IBD medication data were extracted from the Northwell Health Information Exchange (HIE) database. The primary exposure was systemic corticosteroid use, and the primary outcome was CRC. Adjusted odds ratios (aORs) were estimated by logistic regression, controlling for age, sex, IBD type, and use of biologic and immunomodulator therapies. Analyses were stratified by sex, IBD type, and age group (≤50 and >50 years).
Results: Of the 10,955 study patients, 196 (1.8%) were diagnosed with CRC, and 4,375 (40%) were on chronic corticosteroid (Table 1). The use of corticosteroids was associated with a more than twofold increase in the odds of CRC (aOR 2.03, 95% CI 1.49-2.77). This elevated risk was consistent across IBD types, with similar associations in Crohn’s disease (aOR 1.91, 95% CI 1.17–3.13) and ulcerative colitis (aOR 2.09, 95% CI 1.27–3.42). Stratified analysis showed that both males (aOR 2.01, 95% CI 1.27-3.19) and females (aOR 1.90, 95% CI 1.16-3.11) experienced significantly higher risk of CRC with steroid exposure. Notably, the association was strongest among patients older than 50 years (aOR 2.16, 95% CI 1.48-3.15), while no significant association was seen in those 50 years or younger (aOR 1.29, 95% CI 0.64-2.62).
Discussion: Our study shows that corticosteroid use may be independently associated with a twofold increase in risk of CRC in patients with IBD, across sex and disease type. The risk was greatest in older patients. This finding may be explained by the inability to achieve deep remission and mucosal healing with steroid therapy. Future controlled studies are warranted to shed more light on this subject and further underscore the practice of steroid-sparing strategies in IBD management.
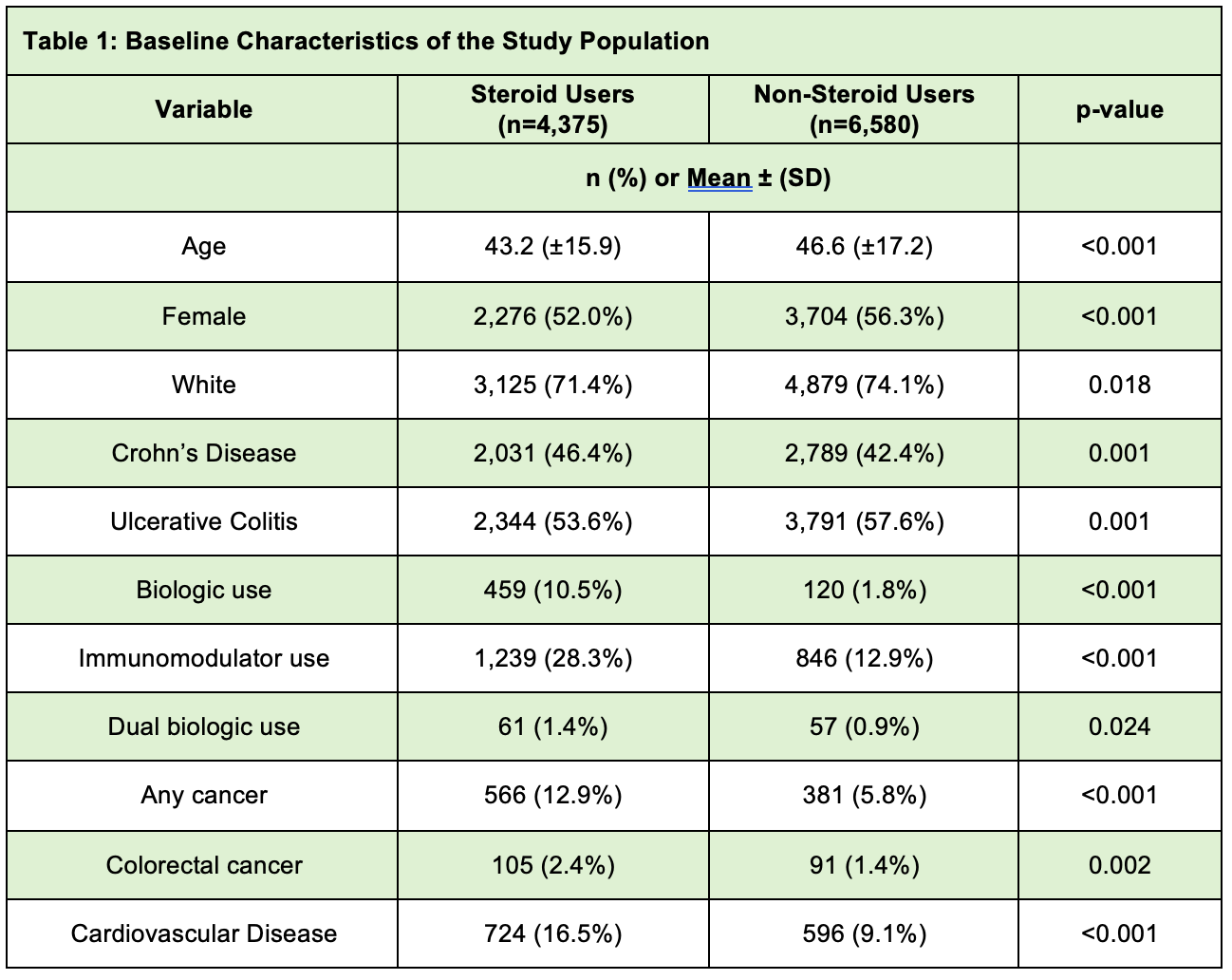
Figure: Baseline Characteristics of the Study Population
Disclosures:
Joelle Sleiman indicated no relevant financial relationships.
Battoul Fakhry indicated no relevant financial relationships.
Reem Dimachkie indicated no relevant financial relationships.
Ryan Njeim indicated no relevant financial relationships.
Uday Sankar Akash Vankayala indicated no relevant financial relationships.
Liliane Deeb indicated no relevant financial relationships.
Joelle Sleiman, MD1, Battoul Fakhry, MD2, Reem Dimachkie, MD1, Ryan Njeim, MD1, Uday Sankar Akash Vankayala, MBBS1, Liliane Deeb, MD1. P3294 - Is the Use of Systemic Corticosteroid Associated With Increased Risk of Colorectal Cancer in Inflammatory Bowel Diseases: A Large Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Staten Island University Hospital, Northwell Health, Staten Island, NY; 2Lerner Research Institute, Cleveland Clinic, Cleveland, OH
Introduction: Chronic inflammation in inflammatory bowel disease (IBD) is a well-established risk factor for colorectal cancer (CRC). While immunosuppressive and biologic therapies have been studied for their potential favorable impact on CRC risk, the role of systemic glucocorticoids remains unclear, and the published data show conflicting results. We aim to investigate the association between the use of systemic glucocorticoids and CRC risk in the IBD population.
Methods: We conducted a retrospective, multi-center cohort study at Northwell Health between 2008 and 2023. Among 11,325 patients with IBD (ulcerative colitis (UC) and Crohn’s disease (CD)), we excluded patients under 18 years, and if they had indeterminate colitis, or history of cancer prior to IBD diagnosis (n=370). Demographics and IBD medication data were extracted from the Northwell Health Information Exchange (HIE) database. The primary exposure was systemic corticosteroid use, and the primary outcome was CRC. Adjusted odds ratios (aORs) were estimated by logistic regression, controlling for age, sex, IBD type, and use of biologic and immunomodulator therapies. Analyses were stratified by sex, IBD type, and age group (≤50 and >50 years).
Results: Of the 10,955 study patients, 196 (1.8%) were diagnosed with CRC, and 4,375 (40%) were on chronic corticosteroid (Table 1). The use of corticosteroids was associated with a more than twofold increase in the odds of CRC (aOR 2.03, 95% CI 1.49-2.77). This elevated risk was consistent across IBD types, with similar associations in Crohn’s disease (aOR 1.91, 95% CI 1.17–3.13) and ulcerative colitis (aOR 2.09, 95% CI 1.27–3.42). Stratified analysis showed that both males (aOR 2.01, 95% CI 1.27-3.19) and females (aOR 1.90, 95% CI 1.16-3.11) experienced significantly higher risk of CRC with steroid exposure. Notably, the association was strongest among patients older than 50 years (aOR 2.16, 95% CI 1.48-3.15), while no significant association was seen in those 50 years or younger (aOR 1.29, 95% CI 0.64-2.62).
Discussion: Our study shows that corticosteroid use may be independently associated with a twofold increase in risk of CRC in patients with IBD, across sex and disease type. The risk was greatest in older patients. This finding may be explained by the inability to achieve deep remission and mucosal healing with steroid therapy. Future controlled studies are warranted to shed more light on this subject and further underscore the practice of steroid-sparing strategies in IBD management.
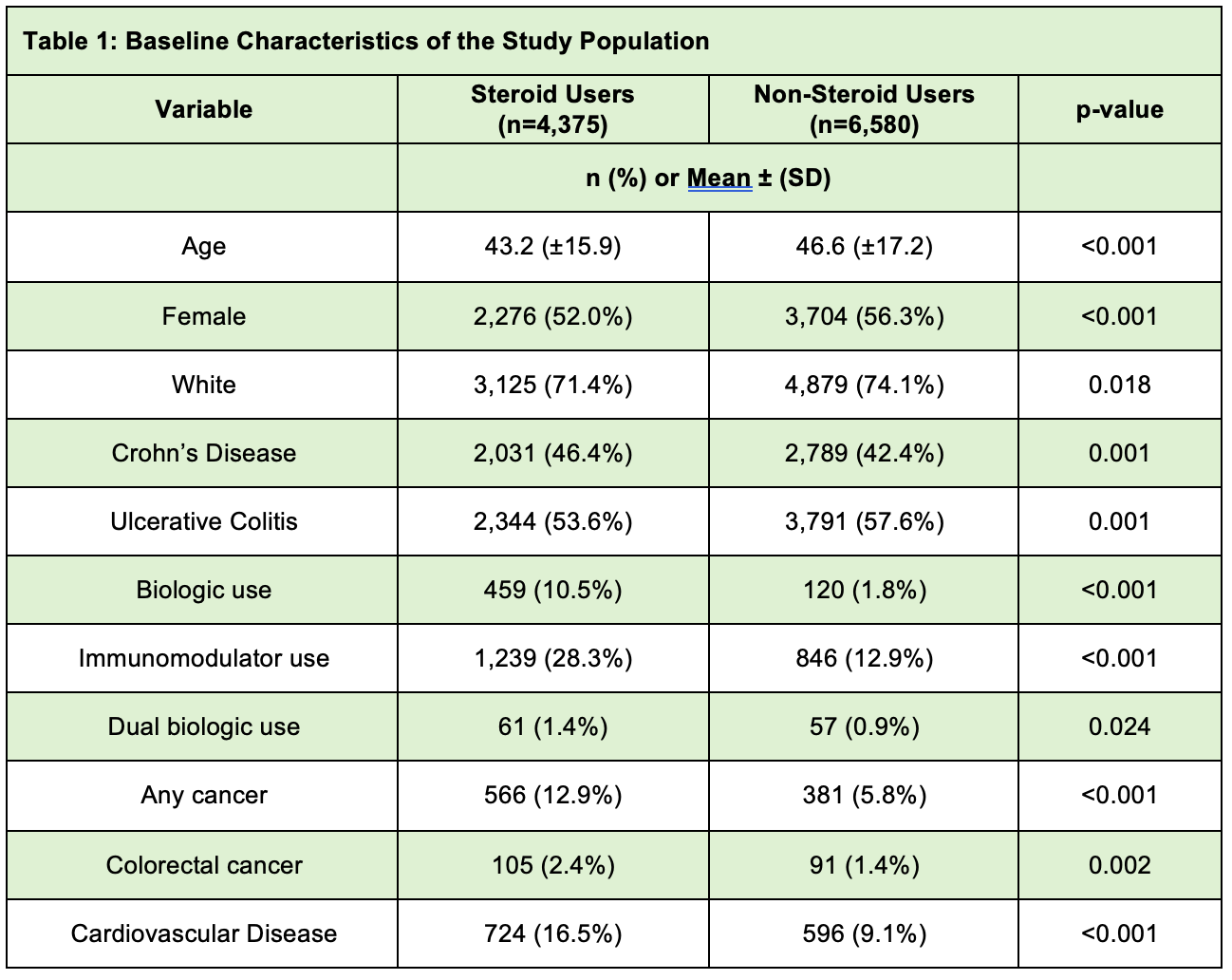
Figure: Baseline Characteristics of the Study Population
Disclosures:
Joelle Sleiman indicated no relevant financial relationships.
Battoul Fakhry indicated no relevant financial relationships.
Reem Dimachkie indicated no relevant financial relationships.
Ryan Njeim indicated no relevant financial relationships.
Uday Sankar Akash Vankayala indicated no relevant financial relationships.
Liliane Deeb indicated no relevant financial relationships.
Joelle Sleiman, MD1, Battoul Fakhry, MD2, Reem Dimachkie, MD1, Ryan Njeim, MD1, Uday Sankar Akash Vankayala, MBBS1, Liliane Deeb, MD1. P3294 - Is the Use of Systemic Corticosteroid Associated With Increased Risk of Colorectal Cancer in Inflammatory Bowel Diseases: A Large Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
