Monday Poster Session
Category: Interventional Endoscopy
P3559 - The Effect of Anticoagulation on Outcomes of Endoscopic Upper GI Balloon Dilation
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- OA
Osama Alshakhatreh, MD (he/him/his)
Albany Medical Center
Norfolk, VA
Presenting Author(s)
Osama Alshakhatreh, MD1, Omar Arman, MD, MPH2, Shunsa Tarar, DO1, Ibrahim Mohammed, MD1, Khaled Elsokary, DO1, Mohsin Chundrigar, MBBS1, Seth Richter, MD, FACG1
1Albany Medical Center, Albany, NY; 2University at Buffalo, Buffalo, NY
Introduction: Upper endoscopy with balloon dilation is a commonly performed procedure to widen narrowed areas within the esophagus or stomach. As with any procedure, there is a potential for complications which includes bleeding, perforation, and seeding infections. The risk of gastrointestinal bleeding is increased in patients on anticoagulants/antiplatelets (AP/AC). The potential influence of AC therapy on endoscopic balloon dilation outcomes is not well-established. This study investigates the outcomes of endoscopic dilation of upper GI tract in patients using AC vs non-users.
Methods: This retrospective cohort study utilized a global federated health research network database, TriNetX. Patients who underwent upper endoscopy with balloon dilation were stratified into two cohorts, those on AC vs those on no AC. AC use was defined as DOAC or Warfarin taken within 7 days prior to procedure. Use of AP was an exclusion criterion for both cohorts. Both cohorts were matched for baseline demographics and co-morbidities including CKD, thrombocytopenia, and PPI use. Incidence rate for 3 outcomes; GI bleed, hospitalization and requiring transfusion, were assessed at 30 days with evaluation of risk differences between the cohort groups. Falsification endpoints were analyzed to assess residual confounding.
Results: In the non-AC group 231 of 4,140 had the adverse event of a GI bleed after balloon dilation. In contrast, the AC group 349 of 4,140 had a GI bleed. Risk difference 2.9%, p< 0.001.
In the non-AC group 985 of 4,140 were hospitalized post-balloon dilation. In contrast, the AC group 2,049 of 4,140 were hospitalized. Risk difference 25.7%, p< 0.001.
In the non-AC group 117 of 4,140 required transfusion after balloon dilation. In contrast, the AC group 172 of 4,140 required transfusion. Risk in non-AC 2.8% vs AC 4.2%. Risk difference 1.3%, p< 0.001.
Discussion: Our findings show that among patients who undergo upper endoscopy with balloon dilation, the use of AC is associated with increased negative outcomes after balloon dilation including GI bleed, hospitalization and more blood transfusion. Clinicians should carefully weigh the risk of this procedure in patients on AC and consider additional monitoring to mitigate adverse effects. Longer periods of AC washout maybe beneficial for elective procedures.
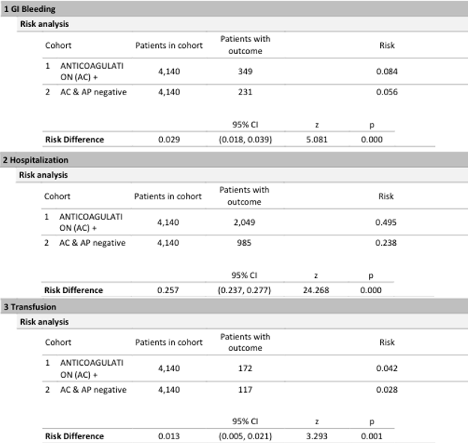
Figure: Table 1: Risk analysis for patients with and without AC with outcomes of GI bleed, hospitalization and transfusion.
Disclosures:
Osama Alshakhatreh indicated no relevant financial relationships.
Omar Arman indicated no relevant financial relationships.
Shunsa Tarar indicated no relevant financial relationships.
Ibrahim Mohammed indicated no relevant financial relationships.
Khaled Elsokary indicated no relevant financial relationships.
Mohsin Chundrigar indicated no relevant financial relationships.
Seth Richter indicated no relevant financial relationships.
Osama Alshakhatreh, MD1, Omar Arman, MD, MPH2, Shunsa Tarar, DO1, Ibrahim Mohammed, MD1, Khaled Elsokary, DO1, Mohsin Chundrigar, MBBS1, Seth Richter, MD, FACG1. P3559 - The Effect of Anticoagulation on Outcomes of Endoscopic Upper GI Balloon Dilation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Albany Medical Center, Albany, NY; 2University at Buffalo, Buffalo, NY
Introduction: Upper endoscopy with balloon dilation is a commonly performed procedure to widen narrowed areas within the esophagus or stomach. As with any procedure, there is a potential for complications which includes bleeding, perforation, and seeding infections. The risk of gastrointestinal bleeding is increased in patients on anticoagulants/antiplatelets (AP/AC). The potential influence of AC therapy on endoscopic balloon dilation outcomes is not well-established. This study investigates the outcomes of endoscopic dilation of upper GI tract in patients using AC vs non-users.
Methods: This retrospective cohort study utilized a global federated health research network database, TriNetX. Patients who underwent upper endoscopy with balloon dilation were stratified into two cohorts, those on AC vs those on no AC. AC use was defined as DOAC or Warfarin taken within 7 days prior to procedure. Use of AP was an exclusion criterion for both cohorts. Both cohorts were matched for baseline demographics and co-morbidities including CKD, thrombocytopenia, and PPI use. Incidence rate for 3 outcomes; GI bleed, hospitalization and requiring transfusion, were assessed at 30 days with evaluation of risk differences between the cohort groups. Falsification endpoints were analyzed to assess residual confounding.
Results: In the non-AC group 231 of 4,140 had the adverse event of a GI bleed after balloon dilation. In contrast, the AC group 349 of 4,140 had a GI bleed. Risk difference 2.9%, p< 0.001.
In the non-AC group 985 of 4,140 were hospitalized post-balloon dilation. In contrast, the AC group 2,049 of 4,140 were hospitalized. Risk difference 25.7%, p< 0.001.
In the non-AC group 117 of 4,140 required transfusion after balloon dilation. In contrast, the AC group 172 of 4,140 required transfusion. Risk in non-AC 2.8% vs AC 4.2%. Risk difference 1.3%, p< 0.001.
Discussion: Our findings show that among patients who undergo upper endoscopy with balloon dilation, the use of AC is associated with increased negative outcomes after balloon dilation including GI bleed, hospitalization and more blood transfusion. Clinicians should carefully weigh the risk of this procedure in patients on AC and consider additional monitoring to mitigate adverse effects. Longer periods of AC washout maybe beneficial for elective procedures.
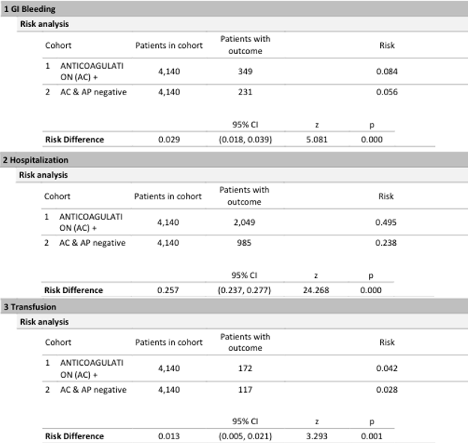
Figure: Table 1: Risk analysis for patients with and without AC with outcomes of GI bleed, hospitalization and transfusion.
Disclosures:
Osama Alshakhatreh indicated no relevant financial relationships.
Omar Arman indicated no relevant financial relationships.
Shunsa Tarar indicated no relevant financial relationships.
Ibrahim Mohammed indicated no relevant financial relationships.
Khaled Elsokary indicated no relevant financial relationships.
Mohsin Chundrigar indicated no relevant financial relationships.
Seth Richter indicated no relevant financial relationships.
Osama Alshakhatreh, MD1, Omar Arman, MD, MPH2, Shunsa Tarar, DO1, Ibrahim Mohammed, MD1, Khaled Elsokary, DO1, Mohsin Chundrigar, MBBS1, Seth Richter, MD, FACG1. P3559 - The Effect of Anticoagulation on Outcomes of Endoscopic Upper GI Balloon Dilation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
