Monday Poster Session
Category: IBD
P3359 - Mistaken for Infection: Delayed Recognition of Pyoderma Gangrenosum in a Crohn’s Flare
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- ME
Marawan Elmassry, MD
Texas Tech University Health Sciences Center
Lubbock, TX
Presenting Author(s)
Marawan Elmassry, MD1, Mohammed Alhabil, MS1, Mohamad Altabaa, MS1, Musa Imam, MS1, Monia Baiomy, MBBCh1, Ahmed Shukri, MD1, Mohamed Mortagy, MBBCh2, Hakan Akin, MD1
1Texas Tech University Health Sciences Center, Lubbock, TX; 2Basingstoke and North Hampshire Hospital, Winchester, England, United Kingdom
Introduction: Pyoderma gangrenosum (PG) is a rare but severe neutrophilic dermatosis associated with inflammatory bowel disease (IBD). We present a case of PG triggered by a severe Crohn’s flare highlighting diagnostic challenges and management strategies.
Case Description/
Methods: A 19-year-old male with a history of Crohn’s disease, previously diagnosed as ulcerative colitis, presented with worsening bloody diarrhea and a painful, enlarging right thigh lesion and multiple smaller lesions in his bilateral lower extremities. His medical history was notable for perianal abscesses and fistulas. Home medications included azathioprine (1600 mg/day), mesalamine, and low-dose prednisone (5 mg daily).
On admission, he was febrile with leukocytosis (WBC 16.3 K/µL), CRP 24.8 mg/dL, ESR 77 mm/hr, and stool calprotectin >5040 µg/g. CT imaging revealed a left thigh fluid collection initially interpreted as an abscess. Colonoscopy demonstrated severe colitis with deep ulcerations, pseudopolyps, and a suspected colonic fistula. A transthoracic echocardiogram (TTE) showed no vegetations, and bacteremia was ruled out. Azathioprine was discontinued, and IV methylprednisolone (40 mg daily) was started for a severe Crohn’s flare.
General surgery was consulted early and performed multiple drainages of the thigh lesion, but the wound continued to enlarge and remained painful despite broad-spectrum antibiotics (cefepime and daptomycin). The lack of clinical improvement raised concern for pyoderma gangrenosum (PG), and prompted Dermatology consult. A punch biopsy confirmed PG. Dermatology recommended avoiding surgical debridment due to concern for pathergy.
The patient’s condition improved on IV steroids. He was discharged on a prednisone taper and later initiated on vedolizumab for maintenance IBD therapy. At 3-month follow-up, his skin lesions had nearly completely resolved.
Discussion: Pyoderma gangrenosum (PG) is a rare extraintestinal manifestation of IBD, affecting 1–2% of Crohn’s patients (Vallini et al., 2017). It is an autoinflammatory disorder driven by neutrophilic dysfunction, often misdiagnosed as infection due to painful ulcerations (Ruocco et al., 2012). Biopsy is essential to confirm PG and exclude mimics (Ahronowitz et al., 2012). Surgical debridement is contraindicated due to pathergy (Ahronowitz et al., 2012). Treatment includes corticosteroids, immunosuppressants, or biologics. In this case, steroids and vedolizumab led to near-complete resolution, highlighting the need for early diagnosis.
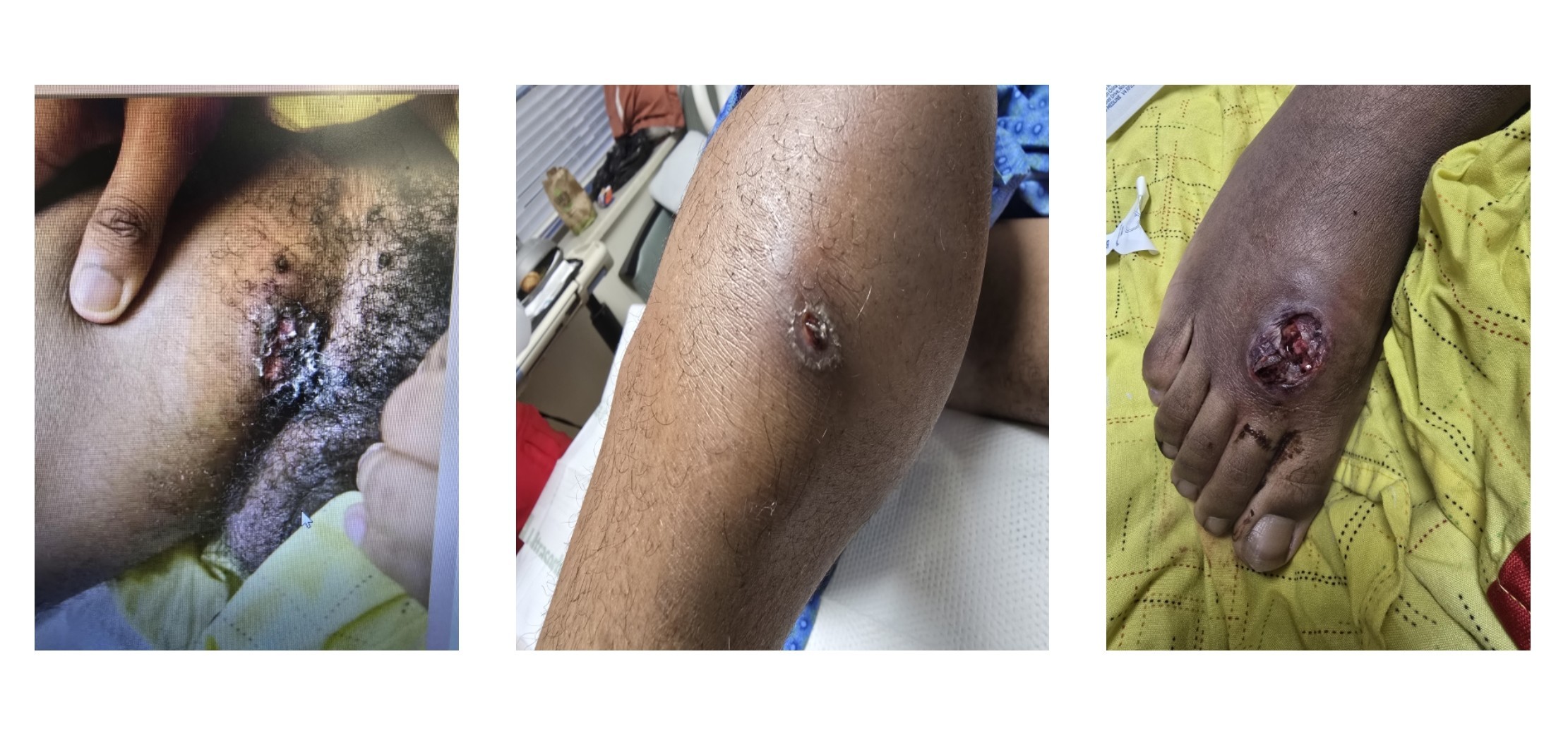
Figure: Pyoderma Gangrenosum Lesions
Disclosures:
Marawan Elmassry indicated no relevant financial relationships.
Mohammed Alhabil indicated no relevant financial relationships.
Mohamad Altabaa indicated no relevant financial relationships.
Musa Imam indicated no relevant financial relationships.
Monia Baiomy indicated no relevant financial relationships.
Ahmed Shukri indicated no relevant financial relationships.
Mohamed Mortagy indicated no relevant financial relationships.
Hakan Akin indicated no relevant financial relationships.
Marawan Elmassry, MD1, Mohammed Alhabil, MS1, Mohamad Altabaa, MS1, Musa Imam, MS1, Monia Baiomy, MBBCh1, Ahmed Shukri, MD1, Mohamed Mortagy, MBBCh2, Hakan Akin, MD1. P3359 - Mistaken for Infection: Delayed Recognition of Pyoderma Gangrenosum in a Crohn’s Flare, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Texas Tech University Health Sciences Center, Lubbock, TX; 2Basingstoke and North Hampshire Hospital, Winchester, England, United Kingdom
Introduction: Pyoderma gangrenosum (PG) is a rare but severe neutrophilic dermatosis associated with inflammatory bowel disease (IBD). We present a case of PG triggered by a severe Crohn’s flare highlighting diagnostic challenges and management strategies.
Case Description/
Methods: A 19-year-old male with a history of Crohn’s disease, previously diagnosed as ulcerative colitis, presented with worsening bloody diarrhea and a painful, enlarging right thigh lesion and multiple smaller lesions in his bilateral lower extremities. His medical history was notable for perianal abscesses and fistulas. Home medications included azathioprine (1600 mg/day), mesalamine, and low-dose prednisone (5 mg daily).
On admission, he was febrile with leukocytosis (WBC 16.3 K/µL), CRP 24.8 mg/dL, ESR 77 mm/hr, and stool calprotectin >5040 µg/g. CT imaging revealed a left thigh fluid collection initially interpreted as an abscess. Colonoscopy demonstrated severe colitis with deep ulcerations, pseudopolyps, and a suspected colonic fistula. A transthoracic echocardiogram (TTE) showed no vegetations, and bacteremia was ruled out. Azathioprine was discontinued, and IV methylprednisolone (40 mg daily) was started for a severe Crohn’s flare.
General surgery was consulted early and performed multiple drainages of the thigh lesion, but the wound continued to enlarge and remained painful despite broad-spectrum antibiotics (cefepime and daptomycin). The lack of clinical improvement raised concern for pyoderma gangrenosum (PG), and prompted Dermatology consult. A punch biopsy confirmed PG. Dermatology recommended avoiding surgical debridment due to concern for pathergy.
The patient’s condition improved on IV steroids. He was discharged on a prednisone taper and later initiated on vedolizumab for maintenance IBD therapy. At 3-month follow-up, his skin lesions had nearly completely resolved.
Discussion: Pyoderma gangrenosum (PG) is a rare extraintestinal manifestation of IBD, affecting 1–2% of Crohn’s patients (Vallini et al., 2017). It is an autoinflammatory disorder driven by neutrophilic dysfunction, often misdiagnosed as infection due to painful ulcerations (Ruocco et al., 2012). Biopsy is essential to confirm PG and exclude mimics (Ahronowitz et al., 2012). Surgical debridement is contraindicated due to pathergy (Ahronowitz et al., 2012). Treatment includes corticosteroids, immunosuppressants, or biologics. In this case, steroids and vedolizumab led to near-complete resolution, highlighting the need for early diagnosis.
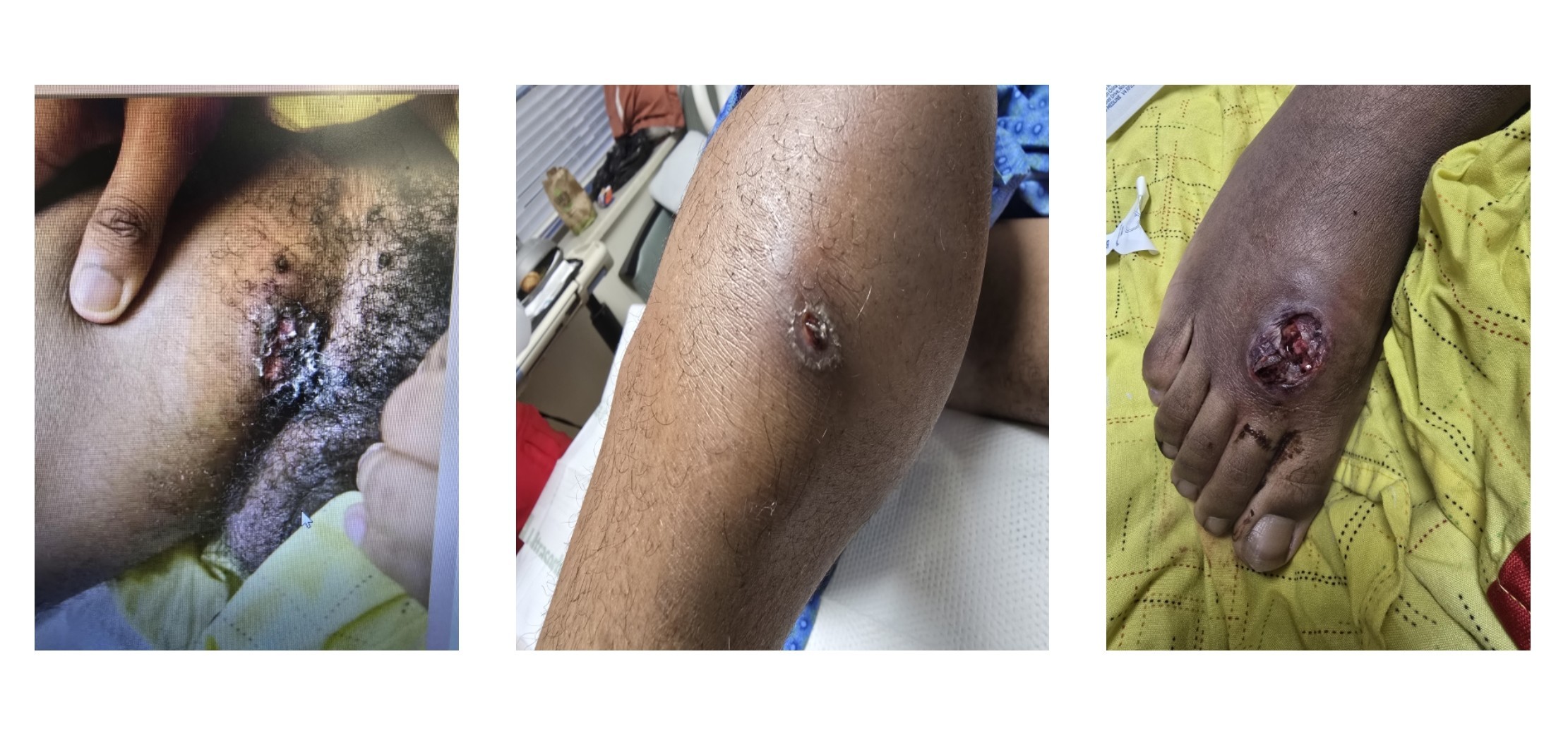
Figure: Pyoderma Gangrenosum Lesions
Disclosures:
Marawan Elmassry indicated no relevant financial relationships.
Mohammed Alhabil indicated no relevant financial relationships.
Mohamad Altabaa indicated no relevant financial relationships.
Musa Imam indicated no relevant financial relationships.
Monia Baiomy indicated no relevant financial relationships.
Ahmed Shukri indicated no relevant financial relationships.
Mohamed Mortagy indicated no relevant financial relationships.
Hakan Akin indicated no relevant financial relationships.
Marawan Elmassry, MD1, Mohammed Alhabil, MS1, Mohamad Altabaa, MS1, Musa Imam, MS1, Monia Baiomy, MBBCh1, Ahmed Shukri, MD1, Mohamed Mortagy, MBBCh2, Hakan Akin, MD1. P3359 - Mistaken for Infection: Delayed Recognition of Pyoderma Gangrenosum in a Crohn’s Flare, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
