Monday Poster Session
Category: IBD
P3349 - Evaluating the Effect of Coronary Artery Disease on Mortality and Discharge Disposition in Hospitalized Patients With Inflammatory Bowel Disease
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- MI
Mohamed Ismail, DO
Rutgers New Jersey Medical School
Astoria, NY
Presenting Author(s)
Mohamed Ismail, DO1, Menna-Allah Elaskandrany, DO2, Brian Kim, MD3, Michael Bebawy, DO1, Mahinaz Mohsen, MD1, Muhammad Hassaan Arif Maan, MBBS1, Weizheng Wang, MD1
1Rutgers New Jersey Medical School, Newark, NJ; 2Lenox Hill Hospital, Northwell Health, New York, NY; 3Rutgers New Jersey Medical School, Kearny, NJ
Introduction: Coronary artery disease (CAD) is an increasing comorbidity amongst patients with inflammatory bowel disease (IBD), due to the fact that the IBD population continues to age. While CAD is well recognized as a predictor of adverse cardiovascular outcomes, its impact on inpatient trajectories for patients with IBD remains insufficiently characterized. We aimed to assess the association between CAD and key hospitalization outcomes, including age at admission, discharge disposition, and in-hospital mortality, in a nationally representative cohort of patients with IBD.
Methods: We performed a cross-sectional analysis of 4,142,365 IBD-related hospitalizations using the National Inpatient Sample (NIS). Patients were stratified based on the presence or absence of CAD. Primary outcomes included routine discharge, transfer to a skilled nursing facility (SNF) or other institution, home health care (HHC) utilization, discharge against medical advice (AMA), and in-hospital mortality. Differences between groups were compared using Chi-square tests, with a two-tailed p < 0.001 considered statistically significant.
Results: CAD was identified in 842,658 (20.3%) of IBD hospitalizations. Compared to patients without CAD (n = 3,299,707), patients with CAD were less likely to be discharged to home (45.0% vs. 58.8%, p < 0.001) and more likely to be discharged to SNFs or other facilities (26.8% vs. 19.1%, p < 0.001), require HHC (21.9% vs. 16.5%, p < 0.001), or die in-hospital (3.2% vs. 2.4%, p < 0.001). Interestingly, discharge AMA was observed less frequently in patients with CAD (0.7% vs. 1.2%, p < 0.001).
Discussion: Coexisting CAD among hospitalized patients with IBD is associated with significantly worse outcomes, including a 33% relative increase in in-hospital mortality and greater post-acute care utilization. These findings highlight the clinical burden of cardiovascular comorbidity in IBD. The lower rate of discharge AMA in the CAD group may reflect more severe illness or better recognition of care needs, emphasizing the importance of individualized discharge planning. These results support the integration of routine cardiovascular screening and multidisciplinary coordination into IBD care. Future studies should evaluate whether incorporation of cardiovascular assessment can improve outcomes in high-risk populations such as those with IBD.
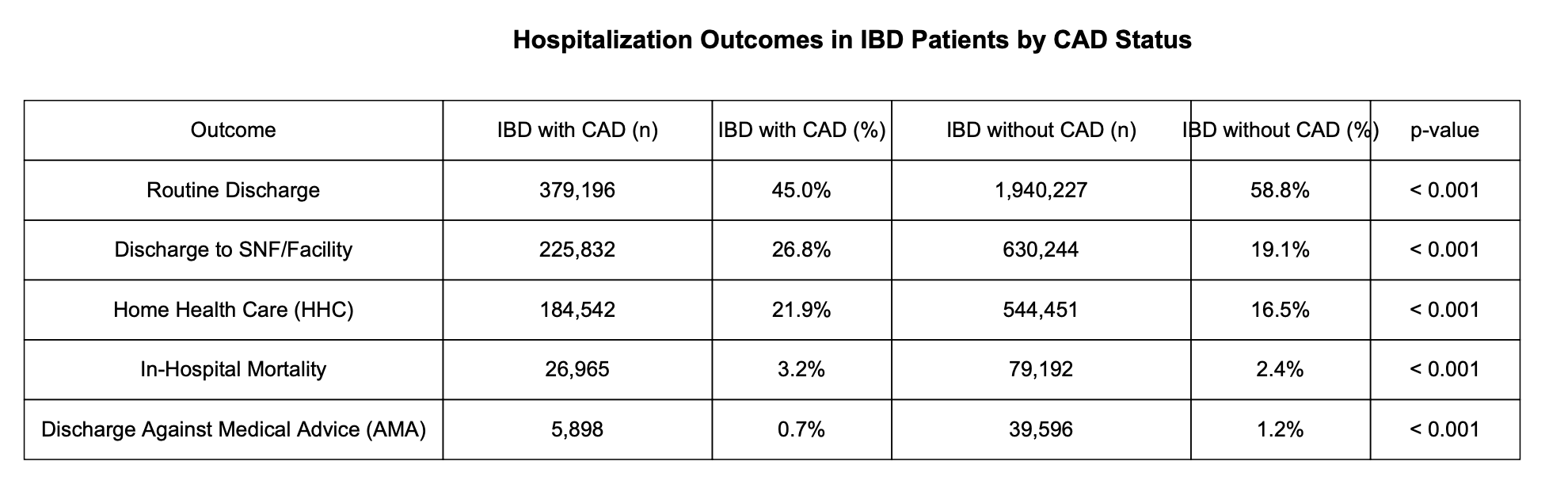
Figure: Comparison of Hospitalization Outcomes in IBD Patients With vs. Without CAD
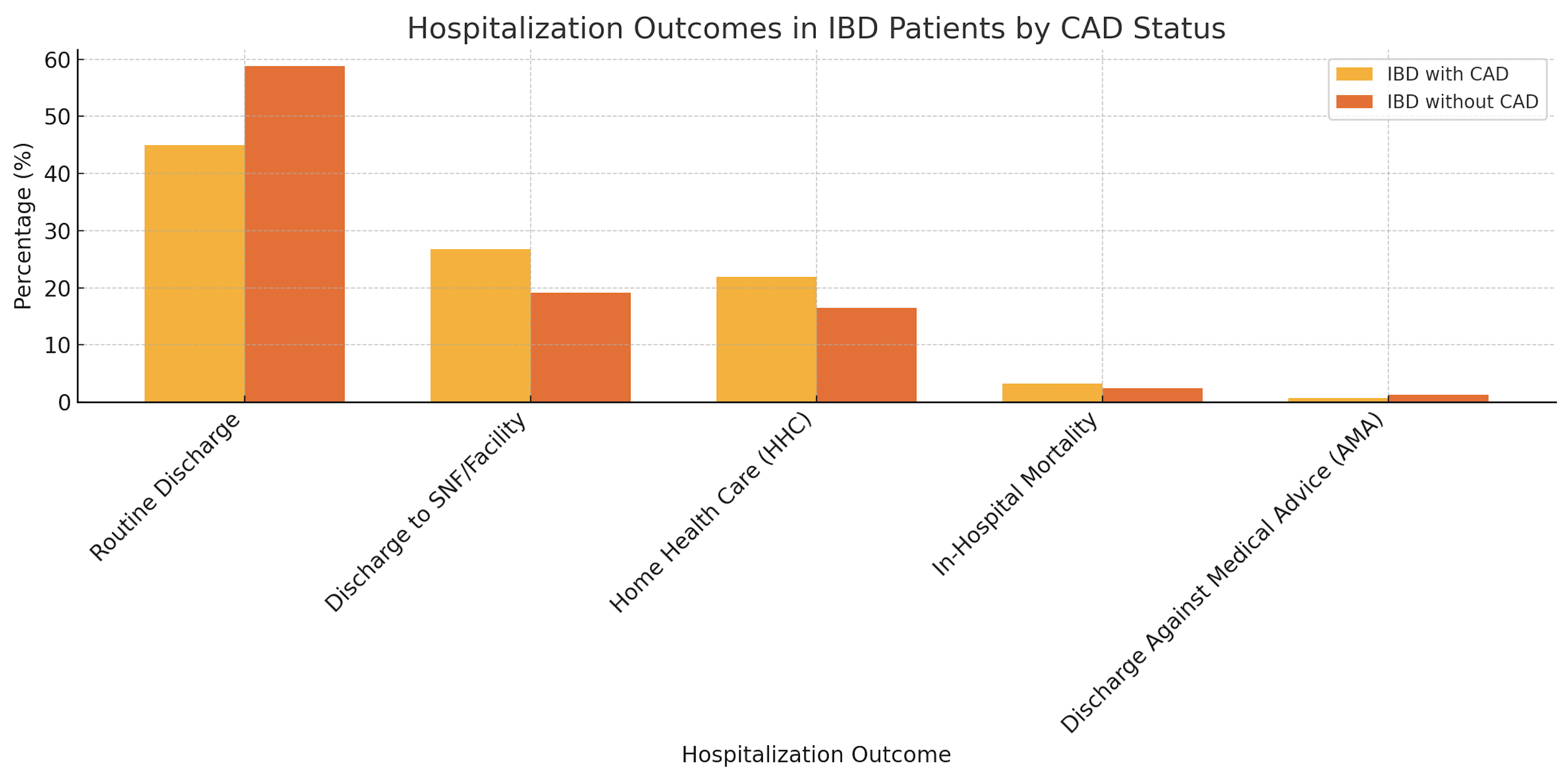
Figure: Comparison of Hospitalization Outcomes in IBD Patients With vs. Without CAD
Disclosures:
Mohamed Ismail indicated no relevant financial relationships.
Menna-Allah Elaskandrany indicated no relevant financial relationships.
Brian Kim indicated no relevant financial relationships.
Michael Bebawy indicated no relevant financial relationships.
Mahinaz Mohsen indicated no relevant financial relationships.
Muhammad Hassaan Arif Maan indicated no relevant financial relationships.
Weizheng Wang indicated no relevant financial relationships.
Mohamed Ismail, DO1, Menna-Allah Elaskandrany, DO2, Brian Kim, MD3, Michael Bebawy, DO1, Mahinaz Mohsen, MD1, Muhammad Hassaan Arif Maan, MBBS1, Weizheng Wang, MD1. P3349 - Evaluating the Effect of Coronary Artery Disease on Mortality and Discharge Disposition in Hospitalized Patients With Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Rutgers New Jersey Medical School, Newark, NJ; 2Lenox Hill Hospital, Northwell Health, New York, NY; 3Rutgers New Jersey Medical School, Kearny, NJ
Introduction: Coronary artery disease (CAD) is an increasing comorbidity amongst patients with inflammatory bowel disease (IBD), due to the fact that the IBD population continues to age. While CAD is well recognized as a predictor of adverse cardiovascular outcomes, its impact on inpatient trajectories for patients with IBD remains insufficiently characterized. We aimed to assess the association between CAD and key hospitalization outcomes, including age at admission, discharge disposition, and in-hospital mortality, in a nationally representative cohort of patients with IBD.
Methods: We performed a cross-sectional analysis of 4,142,365 IBD-related hospitalizations using the National Inpatient Sample (NIS). Patients were stratified based on the presence or absence of CAD. Primary outcomes included routine discharge, transfer to a skilled nursing facility (SNF) or other institution, home health care (HHC) utilization, discharge against medical advice (AMA), and in-hospital mortality. Differences between groups were compared using Chi-square tests, with a two-tailed p < 0.001 considered statistically significant.
Results: CAD was identified in 842,658 (20.3%) of IBD hospitalizations. Compared to patients without CAD (n = 3,299,707), patients with CAD were less likely to be discharged to home (45.0% vs. 58.8%, p < 0.001) and more likely to be discharged to SNFs or other facilities (26.8% vs. 19.1%, p < 0.001), require HHC (21.9% vs. 16.5%, p < 0.001), or die in-hospital (3.2% vs. 2.4%, p < 0.001). Interestingly, discharge AMA was observed less frequently in patients with CAD (0.7% vs. 1.2%, p < 0.001).
Discussion: Coexisting CAD among hospitalized patients with IBD is associated with significantly worse outcomes, including a 33% relative increase in in-hospital mortality and greater post-acute care utilization. These findings highlight the clinical burden of cardiovascular comorbidity in IBD. The lower rate of discharge AMA in the CAD group may reflect more severe illness or better recognition of care needs, emphasizing the importance of individualized discharge planning. These results support the integration of routine cardiovascular screening and multidisciplinary coordination into IBD care. Future studies should evaluate whether incorporation of cardiovascular assessment can improve outcomes in high-risk populations such as those with IBD.
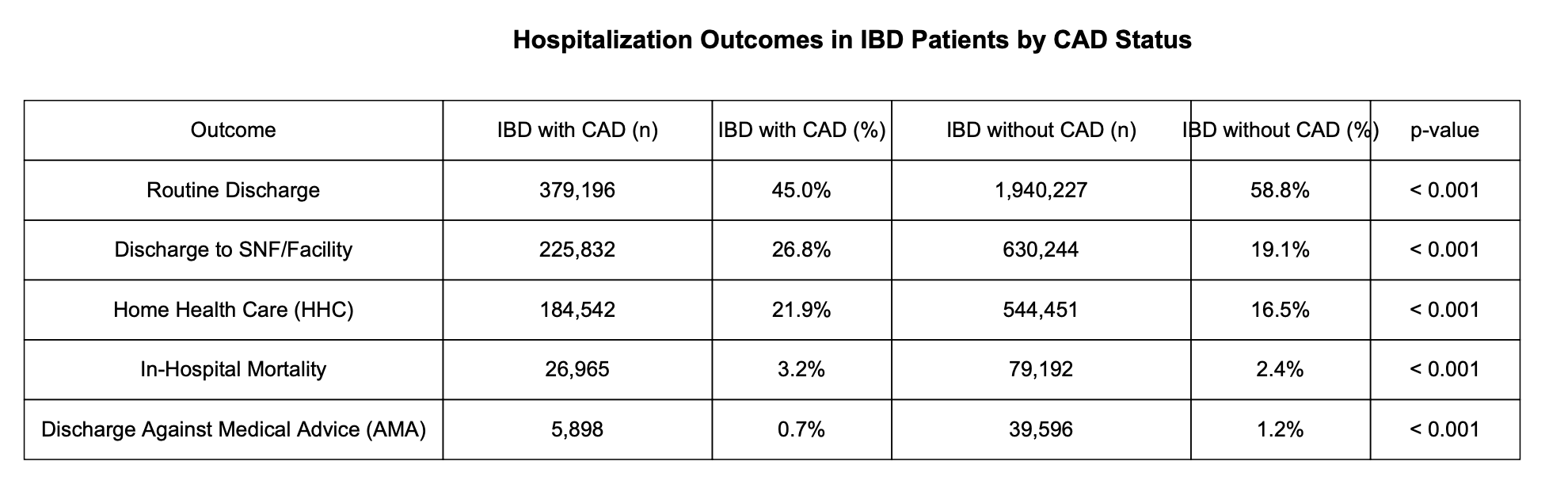
Figure: Comparison of Hospitalization Outcomes in IBD Patients With vs. Without CAD
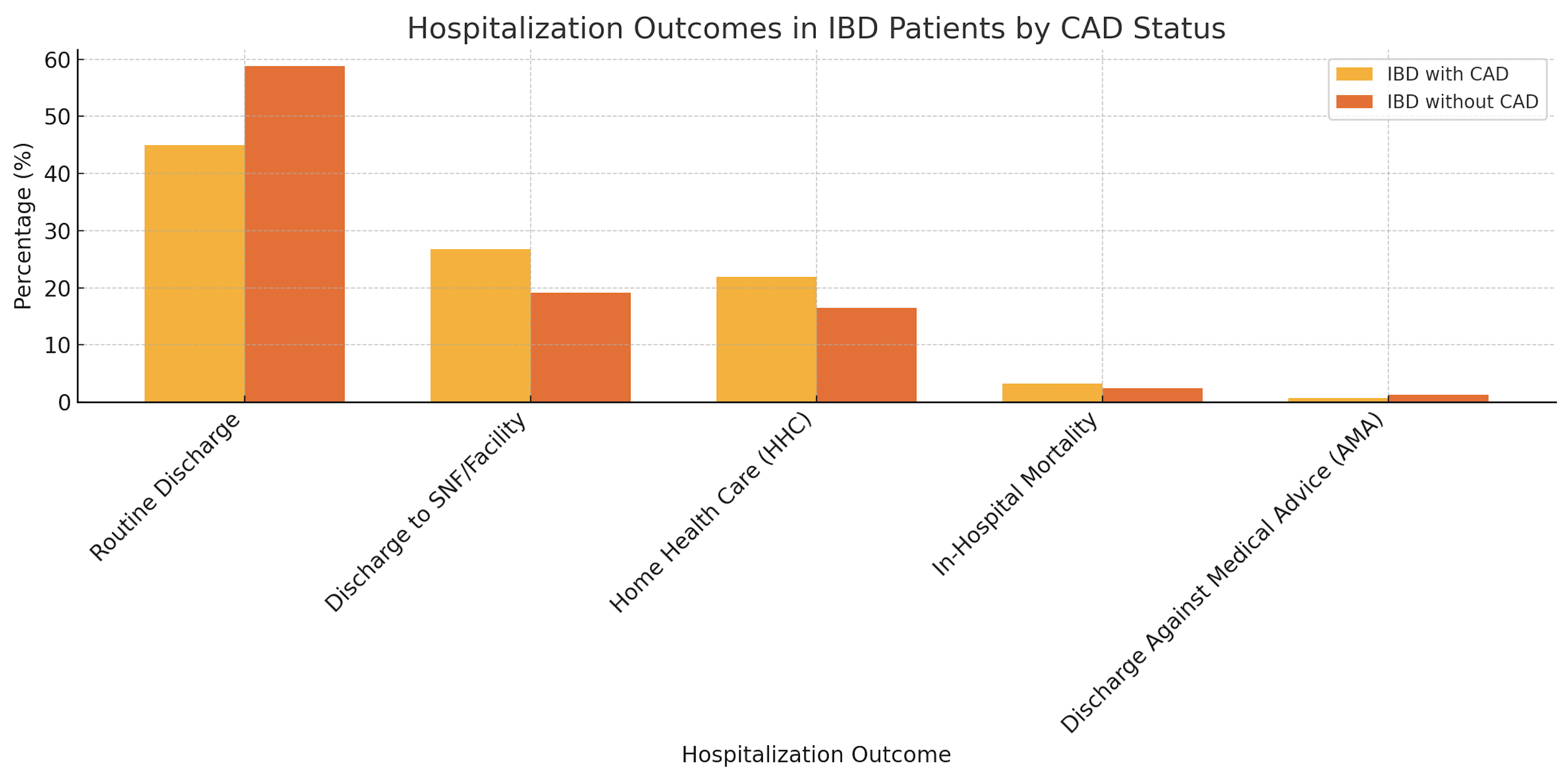
Figure: Comparison of Hospitalization Outcomes in IBD Patients With vs. Without CAD
Disclosures:
Mohamed Ismail indicated no relevant financial relationships.
Menna-Allah Elaskandrany indicated no relevant financial relationships.
Brian Kim indicated no relevant financial relationships.
Michael Bebawy indicated no relevant financial relationships.
Mahinaz Mohsen indicated no relevant financial relationships.
Muhammad Hassaan Arif Maan indicated no relevant financial relationships.
Weizheng Wang indicated no relevant financial relationships.
Mohamed Ismail, DO1, Menna-Allah Elaskandrany, DO2, Brian Kim, MD3, Michael Bebawy, DO1, Mahinaz Mohsen, MD1, Muhammad Hassaan Arif Maan, MBBS1, Weizheng Wang, MD1. P3349 - Evaluating the Effect of Coronary Artery Disease on Mortality and Discharge Disposition in Hospitalized Patients With Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
