Monday Poster Session
Category: Infections and Microbiome
P3486 - Gastric Mucormycosis in a Critically Ill Patient Who Survived: A Case Report
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Andrej M. Sodoma, DO
Northwell Health
Lake Grove, NY
Presenting Author(s)
Andrej M. Sodoma, DO1, Atieh Ashkezari, BS2, James Pellegrini, MD3, Schweta Chaudhary, MD4, Mary Thomas, DO4
1Northwell Health, Lake Grove, NY; 2NYIT College of Osteopathic Medicine, Old Westbury, NY; 3Nassau University Medical Center, East Meadow, NY; 4Northwell Health, Bay Shore, NY
Introduction: Mucormycosis is a rare but severe fungal infection. Its incidence is roughly 1.7 cases per million population per year, and its mortality rate is >50%. Gastrointestinal mucormycosis is an uncommon disease variant, constituting approximately 4% of all cases. This case involves a 57-year-old man with pre-existing diabetes who was not adhering to his medications.
Case Description/
Methods: On admission, he was diagnosed with severe acute respiratory distress syndrome (ARDS). While in the intensive care unit (ICU), he had persistent anemia and gastrointestinal bleeding despite antimicrobial therapy and supportive care. An esophagogastroduodenoscopy (EGD) performed. It showed necrotic tissue in the gastric fundus with ulcerated edges, suggesting invasive fungal infection, malignancy, or ischemic process. Biopsies confirmed mucormycosis with mycetoma. The progression of the EGD findings was key in this case, as there was a significant decrease in the necrotic tissue with antifungal therapy. There was a considerable improvement in the follow-up EGD; the necrotic burden was reduced, and the ulcer bases were better visualized. Initially, amphotericin B was administered as an antifungal therapy with a transition to isavuconazonium after renal impairment. The patient was on a proton pump inhibitor (PPI), sucralfate, and enteral nutrition. Surgical debridement was considered; however, the patient was too unstable for surgery. He had multiple complications, including aspiration pneumonia, septic shock, and multi-organ failure, leading to a prolonged stay in the intensive care unit (ICU). Given the severity of his gastric mucormycosis and its poor prognosis, his recovery was quite unexpected. With the help of antifungal treatment and other support, he improved gradually and was able to come off mechanical ventilation to supplemental oxygen only. Over time, he regained his strength, had his tracheostomy removed, and could speak and eat. The patient was discharged home on supplemental oxygen, requiring home care, and on an extensive medication regimen, including apixaban, isavuconazonium, metformin, and pantoprazole. He was instructed to follow up with pulmonology, infectious disease, gastroenterology, and his primary care physician.
Discussion: Gastric mucormycosis should be suspected clinically in critically ill patients with gastrointestinal symptoms, as highlighted in this case. Early recognition and appropriate management with antifungal agents can lead to a better outcome.
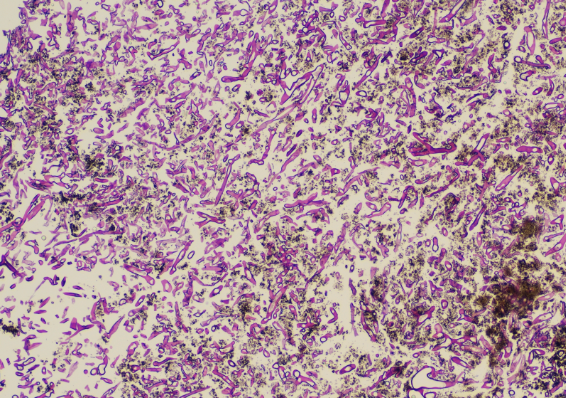
Figure: EGD biopsy was performed and sent for analysis. It showed broad, non-septate hyphae. The angle of branching is greater than in other organisms and usually approaches 90°. They are wider than Aspergillus species and branch irregularly. No background gastric mucosa was seen.
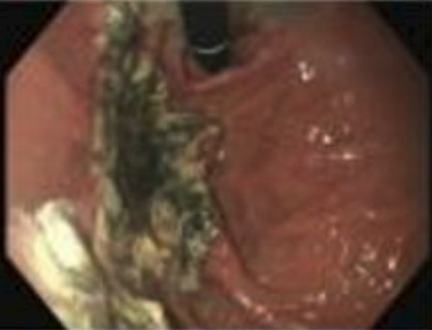
Figure: EGD was performed which showed a necrotic mass.
Disclosures:
Andrej Sodoma indicated no relevant financial relationships.
Atieh Ashkezari indicated no relevant financial relationships.
James Pellegrini indicated no relevant financial relationships.
Schweta Chaudhary indicated no relevant financial relationships.
Mary Thomas indicated no relevant financial relationships.
Andrej M. Sodoma, DO1, Atieh Ashkezari, BS2, James Pellegrini, MD3, Schweta Chaudhary, MD4, Mary Thomas, DO4. P3486 - Gastric Mucormycosis in a Critically Ill Patient Who Survived: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Northwell Health, Lake Grove, NY; 2NYIT College of Osteopathic Medicine, Old Westbury, NY; 3Nassau University Medical Center, East Meadow, NY; 4Northwell Health, Bay Shore, NY
Introduction: Mucormycosis is a rare but severe fungal infection. Its incidence is roughly 1.7 cases per million population per year, and its mortality rate is >50%. Gastrointestinal mucormycosis is an uncommon disease variant, constituting approximately 4% of all cases. This case involves a 57-year-old man with pre-existing diabetes who was not adhering to his medications.
Case Description/
Methods: On admission, he was diagnosed with severe acute respiratory distress syndrome (ARDS). While in the intensive care unit (ICU), he had persistent anemia and gastrointestinal bleeding despite antimicrobial therapy and supportive care. An esophagogastroduodenoscopy (EGD) performed. It showed necrotic tissue in the gastric fundus with ulcerated edges, suggesting invasive fungal infection, malignancy, or ischemic process. Biopsies confirmed mucormycosis with mycetoma. The progression of the EGD findings was key in this case, as there was a significant decrease in the necrotic tissue with antifungal therapy. There was a considerable improvement in the follow-up EGD; the necrotic burden was reduced, and the ulcer bases were better visualized. Initially, amphotericin B was administered as an antifungal therapy with a transition to isavuconazonium after renal impairment. The patient was on a proton pump inhibitor (PPI), sucralfate, and enteral nutrition. Surgical debridement was considered; however, the patient was too unstable for surgery. He had multiple complications, including aspiration pneumonia, septic shock, and multi-organ failure, leading to a prolonged stay in the intensive care unit (ICU). Given the severity of his gastric mucormycosis and its poor prognosis, his recovery was quite unexpected. With the help of antifungal treatment and other support, he improved gradually and was able to come off mechanical ventilation to supplemental oxygen only. Over time, he regained his strength, had his tracheostomy removed, and could speak and eat. The patient was discharged home on supplemental oxygen, requiring home care, and on an extensive medication regimen, including apixaban, isavuconazonium, metformin, and pantoprazole. He was instructed to follow up with pulmonology, infectious disease, gastroenterology, and his primary care physician.
Discussion: Gastric mucormycosis should be suspected clinically in critically ill patients with gastrointestinal symptoms, as highlighted in this case. Early recognition and appropriate management with antifungal agents can lead to a better outcome.
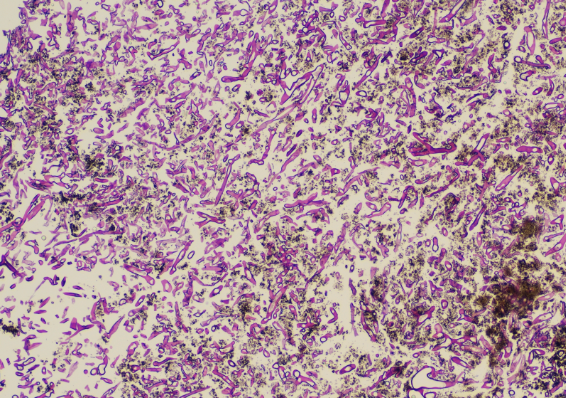
Figure: EGD biopsy was performed and sent for analysis. It showed broad, non-septate hyphae. The angle of branching is greater than in other organisms and usually approaches 90°. They are wider than Aspergillus species and branch irregularly. No background gastric mucosa was seen.
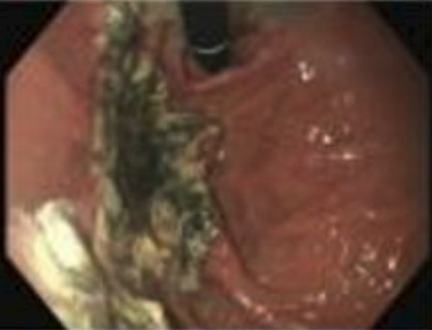
Figure: EGD was performed which showed a necrotic mass.
Disclosures:
Andrej Sodoma indicated no relevant financial relationships.
Atieh Ashkezari indicated no relevant financial relationships.
James Pellegrini indicated no relevant financial relationships.
Schweta Chaudhary indicated no relevant financial relationships.
Mary Thomas indicated no relevant financial relationships.
Andrej M. Sodoma, DO1, Atieh Ashkezari, BS2, James Pellegrini, MD3, Schweta Chaudhary, MD4, Mary Thomas, DO4. P3486 - Gastric Mucormycosis in a Critically Ill Patient Who Survived: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
