Monday Poster Session
Category: IBD
P3404 - Infliximab-Induced Medium Vessel Vasculitis in a Patient Treated for Ulcerative Colitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Evelyn Inga, MD
University of New Mexico Health Sciences Center
Albuquerque, NM
Presenting Author(s)
Evelyn Inga, MD1, Swathi Paleti, MD1, Hareesh K. Gundlapalli, MD2
1University of New Mexico Health Sciences Center, Albuquerque, NM; 2University of New Mexico, Albuquerque, NM
Introduction: Anti-tumor necrosis factor (anti-TNF) therapies like infliximab have established efficacy for treatment of ulcerative colitis (UC); yet rare complications such as vasculitis are noted. Cases often resolve after drug discontinuation and immunosuppressive therapy. We present a 68 yo male with UC who developed medium vessel vasculitis after long-term infliximab use, highlighting diagnostic
challenges and management strategies
Case Description/
Methods: A 68-year-old male with left-sided UC, has been uneventfully managed with infliximab for a decade. He presented to the ED with 3 days of mid-abdominal pain, bloating, fever, chills, nausea, dry heaving, and SOB, and no BM for 3 days. Physical exam showed a tender left lower quadrant. Vital signs and labs were within normal limits. CT of the abdomen/pelvis suggested left pyelonephritis,
prompting admission, Ceftriaxone, IV fluids, and analgesics. By day 5 of admission, the patient experienced worsening pain and a hemoglobin drop to 6.6 g/dL. This prompted repeat imaging and transfusion. CT revealed a 9-10 cm extraluminal hematoma abutting/compressing the ascending. The patient underwent interventional angiography, which identified ongoing bleeding from a
branch of the ileocolic artery and was successfully embolized. Irregular vessels were noted, primarily involving the middle colic artery, as well as the distal branches of the ileocolic artery. These findings suggest segmental arterial medial lysis or vasculitis. Repeat CT angiogram conducted due to new right upper quadrant pain revealed multiple medium vessel aneurysms and stenosis, raising concerns for Polyarteritis Nodosa (PAN), along with signs of ischemic colitis. An autoimmune workup showed ANA 1:640, anti-RNP 1.7, negative ANCA, and positive IgG beta-2 glycoprotein 1 antibodies, which supported a diagnosis of vasculitis. Infliximab was discontinued due to suspected, though rare, drug- induced vasculitis. The patient received IV then PO steroids and his infliximab was switched to upadacitinib (Rinvoq). At 2-month follow-up, the patient had stable hemoglobin and no further imaging findings of vasculitis
Discussion: This case highlights the rare association between long-term infliximab use and medium vessel vasculitis. Early recognition and prompt intervention, including drug discontinuation and immunosuppressive therapy, are crucial. Given the severity of vasculitis, clinicians should maintain a high index of suspicion in biologic-treated UC patients presenting with systemic or ischemic symptoms.
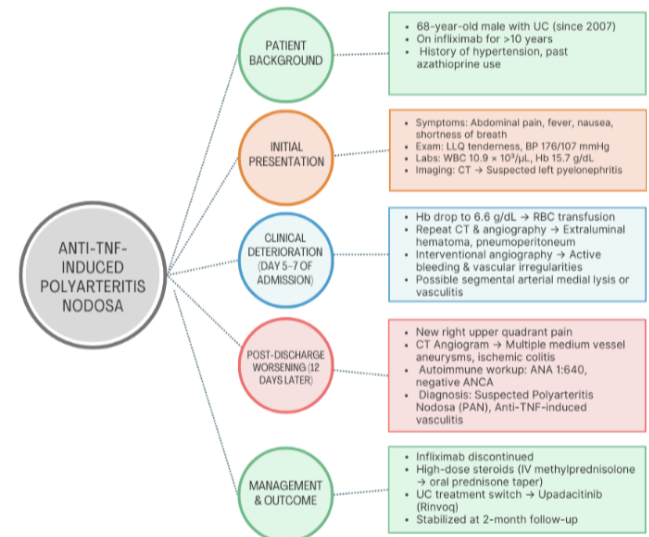
Figure: Case in Chart Format
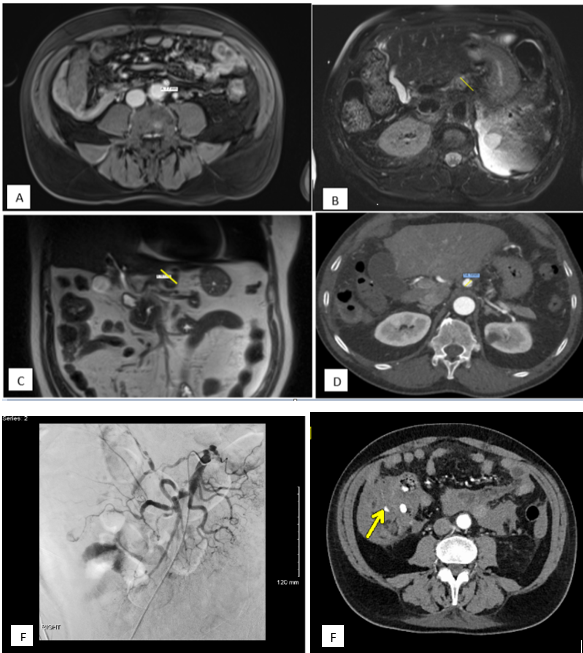
Figure: Aneurysmal Dilations of Intra-Abdominal Vasculature:
A) Dilated Inferior Mesenteric Artery (IMA) to 7.7 (Normal 3-5 mm)
B) Dilated Left Gastric Artery to 9 mm (Normal 3-5 mm)
C) Repeat Imaging with further dilation of Left Gastric Artery to 18 mm
D) Aneurysm of the Common Hepatic Artery to 14 mm (Normal 5-6 mm)
E) Angiogram with superior mesenteric arteriogram showing highly irregular vessels, mainly the middle colic artery as well the distal branches of the ileocolic artery and some branches to the ileum. Active hemorrhage was seen from a very distal branch of the ileal colic artery which was embolized.
F) CT Angiogram repeated and arterial phase showed bleeding in the soft tissue just lateral to and abutting the ascending colon. No bleeding in the portal venous phase and delayed phase.
Disclosures:
Evelyn Inga indicated no relevant financial relationships.
Swathi Paleti indicated no relevant financial relationships.
Hareesh Gundlapalli indicated no relevant financial relationships.
Evelyn Inga, MD1, Swathi Paleti, MD1, Hareesh K. Gundlapalli, MD2. P3404 - Infliximab-Induced Medium Vessel Vasculitis in a Patient Treated for Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of New Mexico Health Sciences Center, Albuquerque, NM; 2University of New Mexico, Albuquerque, NM
Introduction: Anti-tumor necrosis factor (anti-TNF) therapies like infliximab have established efficacy for treatment of ulcerative colitis (UC); yet rare complications such as vasculitis are noted. Cases often resolve after drug discontinuation and immunosuppressive therapy. We present a 68 yo male with UC who developed medium vessel vasculitis after long-term infliximab use, highlighting diagnostic
challenges and management strategies
Case Description/
Methods: A 68-year-old male with left-sided UC, has been uneventfully managed with infliximab for a decade. He presented to the ED with 3 days of mid-abdominal pain, bloating, fever, chills, nausea, dry heaving, and SOB, and no BM for 3 days. Physical exam showed a tender left lower quadrant. Vital signs and labs were within normal limits. CT of the abdomen/pelvis suggested left pyelonephritis,
prompting admission, Ceftriaxone, IV fluids, and analgesics. By day 5 of admission, the patient experienced worsening pain and a hemoglobin drop to 6.6 g/dL. This prompted repeat imaging and transfusion. CT revealed a 9-10 cm extraluminal hematoma abutting/compressing the ascending. The patient underwent interventional angiography, which identified ongoing bleeding from a
branch of the ileocolic artery and was successfully embolized. Irregular vessels were noted, primarily involving the middle colic artery, as well as the distal branches of the ileocolic artery. These findings suggest segmental arterial medial lysis or vasculitis. Repeat CT angiogram conducted due to new right upper quadrant pain revealed multiple medium vessel aneurysms and stenosis, raising concerns for Polyarteritis Nodosa (PAN), along with signs of ischemic colitis. An autoimmune workup showed ANA 1:640, anti-RNP 1.7, negative ANCA, and positive IgG beta-2 glycoprotein 1 antibodies, which supported a diagnosis of vasculitis. Infliximab was discontinued due to suspected, though rare, drug- induced vasculitis. The patient received IV then PO steroids and his infliximab was switched to upadacitinib (Rinvoq). At 2-month follow-up, the patient had stable hemoglobin and no further imaging findings of vasculitis
Discussion: This case highlights the rare association between long-term infliximab use and medium vessel vasculitis. Early recognition and prompt intervention, including drug discontinuation and immunosuppressive therapy, are crucial. Given the severity of vasculitis, clinicians should maintain a high index of suspicion in biologic-treated UC patients presenting with systemic or ischemic symptoms.
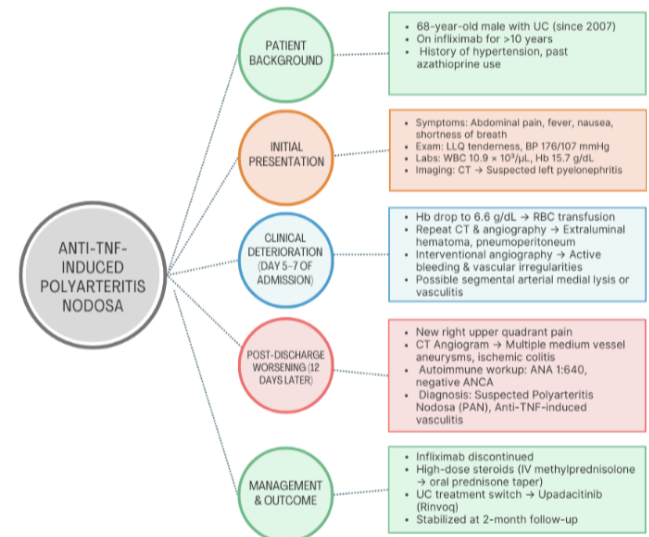
Figure: Case in Chart Format
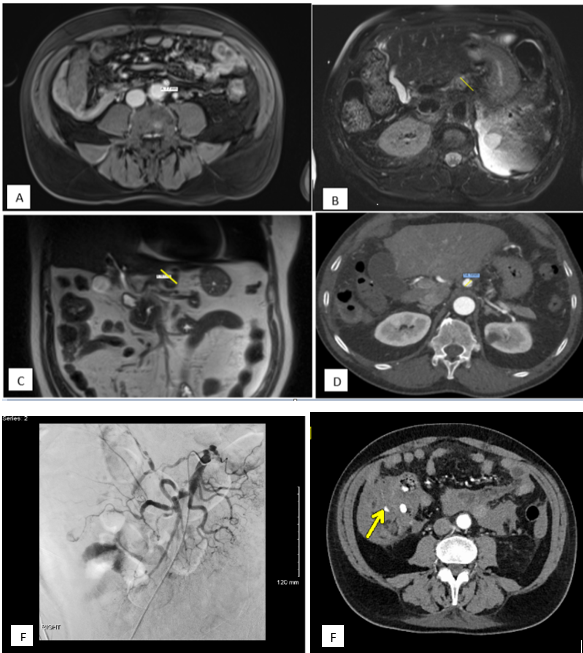
Figure: Aneurysmal Dilations of Intra-Abdominal Vasculature:
A) Dilated Inferior Mesenteric Artery (IMA) to 7.7 (Normal 3-5 mm)
B) Dilated Left Gastric Artery to 9 mm (Normal 3-5 mm)
C) Repeat Imaging with further dilation of Left Gastric Artery to 18 mm
D) Aneurysm of the Common Hepatic Artery to 14 mm (Normal 5-6 mm)
E) Angiogram with superior mesenteric arteriogram showing highly irregular vessels, mainly the middle colic artery as well the distal branches of the ileocolic artery and some branches to the ileum. Active hemorrhage was seen from a very distal branch of the ileal colic artery which was embolized.
F) CT Angiogram repeated and arterial phase showed bleeding in the soft tissue just lateral to and abutting the ascending colon. No bleeding in the portal venous phase and delayed phase.
Disclosures:
Evelyn Inga indicated no relevant financial relationships.
Swathi Paleti indicated no relevant financial relationships.
Hareesh Gundlapalli indicated no relevant financial relationships.
Evelyn Inga, MD1, Swathi Paleti, MD1, Hareesh K. Gundlapalli, MD2. P3404 - Infliximab-Induced Medium Vessel Vasculitis in a Patient Treated for Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
