Monday Poster Session
Category: Infections and Microbiome
A Rare Case of Spondylodiscitis Due to <i>Actinotignum schaalii</i> In a Patient With Crohn’s Disease
P3488 - A Rare Case of Spondylodiscitis Due to Actinotignum schaalii in a Patient With Crohn’s Disease
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Austin Tiesenga, DO
Corewell Health Lakeland
St. Joseph, MI
Presenting Author(s)
Austin Tiesenga, DO1, Thomas Birris, MD2, William Schreiner, MD1, David Malaka, MD1, Rafeek Woods, MD1, Michael Wang, MD1
1Corewell Health Lakeland, St. Joseph, MI; 2Corewell Health Lakeland, Saint Joseph, MI
Introduction: Patients with Crohn’s disease have an increased risk for infectious spondylodiscitis, particularly in the presence of GI fistula formation. Patients with inflammatory bowel disease (IBD) can also develop autoimmune causes of spondyloarthritis, including HLA-B27 related disease, which can complicate identifying the underlying etiology of spondylodiscitis. We report a rare case of spondylodiscitis secondary to Actinotignum schaalii, an uncommon urinary pathogen, in a patient with a history of Crohn’s disease and previous exposure to infliximab therapy.
Case Description/
Methods: We present a 55 year old male with a PMH of Crohn’s disease with a prior exposure to infliximab, degenerative disc disease, and chronic urinary retention, who presented for worsening back pain. He was treated for a UTI two days prior to admission with ciprofloxacin. He denied fever, chills, dysuria, frequency, urgency, numbness, weakness bilateral lower extremities, and saddle anesthesia. The MRI lumbar spine/sacrum revealed bone marrow edema within L2/L3, suspicious for developing discitis osteomyelitis with adjacent psoas muscle myositis. Remarkable labs included leukocytosis, and elevated ESR and CRP. Urine cultures were negative. Blood cultures, which were drawn after two days of receiving ciprofloxacin, were negative. The patient underwent CT-guided biopsy of the L2/L3 disc. Cultures were negative. Patient subsequently underwent a surgical biopsy. The patient was initiated on empiric IV vancomycin and ceftriaxone. Upon discharge, the vancomycin was transitioned to daptomycin to complete a 6 week course. The biopsy culture resulted positive for Actinotignum schaalii after his discharge from the hospital. A colonoscopy revealed only benign polypoid mucosa with rare lymphoid follicles and surface erosions.
Discussion: This patient with Crohn’s disease and Actinotignum schaalii spondylodiscitis was successfully treated with long term IV antibiotics. The pathogenesis of the infection is unclear, although presumed to be secondary to a UTI. The route of inoculation is likely hematogenous via Batson’s venous plexus. However, the immunosuppression secondary to Crohn’s disease and biologic therapy were contributing factors. This case highlights the complexity of diagnosing and managing a patient with Crohn’s disease with prior exposure to immunosuppressive therapy and spondylodiscitis. This is the first reported case of Actinotignum schaalii spondylodiscitis in a Crohn’s disease patient with previous exposure to infliximab.
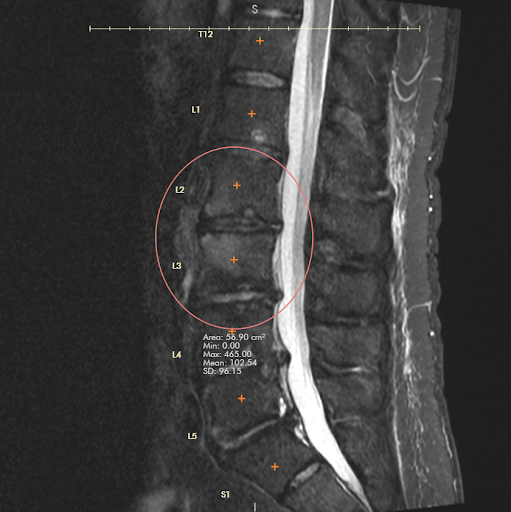
Figure: Figure 1. Bone marrow edema within L2 and L3.
Disclosures:
Austin Tiesenga indicated no relevant financial relationships.
Thomas Birris: BMS – Speakers Bureau.
William Schreiner indicated no relevant financial relationships.
David Malaka indicated no relevant financial relationships.
Rafeek Woods indicated no relevant financial relationships.
Michael Wang indicated no relevant financial relationships.
Austin Tiesenga, DO1, Thomas Birris, MD2, William Schreiner, MD1, David Malaka, MD1, Rafeek Woods, MD1, Michael Wang, MD1. P3488 - A Rare Case of Spondylodiscitis Due to <i>Actinotignum schaalii</i> In a Patient With Crohn’s Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Corewell Health Lakeland, St. Joseph, MI; 2Corewell Health Lakeland, Saint Joseph, MI
Introduction: Patients with Crohn’s disease have an increased risk for infectious spondylodiscitis, particularly in the presence of GI fistula formation. Patients with inflammatory bowel disease (IBD) can also develop autoimmune causes of spondyloarthritis, including HLA-B27 related disease, which can complicate identifying the underlying etiology of spondylodiscitis. We report a rare case of spondylodiscitis secondary to Actinotignum schaalii, an uncommon urinary pathogen, in a patient with a history of Crohn’s disease and previous exposure to infliximab therapy.
Case Description/
Methods: We present a 55 year old male with a PMH of Crohn’s disease with a prior exposure to infliximab, degenerative disc disease, and chronic urinary retention, who presented for worsening back pain. He was treated for a UTI two days prior to admission with ciprofloxacin. He denied fever, chills, dysuria, frequency, urgency, numbness, weakness bilateral lower extremities, and saddle anesthesia. The MRI lumbar spine/sacrum revealed bone marrow edema within L2/L3, suspicious for developing discitis osteomyelitis with adjacent psoas muscle myositis. Remarkable labs included leukocytosis, and elevated ESR and CRP. Urine cultures were negative. Blood cultures, which were drawn after two days of receiving ciprofloxacin, were negative. The patient underwent CT-guided biopsy of the L2/L3 disc. Cultures were negative. Patient subsequently underwent a surgical biopsy. The patient was initiated on empiric IV vancomycin and ceftriaxone. Upon discharge, the vancomycin was transitioned to daptomycin to complete a 6 week course. The biopsy culture resulted positive for Actinotignum schaalii after his discharge from the hospital. A colonoscopy revealed only benign polypoid mucosa with rare lymphoid follicles and surface erosions.
Discussion: This patient with Crohn’s disease and Actinotignum schaalii spondylodiscitis was successfully treated with long term IV antibiotics. The pathogenesis of the infection is unclear, although presumed to be secondary to a UTI. The route of inoculation is likely hematogenous via Batson’s venous plexus. However, the immunosuppression secondary to Crohn’s disease and biologic therapy were contributing factors. This case highlights the complexity of diagnosing and managing a patient with Crohn’s disease with prior exposure to immunosuppressive therapy and spondylodiscitis. This is the first reported case of Actinotignum schaalii spondylodiscitis in a Crohn’s disease patient with previous exposure to infliximab.
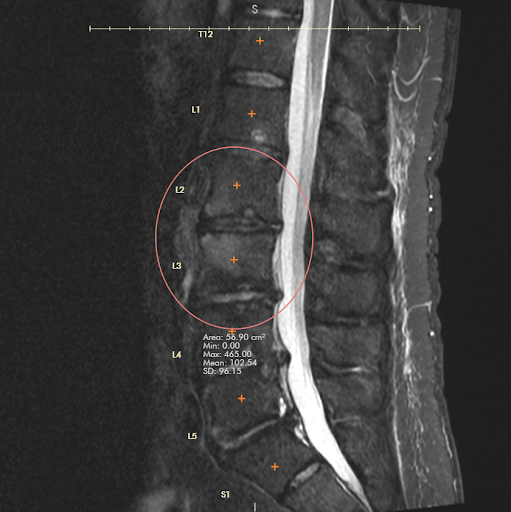
Figure: Figure 1. Bone marrow edema within L2 and L3.
Disclosures:
Austin Tiesenga indicated no relevant financial relationships.
Thomas Birris: BMS – Speakers Bureau.
William Schreiner indicated no relevant financial relationships.
David Malaka indicated no relevant financial relationships.
Rafeek Woods indicated no relevant financial relationships.
Michael Wang indicated no relevant financial relationships.
Austin Tiesenga, DO1, Thomas Birris, MD2, William Schreiner, MD1, David Malaka, MD1, Rafeek Woods, MD1, Michael Wang, MD1. P3488 - A Rare Case of Spondylodiscitis Due to <i>Actinotignum schaalii</i> In a Patient With Crohn’s Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
