Monday Poster Session
Category: IBD
P3364 - Biologic Induction Therapy in Hospitalized Ulcerative Colitis With Latent Tuberculosis: A Case Series Emphasizing Individualized Care
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Zach Vinton, DO
University of Nebraska Medical Center
Omaha, NE
Presenting Author(s)
Zach Vinton, DO1, Jason Barbaretta, MD1, Nurlan Aliyev, MD2, Kathryn Hutchins, MD, FACG1
1University of Nebraska Medical Center, Omaha, NE; 2University of Nebraska Medical Center, Elkhorn, NE
Introduction: Initiating biologic therapy in Ulcerative Colitis (UC) and latent tuberculosis infection (LTBI) increases risk of LTBI reactivation. This poses a clinical challenge, particularly when inpatient, where urgent induction is often necessary. We present two cases with UC flares and concurrent LTBI requiring biologic therapy following steroid-refractory disease.
Case Description/
Methods: Case 1: A 24-year-old female with UC with a two-month history of >15 bloody stools daily. LTBI was diagnosed during outpatient pre-biologic screening, and rifampin was started one month prior to admission per infectious disease (ID) recommendation. On admission, she was hypotensive and tachycardic with CRP of 1.9 mg/dL. CT revealed proctosigmoiditis, and colonoscopy demonstrated Mayo 2 (moderate) pancolitis (Figure 1) with chronic active colitis and negative CMV staining. After failing a 72-hour intravenous (IV) steroid trial, vedolizumab was initiated with ID guidance. Her symptoms and CRP improved, and she was discharged on a steroid taper with plans for outpatient vedolizumab maintenance.
Case 2: A 48-year-old male with UC presented with 8 days of >10 bloody stools daily with abdominal pain and intermittent fevers. He was tachycardic with elevated CRP (13.4 mg/dL). CT showed pancolitis and colonoscopy revealed Mayo 3 (severe) colitis in the right colon with Mayo 2 (moderate) colitis in the left (Figure 2). After failing a 72-hour IV steroid trial, pre-biologic screening revealed LTBI. A multidisciplinary team initiated infliximab alongside isoniazid and B6. He showed rapid clinical improvement and was discharged with outpatient infliximab therapy.
At 1 and 4 months, both patients were without clinical or radiological evidence of active tuberculosis.
Discussion: Although infliximab or cyclosporine are the standard treatment for hospitalized patients with acute severe UC unresponsive to IV steroids, the presence of LTBI complicates decision-making. In case 1, vedolizumab was chosen for its gut-specific mechanism and low reactivation risk when slower onset of action was feasible. In case 2, infliximab was chosen for rapid effect in a severe flare after weighing LTBI reactivation risk and the patient’s refusal of surgery. These cases underscore the importance of balancing severity, onset of action, risk of disease progression, and reactivation of LTBI. While completion of LTBI therapy is ideal before biologic initiation, urgent clinical needs may justify after three weeks—or even concurrently—with ID involvement.
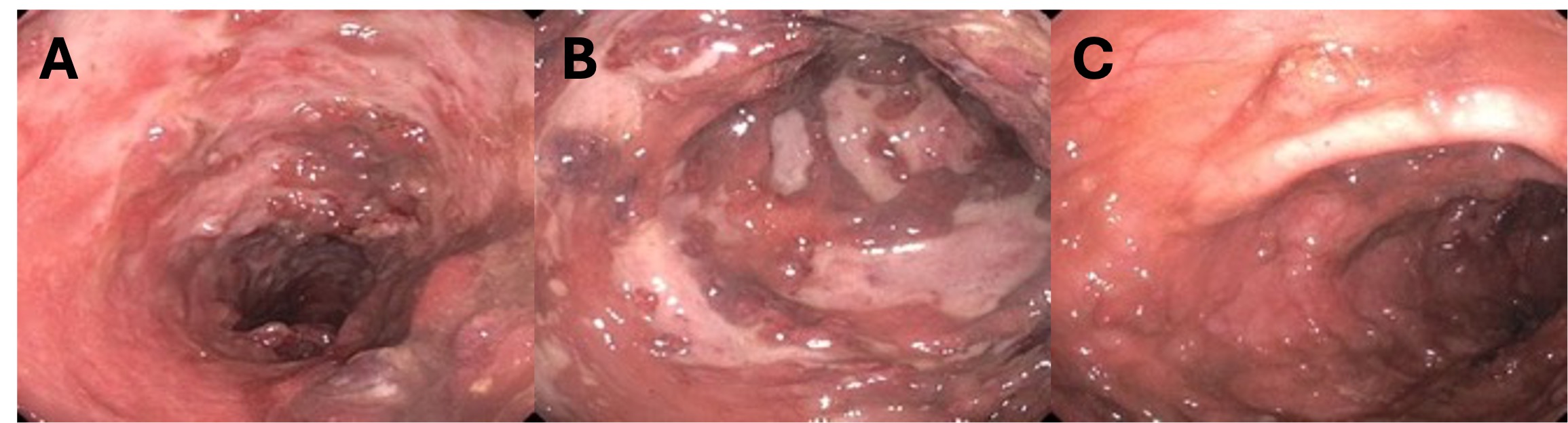
Figure: Figure 1. (A) Cecum, (B) Descending colon, and (C) Sigmoid colon.
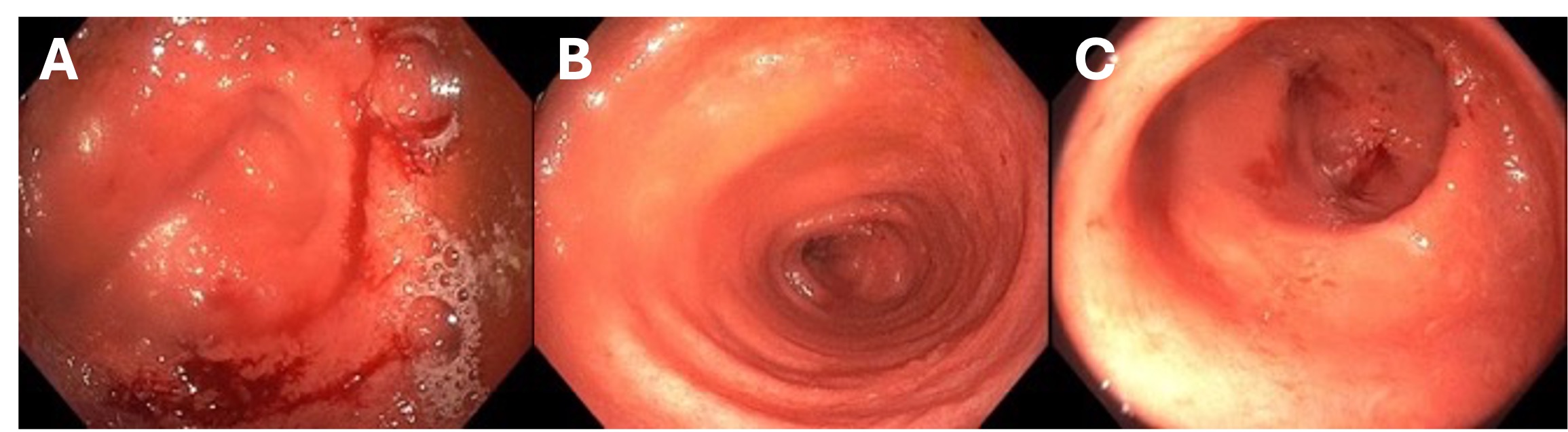
Figure: Figure 2. (A) Ascending colon, (B) Transverse colon, and (C) Descending colon.
Disclosures:
Zach Vinton indicated no relevant financial relationships.
Jason Barbaretta indicated no relevant financial relationships.
Nurlan Aliyev indicated no relevant financial relationships.
Kathryn Hutchins indicated no relevant financial relationships.
Zach Vinton, DO1, Jason Barbaretta, MD1, Nurlan Aliyev, MD2, Kathryn Hutchins, MD, FACG1. P3364 - Biologic Induction Therapy in Hospitalized Ulcerative Colitis With Latent Tuberculosis: A Case Series Emphasizing Individualized Care, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Nebraska Medical Center, Omaha, NE; 2University of Nebraska Medical Center, Elkhorn, NE
Introduction: Initiating biologic therapy in Ulcerative Colitis (UC) and latent tuberculosis infection (LTBI) increases risk of LTBI reactivation. This poses a clinical challenge, particularly when inpatient, where urgent induction is often necessary. We present two cases with UC flares and concurrent LTBI requiring biologic therapy following steroid-refractory disease.
Case Description/
Methods: Case 1: A 24-year-old female with UC with a two-month history of >15 bloody stools daily. LTBI was diagnosed during outpatient pre-biologic screening, and rifampin was started one month prior to admission per infectious disease (ID) recommendation. On admission, she was hypotensive and tachycardic with CRP of 1.9 mg/dL. CT revealed proctosigmoiditis, and colonoscopy demonstrated Mayo 2 (moderate) pancolitis (Figure 1) with chronic active colitis and negative CMV staining. After failing a 72-hour intravenous (IV) steroid trial, vedolizumab was initiated with ID guidance. Her symptoms and CRP improved, and she was discharged on a steroid taper with plans for outpatient vedolizumab maintenance.
Case 2: A 48-year-old male with UC presented with 8 days of >10 bloody stools daily with abdominal pain and intermittent fevers. He was tachycardic with elevated CRP (13.4 mg/dL). CT showed pancolitis and colonoscopy revealed Mayo 3 (severe) colitis in the right colon with Mayo 2 (moderate) colitis in the left (Figure 2). After failing a 72-hour IV steroid trial, pre-biologic screening revealed LTBI. A multidisciplinary team initiated infliximab alongside isoniazid and B6. He showed rapid clinical improvement and was discharged with outpatient infliximab therapy.
At 1 and 4 months, both patients were without clinical or radiological evidence of active tuberculosis.
Discussion: Although infliximab or cyclosporine are the standard treatment for hospitalized patients with acute severe UC unresponsive to IV steroids, the presence of LTBI complicates decision-making. In case 1, vedolizumab was chosen for its gut-specific mechanism and low reactivation risk when slower onset of action was feasible. In case 2, infliximab was chosen for rapid effect in a severe flare after weighing LTBI reactivation risk and the patient’s refusal of surgery. These cases underscore the importance of balancing severity, onset of action, risk of disease progression, and reactivation of LTBI. While completion of LTBI therapy is ideal before biologic initiation, urgent clinical needs may justify after three weeks—or even concurrently—with ID involvement.
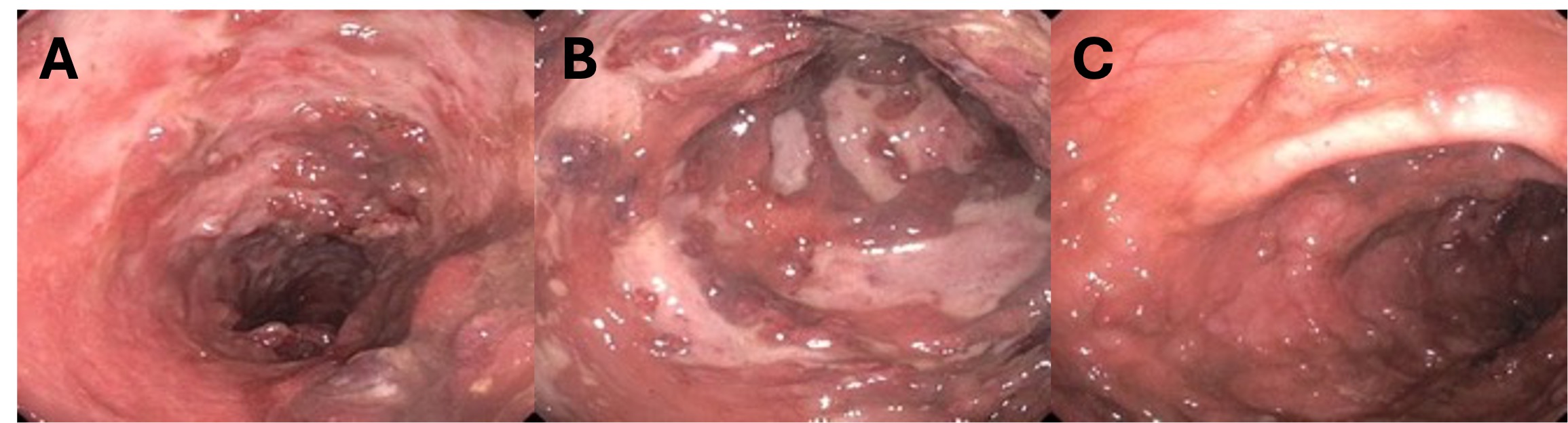
Figure: Figure 1. (A) Cecum, (B) Descending colon, and (C) Sigmoid colon.
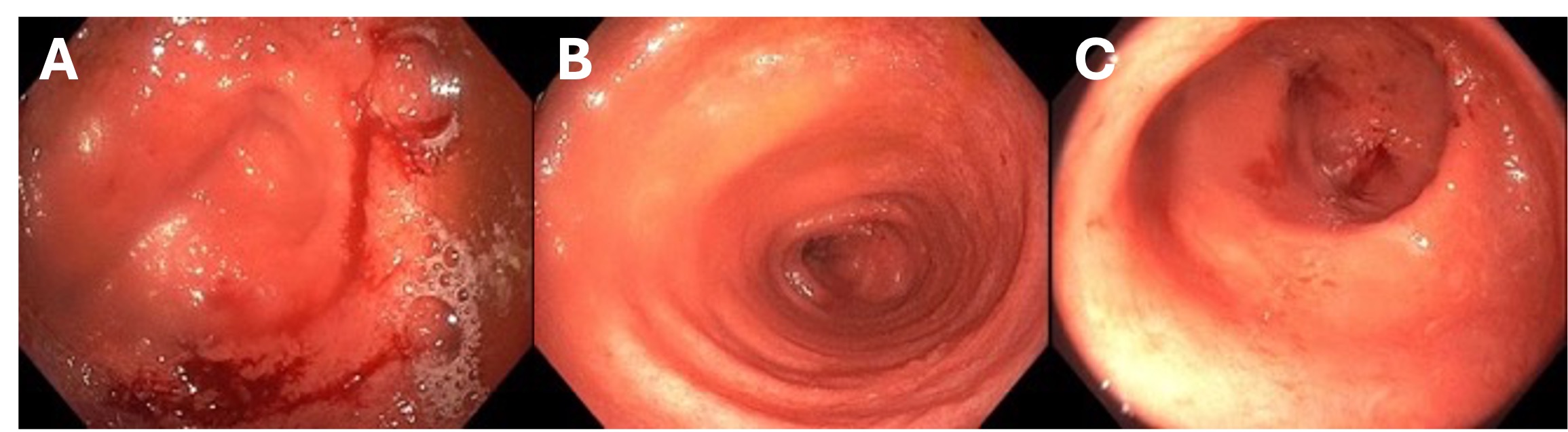
Figure: Figure 2. (A) Ascending colon, (B) Transverse colon, and (C) Descending colon.
Disclosures:
Zach Vinton indicated no relevant financial relationships.
Jason Barbaretta indicated no relevant financial relationships.
Nurlan Aliyev indicated no relevant financial relationships.
Kathryn Hutchins indicated no relevant financial relationships.
Zach Vinton, DO1, Jason Barbaretta, MD1, Nurlan Aliyev, MD2, Kathryn Hutchins, MD, FACG1. P3364 - Biologic Induction Therapy in Hospitalized Ulcerative Colitis With Latent Tuberculosis: A Case Series Emphasizing Individualized Care, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
