Monday Poster Session
Category: Interventional Endoscopy
P3558 - Long-Term Outcomes of Patients With T1b Esophageal Carcinoma Status Post Endoscopic Resection With Esophagectomy or Surveillance
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- IP
Irene C. Perez, MD, MS
University of Colorado Anschutz Medical Campus
Denver, CO
Presenting Author(s)
Irene C. Perez, MD, MS, Mohammad Bilal, MD, FACG
University of Colorado Anschutz Medical Campus, Denver, CO
Introduction: Esophagectomy is considered standard of care for patients with T1b esophageal carcinoma (EC) with high-risk features due to increased risk for lymph node metastasis (LNM). However, endoscopic resection (ER) can be curative in cases of superficial submucosal invasion. We aimed to compare the disease-free survival and overall survival in patients with T1b EC status post ER and esophagectomy or active surveillance.
Methods: Patients with EC at our tertiary care academic medical center treated with ER [endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD)] from January 2012-December 2021 with ER specimen staged as pathologic T1bNX EC with no presumed metastasis after ER and with at least 1 year of follow-up since ER were included. Histopathologic high-risk features were recorded, and disease-free survival and overall survival was assessed. Independent-samples t-test, Fisher’s exact test and the Kaplan-Meier method were used for statistical analysis.
Results: Forty-one cases with pT1b EC were included (N=19 ER with surveillance, N=22 ER with esophagectomy), and most cases were adenocarcinoma (N=39). The mean age was 73 ± 11 years (ER with surveillance) and 68 ± 7 years (ER with esophagectomy) (p=0.81), and the Charlson co-morbidity index was 6.6 ± 3.8 (ER with surveillance) and 4.6 ± 2.5 (ER with esophagectomy) (p=0.06). Tumor size was 1.23 ± .67 cm and 2.24 ± 2.14 in the surveillance and esophagectomy groups (p=0.06). ESD was the main ER performed. Most lesions were in the lower third of the esophagus and/or GEJ. (Table 1) High-risk features were comparable in the two groups, however, patients in the esophagectomy group were more likely to have positive ER margins (13/23) (p< 0.001). (Table 1) Five patients in the esophagectomy group received neo and/or adjuvant chemotherapy and 1 patient had radiation prior to esophagectomy. Ten (42%) patients with esophagectomy had residual disease on surgical pathology and 4 (17%) had LNM. Additionally, recurrence occurred in 3 (16%) and 6 (25%) patients in the surveillance and esophagectomy groups. There was no difference in disease-free survival (0.433) or overall survival (p=0.610) (Figure 1). Two patients died from post-surgical complications.
Discussion: Patients T1b EC with positive margins were likely to undergo esophagectomy, as expected. Outcomes did not differ for patients who underwent ER with esophagectomy compared to ER with active surveillance.
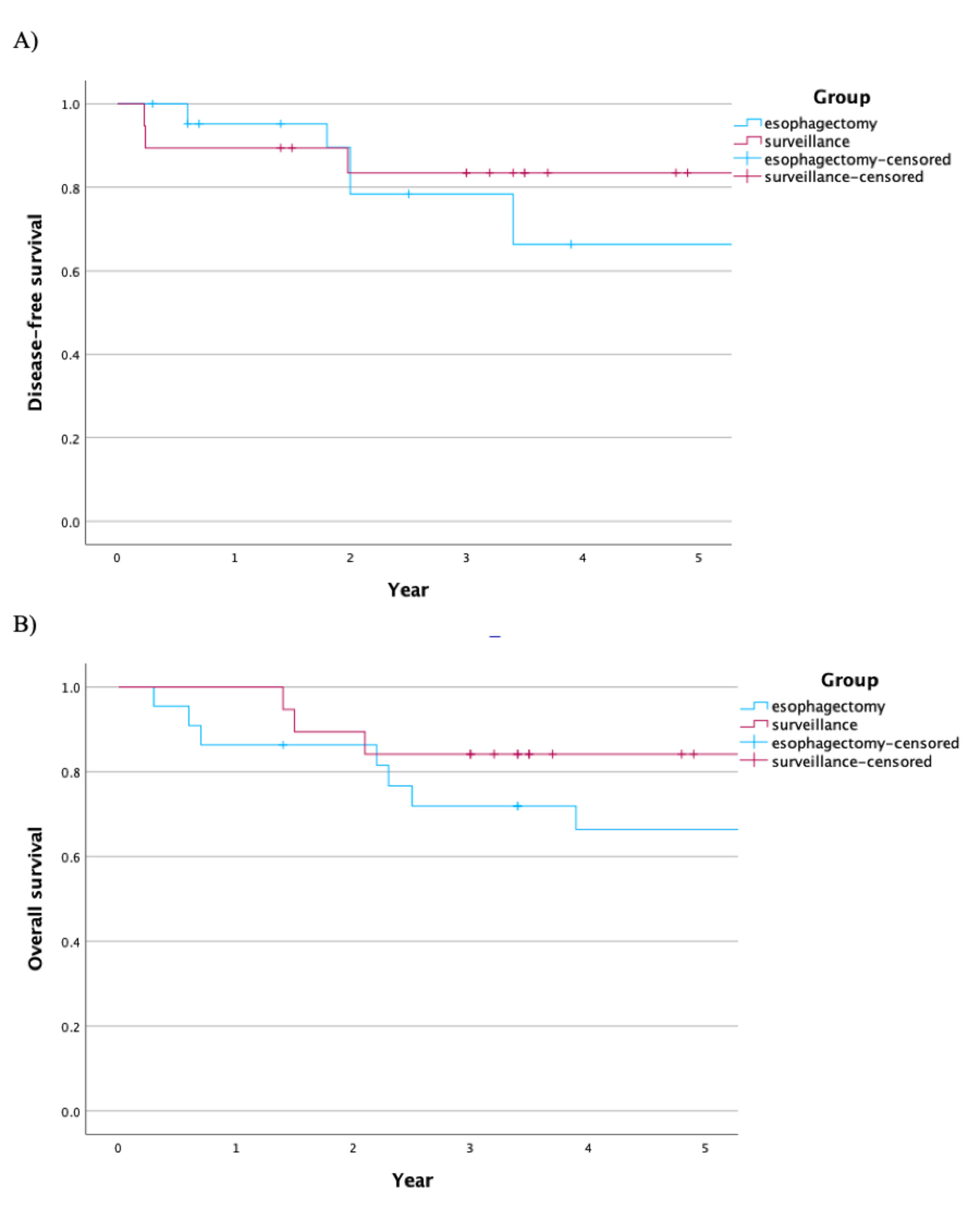
Figure: Table 1. Patient, Tumor and Endoscopic Resection (ER) Characteristics
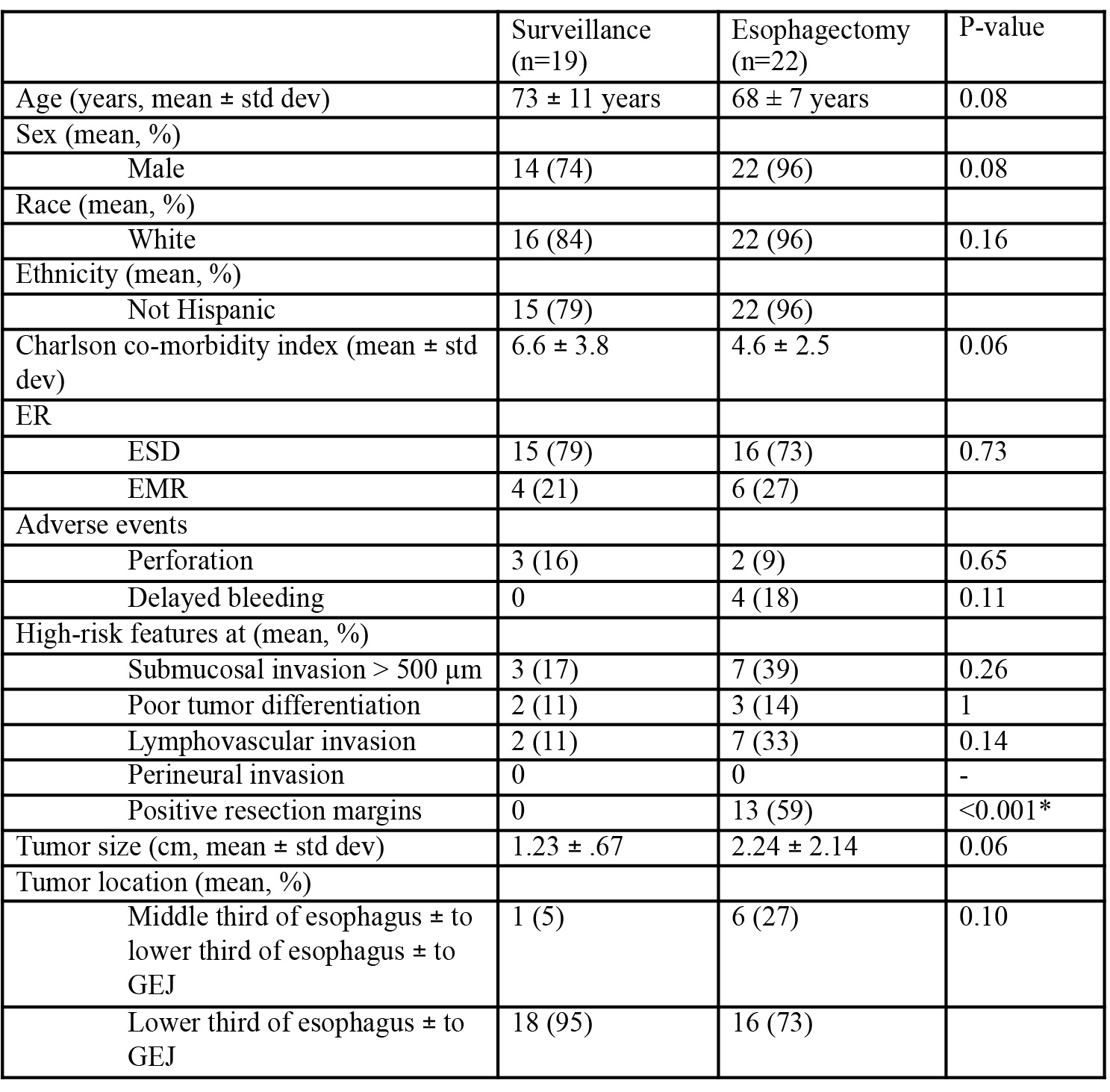
Figure: Figure 1: A) Kaplan-Meier disease-free survival curve is shown for patients with T1b EC and subsequent esophagectomy or surveillance. There was no statistical difference found between the two groups (p=0.433). B) Kaplan-Meier overall survival curve is shown. No statistical difference was found between the two groups (p=0.610).
Disclosures:
Irene Perez indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Irene C. Perez, MD, MS, Mohammad Bilal, MD, FACG. P3558 - Long-Term Outcomes of Patients With T1b Esophageal Carcinoma Status Post Endoscopic Resection With Esophagectomy or Surveillance, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Colorado Anschutz Medical Campus, Denver, CO
Introduction: Esophagectomy is considered standard of care for patients with T1b esophageal carcinoma (EC) with high-risk features due to increased risk for lymph node metastasis (LNM). However, endoscopic resection (ER) can be curative in cases of superficial submucosal invasion. We aimed to compare the disease-free survival and overall survival in patients with T1b EC status post ER and esophagectomy or active surveillance.
Methods: Patients with EC at our tertiary care academic medical center treated with ER [endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD)] from January 2012-December 2021 with ER specimen staged as pathologic T1bNX EC with no presumed metastasis after ER and with at least 1 year of follow-up since ER were included. Histopathologic high-risk features were recorded, and disease-free survival and overall survival was assessed. Independent-samples t-test, Fisher’s exact test and the Kaplan-Meier method were used for statistical analysis.
Results: Forty-one cases with pT1b EC were included (N=19 ER with surveillance, N=22 ER with esophagectomy), and most cases were adenocarcinoma (N=39). The mean age was 73 ± 11 years (ER with surveillance) and 68 ± 7 years (ER with esophagectomy) (p=0.81), and the Charlson co-morbidity index was 6.6 ± 3.8 (ER with surveillance) and 4.6 ± 2.5 (ER with esophagectomy) (p=0.06). Tumor size was 1.23 ± .67 cm and 2.24 ± 2.14 in the surveillance and esophagectomy groups (p=0.06). ESD was the main ER performed. Most lesions were in the lower third of the esophagus and/or GEJ. (Table 1) High-risk features were comparable in the two groups, however, patients in the esophagectomy group were more likely to have positive ER margins (13/23) (p< 0.001). (Table 1) Five patients in the esophagectomy group received neo and/or adjuvant chemotherapy and 1 patient had radiation prior to esophagectomy. Ten (42%) patients with esophagectomy had residual disease on surgical pathology and 4 (17%) had LNM. Additionally, recurrence occurred in 3 (16%) and 6 (25%) patients in the surveillance and esophagectomy groups. There was no difference in disease-free survival (0.433) or overall survival (p=0.610) (Figure 1). Two patients died from post-surgical complications.
Discussion: Patients T1b EC with positive margins were likely to undergo esophagectomy, as expected. Outcomes did not differ for patients who underwent ER with esophagectomy compared to ER with active surveillance.
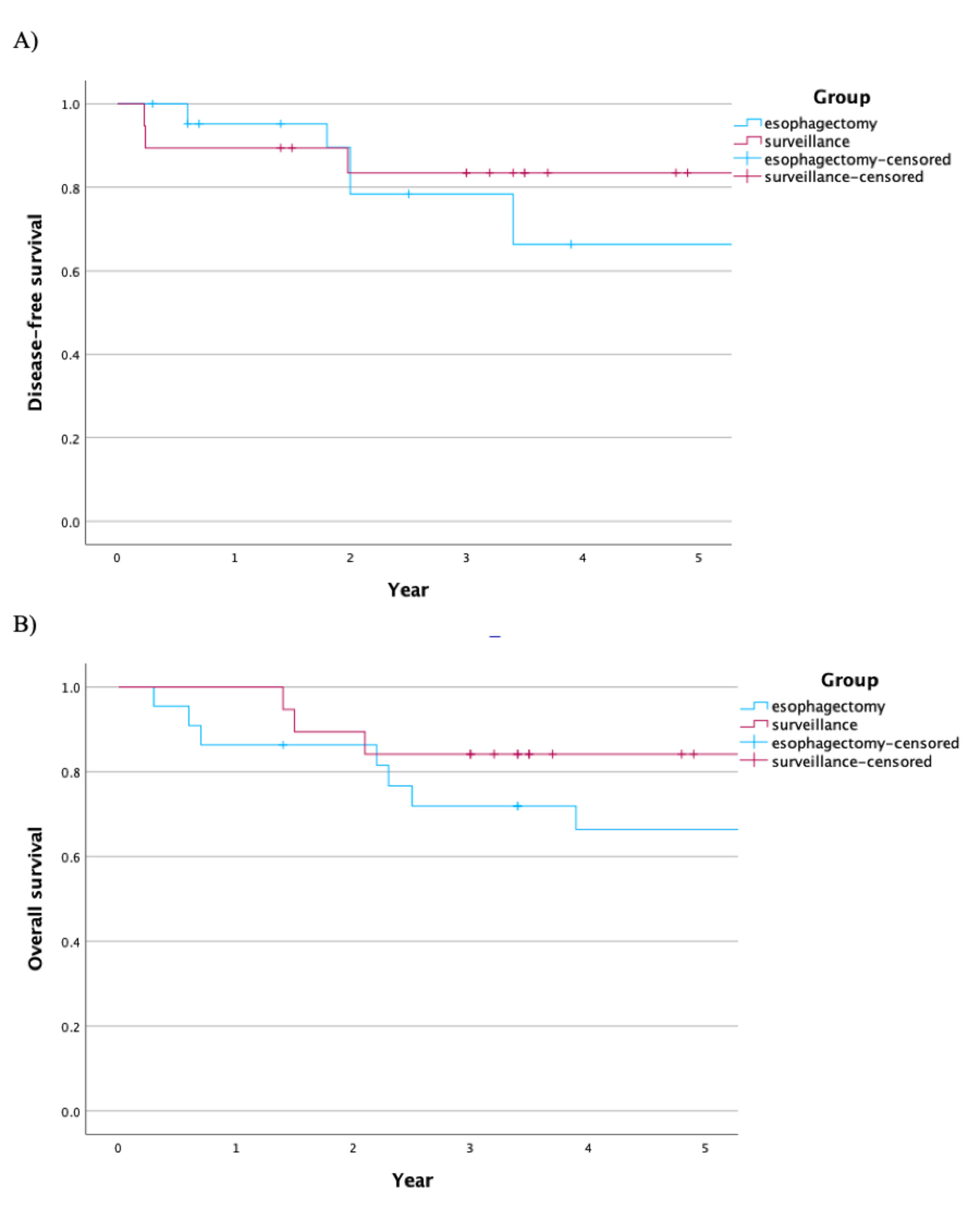
Figure: Table 1. Patient, Tumor and Endoscopic Resection (ER) Characteristics
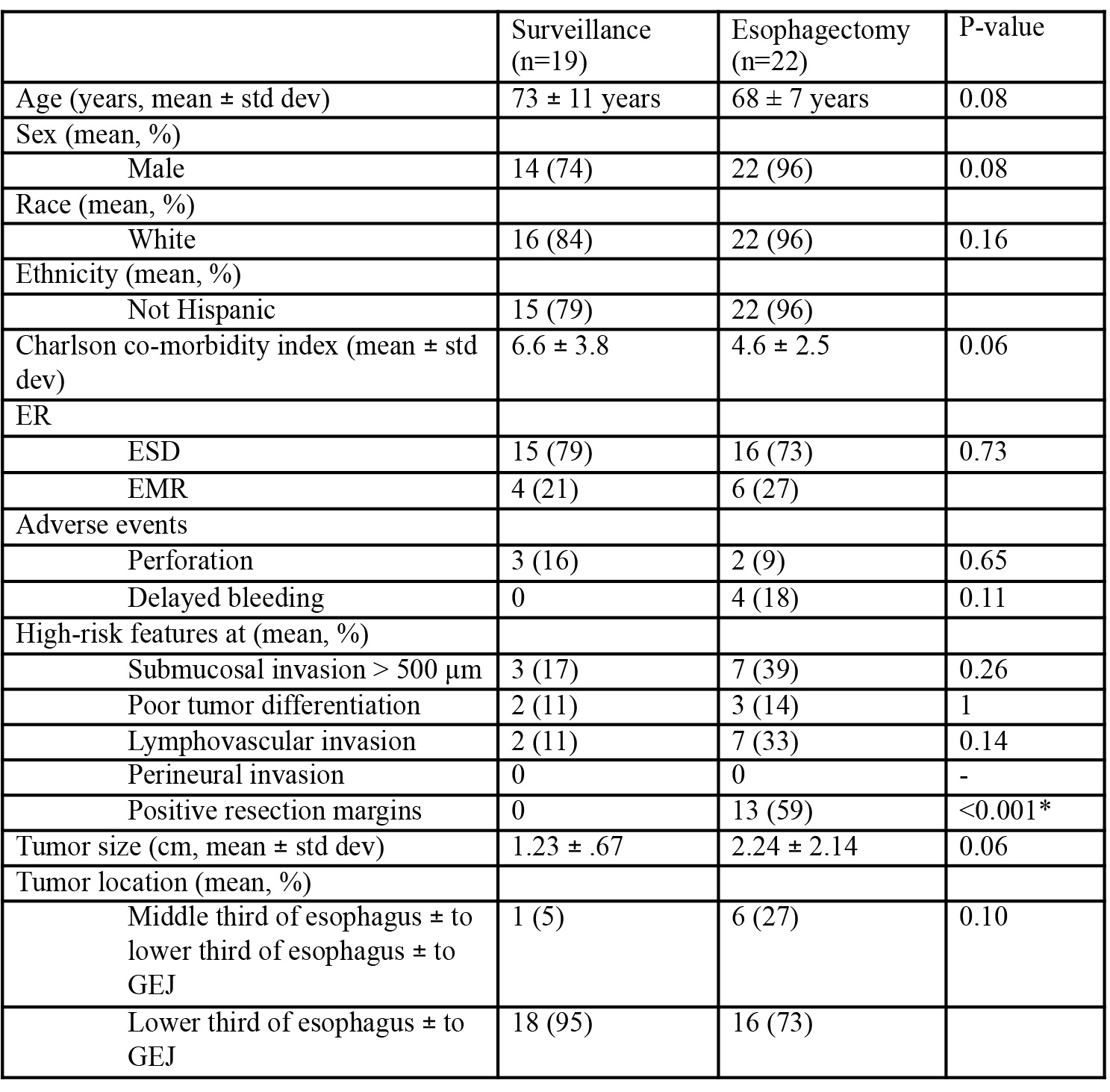
Figure: Figure 1: A) Kaplan-Meier disease-free survival curve is shown for patients with T1b EC and subsequent esophagectomy or surveillance. There was no statistical difference found between the two groups (p=0.433). B) Kaplan-Meier overall survival curve is shown. No statistical difference was found between the two groups (p=0.610).
Disclosures:
Irene Perez indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Irene C. Perez, MD, MS, Mohammad Bilal, MD, FACG. P3558 - Long-Term Outcomes of Patients With T1b Esophageal Carcinoma Status Post Endoscopic Resection With Esophagectomy or Surveillance, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
