Monday Poster Session
Category: Infections and Microbiome
P3493 - Persistent Pyrexia and Hepatic Abscess in a Non-Endemic Region: A Rare Case of Amebic Liver Abscess Due to Entamoeba Histolytica
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Rajan Patel, BA (he/him/his)
Geisinger Commonwealth School of Medicine
Danville, PA
Presenting Author(s)
Rajan Patel, BA1, Shriraj Patel, DO2, Darrell Mcbride, DO2
1Geisinger Commonwealth School of Medicine, Danville, PA; 2Geisinger Medical Center, Danville, PA
Introduction: E. Histolytica is an enteric protozoan that causes amebic dysentery in underdeveloped tropical regions. It is typically acquired by ingestion of contaminated water or sexual oral-anal contact. It can spread beyond the intestinal lumen to the liver and result in amebic liver abscess (ALA). Patients typically present with right upper quadrant (RUQ) abdominal pain and fever. While endemic to other regions, E. histolytica is exceedingly rare in the United States with an incidence of 1.38 per million population. We present the rare case of E. Histolytica ALA in a middle-aged male, without international travel history, in rural Pennsylvania (PA).
Case Description/
Methods: A 45-year-old male who has sex with men (MSM), and well-controlled HIV on antiretroviral therapy, presented with RUQ abdominal pain and a fever of 38.1℃. Initial labs noted elevated alkaline phosphatase (256 U/L). Due to a contrast allergy, a non-contrast abdominal computed tomography (CT) scan was obtained, revealing a 5.4 x 6.4 x 4.5 cm mass (Figure 1) in the right posterior hepatic lobe. He was admitted and started on piperacillin-tazobactam. The abscess was drained with aspirate sent for culture. Blood cultures, acid-fast bacilli, Bartonella, and Q-fever serologies returned negative, but fevers persisted over 38.5 °C. A repeat non-contrast CT (Figure 2) the next day revealed unchanged abscess size but increased loculations, prompting escalation to Meropenem. E. histolytica serology ultimately resulted positive on day 15. Antibiotics were transitioned to a ten-day course of metronidazole and a seven-day course of paromomycin.
Discussion: ALA is a common extraintestinal manifestation of Entamoeba histolytica infection. It is endemic to tropical regions and exceedingly rare in the United States, especially in rural PA. This case highlights a diagnostic challenge posed by ALA in non-endemic regions, where it may be misdiagnosed as pyogenic liver abscess. ALA should be considered in at-risk populations, particularly MSM and immunocompromised individuals, regardless of travel history. The diagnostic delay in this case highlights the limited specificity of imaging in distinguishing between pyogenic amebic abscesses. Moreover, a broad differential diagnosis is essential in patients with persistent, unexplained fevers and hepatic lesions. Clinicians should maintain a high index of suspicion for E. histolytica in an appropriate clinical context, as untreated cases may progress to abscess rupture or systemic dissemination.
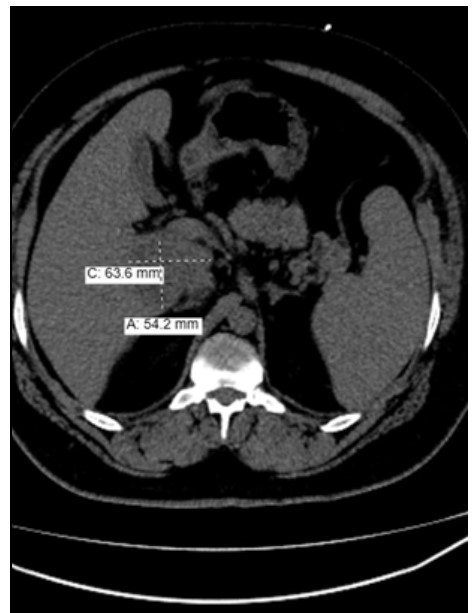
Figure: Figure 1: Axial view of a non-contrast CT demonstrating an ill-defined, indeterminate hypodense lesion measuring 5.4 x 6.4 x 4.5 cm in the posterior segment of the right hepatic lobe.
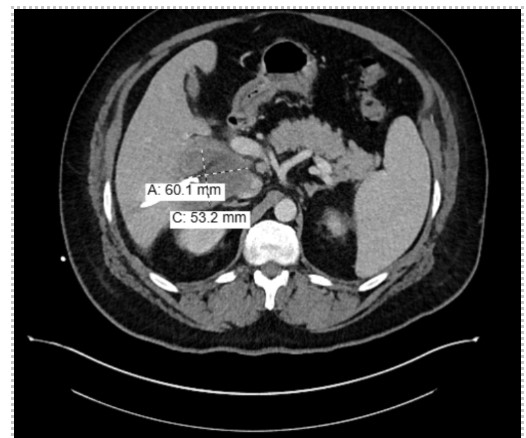
Figure: Figure 2: Axial view of a non-contrast CT obtained on Day 7 of admission showing relatively unchanged size of ill-defined hypodense lesion in right posterior hepatic lobe with increased loculations.
Disclosures:
Rajan Patel indicated no relevant financial relationships.
Shriraj Patel indicated no relevant financial relationships.
Darrell Mcbride indicated no relevant financial relationships.
Rajan Patel, BA1, Shriraj Patel, DO2, Darrell Mcbride, DO2. P3493 - Persistent Pyrexia and Hepatic Abscess in a Non-Endemic Region: A Rare Case of Amebic Liver Abscess Due to Entamoeba Histolytica, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Geisinger Commonwealth School of Medicine, Danville, PA; 2Geisinger Medical Center, Danville, PA
Introduction: E. Histolytica is an enteric protozoan that causes amebic dysentery in underdeveloped tropical regions. It is typically acquired by ingestion of contaminated water or sexual oral-anal contact. It can spread beyond the intestinal lumen to the liver and result in amebic liver abscess (ALA). Patients typically present with right upper quadrant (RUQ) abdominal pain and fever. While endemic to other regions, E. histolytica is exceedingly rare in the United States with an incidence of 1.38 per million population. We present the rare case of E. Histolytica ALA in a middle-aged male, without international travel history, in rural Pennsylvania (PA).
Case Description/
Methods: A 45-year-old male who has sex with men (MSM), and well-controlled HIV on antiretroviral therapy, presented with RUQ abdominal pain and a fever of 38.1℃. Initial labs noted elevated alkaline phosphatase (256 U/L). Due to a contrast allergy, a non-contrast abdominal computed tomography (CT) scan was obtained, revealing a 5.4 x 6.4 x 4.5 cm mass (Figure 1) in the right posterior hepatic lobe. He was admitted and started on piperacillin-tazobactam. The abscess was drained with aspirate sent for culture. Blood cultures, acid-fast bacilli, Bartonella, and Q-fever serologies returned negative, but fevers persisted over 38.5 °C. A repeat non-contrast CT (Figure 2) the next day revealed unchanged abscess size but increased loculations, prompting escalation to Meropenem. E. histolytica serology ultimately resulted positive on day 15. Antibiotics were transitioned to a ten-day course of metronidazole and a seven-day course of paromomycin.
Discussion: ALA is a common extraintestinal manifestation of Entamoeba histolytica infection. It is endemic to tropical regions and exceedingly rare in the United States, especially in rural PA. This case highlights a diagnostic challenge posed by ALA in non-endemic regions, where it may be misdiagnosed as pyogenic liver abscess. ALA should be considered in at-risk populations, particularly MSM and immunocompromised individuals, regardless of travel history. The diagnostic delay in this case highlights the limited specificity of imaging in distinguishing between pyogenic amebic abscesses. Moreover, a broad differential diagnosis is essential in patients with persistent, unexplained fevers and hepatic lesions. Clinicians should maintain a high index of suspicion for E. histolytica in an appropriate clinical context, as untreated cases may progress to abscess rupture or systemic dissemination.
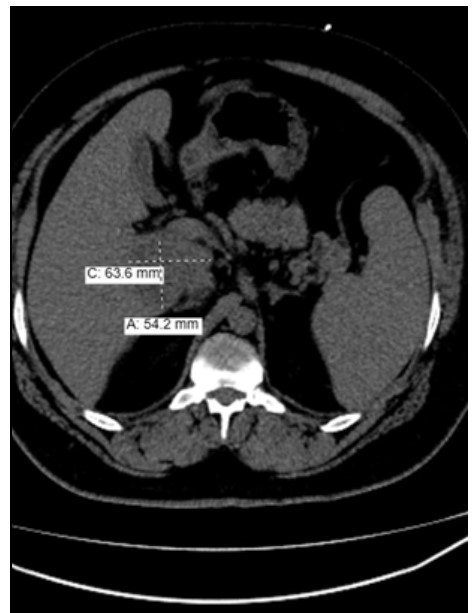
Figure: Figure 1: Axial view of a non-contrast CT demonstrating an ill-defined, indeterminate hypodense lesion measuring 5.4 x 6.4 x 4.5 cm in the posterior segment of the right hepatic lobe.
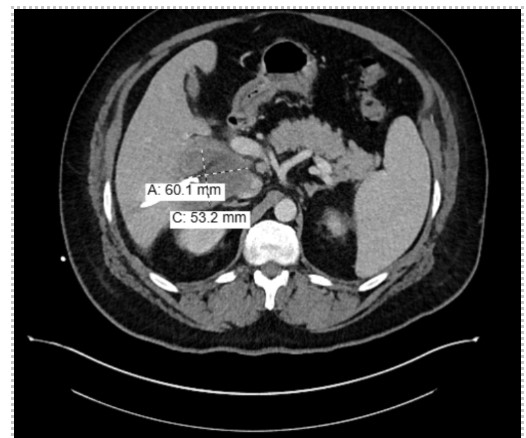
Figure: Figure 2: Axial view of a non-contrast CT obtained on Day 7 of admission showing relatively unchanged size of ill-defined hypodense lesion in right posterior hepatic lobe with increased loculations.
Disclosures:
Rajan Patel indicated no relevant financial relationships.
Shriraj Patel indicated no relevant financial relationships.
Darrell Mcbride indicated no relevant financial relationships.
Rajan Patel, BA1, Shriraj Patel, DO2, Darrell Mcbride, DO2. P3493 - Persistent Pyrexia and Hepatic Abscess in a Non-Endemic Region: A Rare Case of Amebic Liver Abscess Due to Entamoeba Histolytica, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

