Monday Poster Session
Category: Interventional Endoscopy
P3561 - Stone, Scope, Surprise: Ampullary Neuroendocrine Tumor Detected and Resected During Endoscopic Retrograde Cholangiopancreatography
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Priya Kumari Maheshwari, MD (she/her/hers)
University of Central Florida, HCA Healthcare GME
Pensacola, FL
Presenting Author(s)
Priya Kumari Maheshwari, MD1, Sarah Elrod, DO2, Parth Desai, DO2, Zachary Zator, MD2
1University of Central Florida, HCA Healthcare GME, Pensacola, FL; 2Lehigh Valley Health Network, Allentown, PA
Introduction: Ampullary neuroendocrine tumors (NETs) are exceedingly rare, comprising approximately 0.3–1% of gastrointestinal NETs and less than 2% of periampullary tumors. Often asymptomatic and submucosal in origin, they may be missed on routine biopsy. While surgical resection has traditionally been the standard of care, endoscopic ampullectomy has emerged as a viable, less invasive option in select cases. We present a case of an incidentally discovered ampullary NET during endoscopic Retrograde Cholangiopancreatography (ERCP) for choledocholithiasis, successfully treated with endoscopic resection.
Case Description/
Methods: A 72-year-old woman with a history of coronary artery disease, type 1 diabetes, and stage 3 chronic kidney disease presented with epigastric pain. On admission, vitals were: blood pressure 153/51 mmHg, heart rate 79 bpm, respiratory rate 17 breaths/minute, temperature 98.7°F, and oxygen saturation 100% on room air. Physical exam revealed epigastric tenderness. Labs showed elevated lipase to 478 U/L, hemoglobin 10.8 g/dL, and normal liver enzymes and bilirubin.
Computed tomography of the abdomen and pelvis demonstrated a 13 mm distal common bile duct stone with biliary dilation up to 22 mm. The patient underwent ERCP with biliary sphincterotomy, stone extraction, and prophylactic pancreatic duct stenting. A prominent ampulla was noted and biopsied. Histopathology revealed a well-differentiated NET confined to the mucosa. Endoscopic ultrasound (EUS) demonstrated a 13 mm hypoechoic ampullary lesion limited to the mucosal layer, with no invasion of the pancreatic or bile ducts and no regional lymphadenopathy.
Following multidisciplinary discussion, a second ERCP was performed with endoscopic mucosal resection (EMR) and ampullectomy. The lesion was removed piecemeal using submucosal lift and hot snare technique. Final pathology confirmed complete excision. The patient recovered without complication and was discharged with plans for surveillance endoscopy.
Discussion: Ampullary NETs are rare and often diagnosed incidentally. While pancreaticoduodenectomy has been the mainstay of treatment, recent evidence supports endoscopic resection in small, well-differentiated, non-invasive tumors. This case highlights the role of careful ampullary evaluation during ERCP and demonstrates that endoscopic ampullectomy can be curative in appropriately selected patients, offering a less invasive alternative to surgery. Long-term outcomes and recurrence data remain limited and warrant further study.
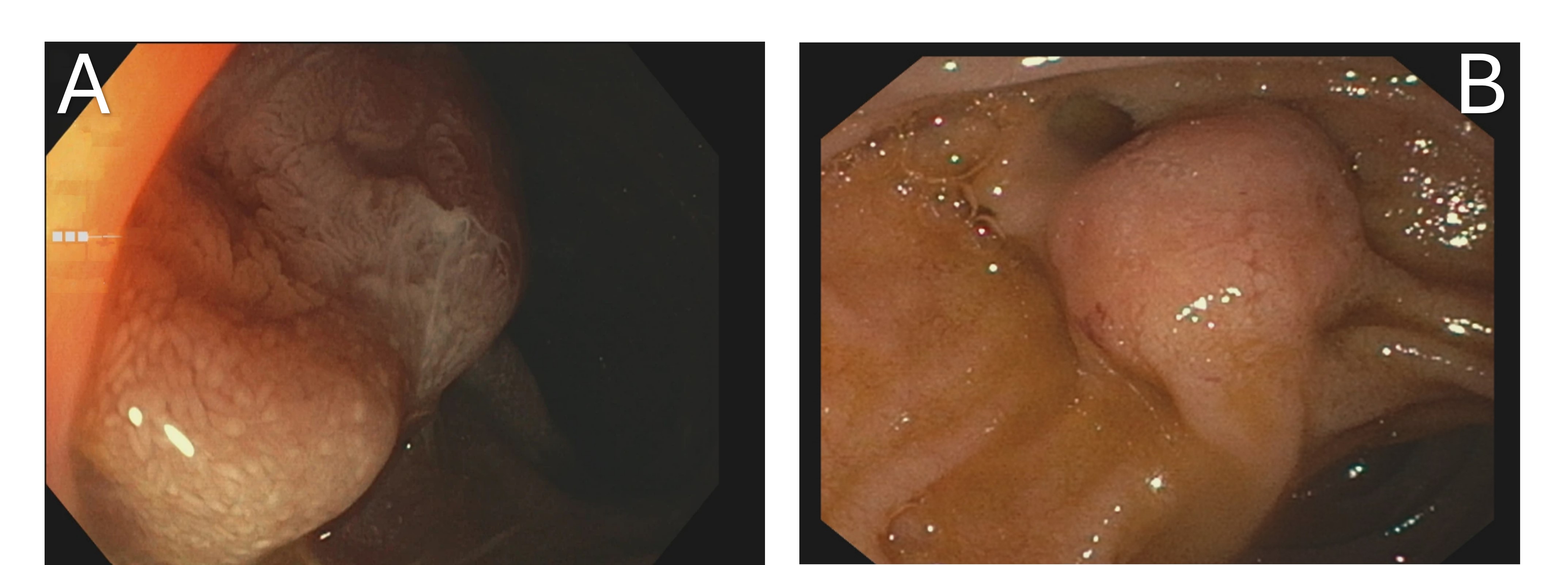
Figure: Figure 1A-B: Endoscopic image demonstrating a prominent ampullary lesion.
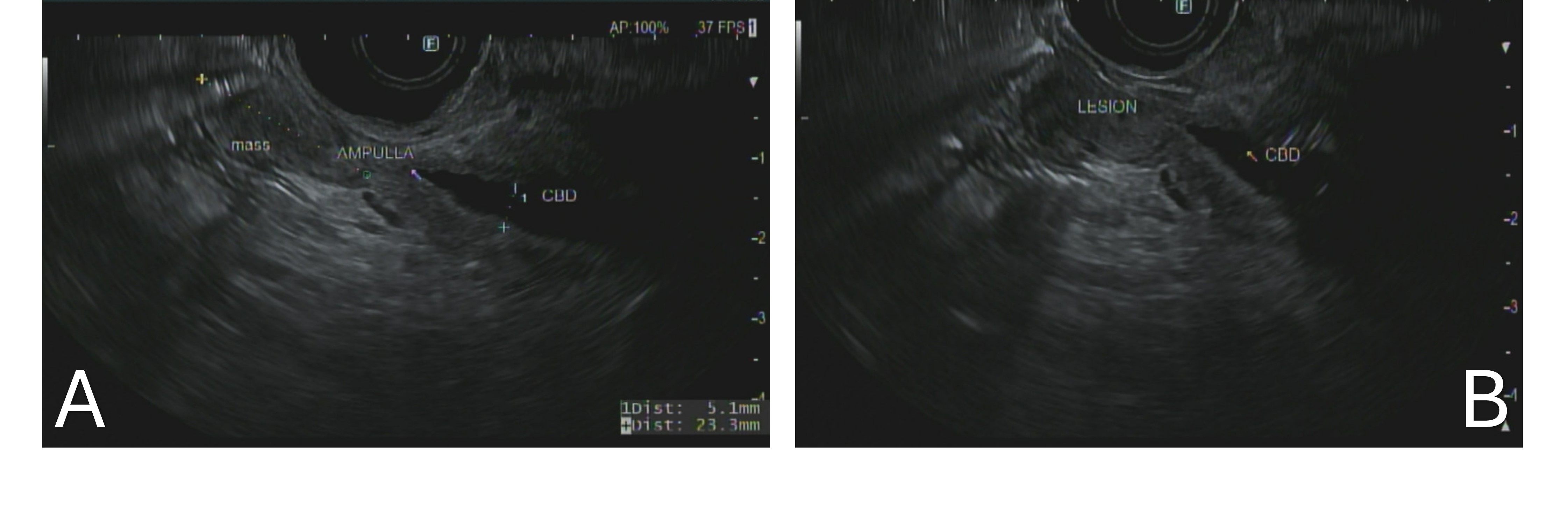
Figure: Figure 2A-B: Endoscopic ultrasound (EUS) image showing a hypoechoic lesion at the ampulla.
Disclosures:
Priya Kumari Maheshwari indicated no relevant financial relationships.
Sarah Elrod indicated no relevant financial relationships.
Parth Desai indicated no relevant financial relationships.
Zachary Zator indicated no relevant financial relationships.
Priya Kumari Maheshwari, MD1, Sarah Elrod, DO2, Parth Desai, DO2, Zachary Zator, MD2. P3561 - Stone, Scope, Surprise: Ampullary Neuroendocrine Tumor Detected and Resected During Endoscopic Retrograde Cholangiopancreatography, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Central Florida, HCA Healthcare GME, Pensacola, FL; 2Lehigh Valley Health Network, Allentown, PA
Introduction: Ampullary neuroendocrine tumors (NETs) are exceedingly rare, comprising approximately 0.3–1% of gastrointestinal NETs and less than 2% of periampullary tumors. Often asymptomatic and submucosal in origin, they may be missed on routine biopsy. While surgical resection has traditionally been the standard of care, endoscopic ampullectomy has emerged as a viable, less invasive option in select cases. We present a case of an incidentally discovered ampullary NET during endoscopic Retrograde Cholangiopancreatography (ERCP) for choledocholithiasis, successfully treated with endoscopic resection.
Case Description/
Methods: A 72-year-old woman with a history of coronary artery disease, type 1 diabetes, and stage 3 chronic kidney disease presented with epigastric pain. On admission, vitals were: blood pressure 153/51 mmHg, heart rate 79 bpm, respiratory rate 17 breaths/minute, temperature 98.7°F, and oxygen saturation 100% on room air. Physical exam revealed epigastric tenderness. Labs showed elevated lipase to 478 U/L, hemoglobin 10.8 g/dL, and normal liver enzymes and bilirubin.
Computed tomography of the abdomen and pelvis demonstrated a 13 mm distal common bile duct stone with biliary dilation up to 22 mm. The patient underwent ERCP with biliary sphincterotomy, stone extraction, and prophylactic pancreatic duct stenting. A prominent ampulla was noted and biopsied. Histopathology revealed a well-differentiated NET confined to the mucosa. Endoscopic ultrasound (EUS) demonstrated a 13 mm hypoechoic ampullary lesion limited to the mucosal layer, with no invasion of the pancreatic or bile ducts and no regional lymphadenopathy.
Following multidisciplinary discussion, a second ERCP was performed with endoscopic mucosal resection (EMR) and ampullectomy. The lesion was removed piecemeal using submucosal lift and hot snare technique. Final pathology confirmed complete excision. The patient recovered without complication and was discharged with plans for surveillance endoscopy.
Discussion: Ampullary NETs are rare and often diagnosed incidentally. While pancreaticoduodenectomy has been the mainstay of treatment, recent evidence supports endoscopic resection in small, well-differentiated, non-invasive tumors. This case highlights the role of careful ampullary evaluation during ERCP and demonstrates that endoscopic ampullectomy can be curative in appropriately selected patients, offering a less invasive alternative to surgery. Long-term outcomes and recurrence data remain limited and warrant further study.
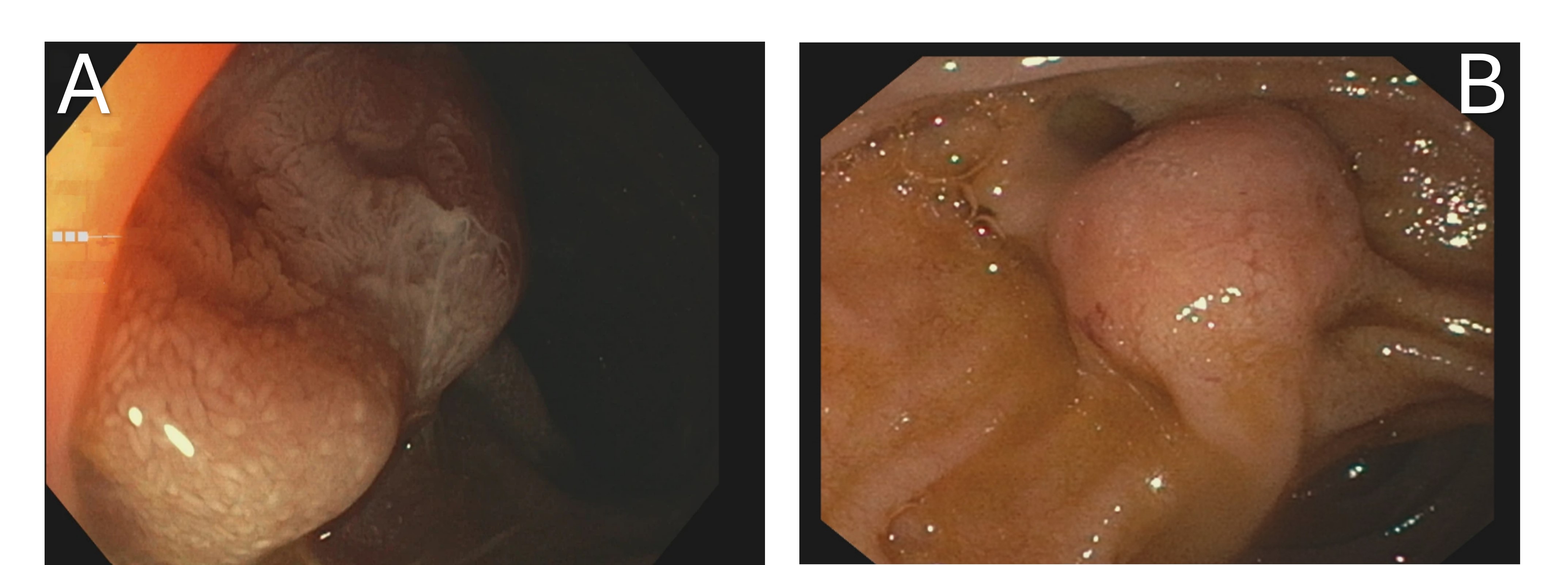
Figure: Figure 1A-B: Endoscopic image demonstrating a prominent ampullary lesion.
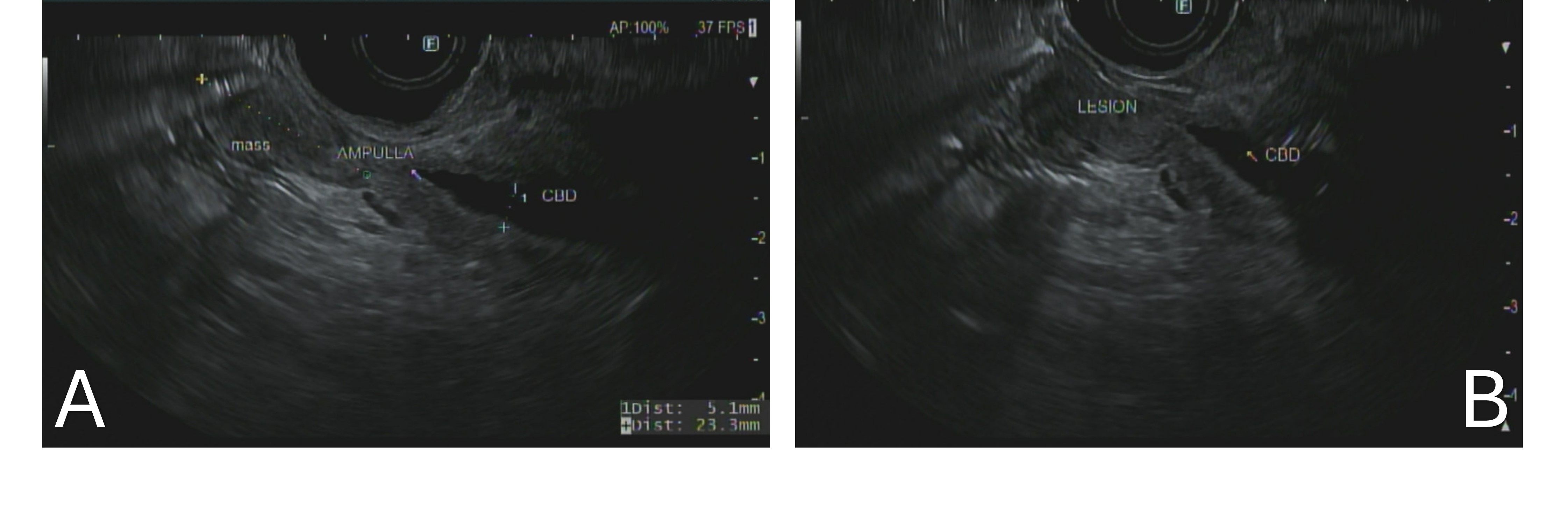
Figure: Figure 2A-B: Endoscopic ultrasound (EUS) image showing a hypoechoic lesion at the ampulla.
Disclosures:
Priya Kumari Maheshwari indicated no relevant financial relationships.
Sarah Elrod indicated no relevant financial relationships.
Parth Desai indicated no relevant financial relationships.
Zachary Zator indicated no relevant financial relationships.
Priya Kumari Maheshwari, MD1, Sarah Elrod, DO2, Parth Desai, DO2, Zachary Zator, MD2. P3561 - Stone, Scope, Surprise: Ampullary Neuroendocrine Tumor Detected and Resected During Endoscopic Retrograde Cholangiopancreatography, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
