Monday Poster Session
Category: Interventional Endoscopy
P3553 - The Rise of POEM: Achalasia Treatment Trends, Institutional Disparities, and the Impact of CPT Coding in a Nationwide Cohort (2014-2024)
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mohammad AbuAssi, MD (he/him/his)
University of Central Florida, HCA Healthcare GME
Gainesville, FL
Presenting Author(s)
Mohammad Abuassi, MD1, Ashraf Almomani, MD2, Kobina Essilfie-Quaye, MD3, Carson Creamer, DO1, Harsimran Kalsi, MD3, Yeshika Thapa, MD3, Tony Brar, MD3, Yaseen Perbtani, DO1
1University of Central Florida, HCA Healthcare GME, Gainesville, FL; 2Cleveland Clinic Florida, Weston, FL; 3University of Central Florida, Gainesville, FL
Introduction: Peroral endoscopic myotomy (POEM) has transformed the management of achalasia over the past decade. While utilization has increased, the impact of procedural coding changes and institutional disparities remains unclear. This study assessed nationwide trends in achalasia treatment, institutional differences in POEM adoption, and the effect of the 2022 CPT code introduction.
Methods: We analyzed adults diagnosed with achalasia (2014–2024) using the TriNetX Network, a large, federated database of de-identified electronic health records from academic and community healthcare organizations across the U.S. We calculated annual incidence proportions and prevalence rates for POEM, laparoscopic Heller myotomy (LHM), pneumatic dilation (PD), and botulinum toxin injection (BT), defined per 100,000 patients with achalasia. Interrupted time series (ITS) analysis was used to assess the impact of the dedicated CPT code for POEM introduced in 2022. Procedure utilization trends were compared between academic and non-academic institutions and stratified by age group.
Results: Among 47,881 patients (mean age 66 ± 17 years; 53% female), achalasia diagnoses nearly doubled over the study period. POEM utilization rose sharply from 0.42% in 2014 to 3.21% in 2024, while LHM declined from 1.46% to 0.94%. BT use increased four-fold, whereas PD rates remained relatively stable. Despite the 2022 CPT code implementation, ITS analysis showed no significant change in POEM utilization slope or level (p > 0.30). In 2024, POEM rates were over four times higher in academic centers versus non-academic centers (4,112 vs 989 per 100,000 achalasia patients; p < 0.001). Age-based analysis revealed that younger patients (< 40 years) predominantly underwent POEM or LHM, whereas older adults ( >60 years) were more likely to receive PD or BT.
Discussion: Over the past decade, POEM has emerged as the leading therapy for achalasia in the U.S., with its adoption driven primarily by clinical efficacy and provider expertise rather than reimbursement or procedural coding changes, as demonstrated by our ITS analysis. However, substantial disparities persist across institutional settings and age groups, with academic centers exhibiting significantly higher and earlier adoption. These findings highlight the need for broader dissemination, enhanced training, and equitable access to advanced endoscopic therapies across all practice environments.
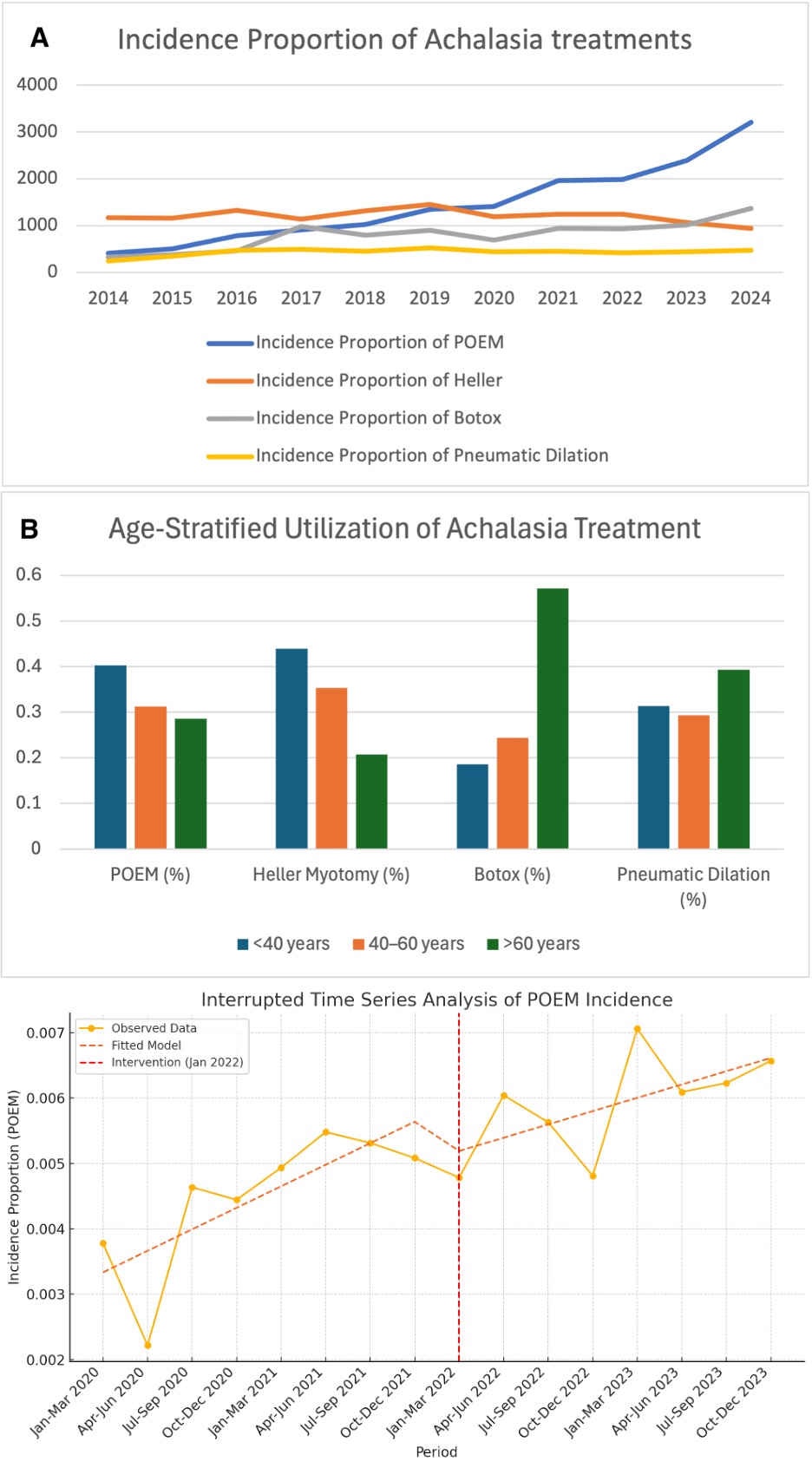
Figure: National Trends in Achalasia Treatment Utilization, Age Stratification, and Impact of CPT Coding (2014–2024).

Figure: Institutional Disparities in POEM and Other Achalasia Treatments Across Academic and Non-Academic Centers (2014–2024).
Disclosures:
Mohammad Abuassi indicated no relevant financial relationships.
Ashraf Almomani indicated no relevant financial relationships.
Kobina Essilfie-Quaye indicated no relevant financial relationships.
Carson Creamer indicated no relevant financial relationships.
Harsimran Kalsi indicated no relevant financial relationships.
Yeshika Thapa indicated no relevant financial relationships.
Tony Brar indicated no relevant financial relationships.
Yaseen Perbtani indicated no relevant financial relationships.
Mohammad Abuassi, MD1, Ashraf Almomani, MD2, Kobina Essilfie-Quaye, MD3, Carson Creamer, DO1, Harsimran Kalsi, MD3, Yeshika Thapa, MD3, Tony Brar, MD3, Yaseen Perbtani, DO1. P3553 - The Rise of POEM: Achalasia Treatment Trends, Institutional Disparities, and the Impact of CPT Coding in a Nationwide Cohort (2014-2024), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Central Florida, HCA Healthcare GME, Gainesville, FL; 2Cleveland Clinic Florida, Weston, FL; 3University of Central Florida, Gainesville, FL
Introduction: Peroral endoscopic myotomy (POEM) has transformed the management of achalasia over the past decade. While utilization has increased, the impact of procedural coding changes and institutional disparities remains unclear. This study assessed nationwide trends in achalasia treatment, institutional differences in POEM adoption, and the effect of the 2022 CPT code introduction.
Methods: We analyzed adults diagnosed with achalasia (2014–2024) using the TriNetX Network, a large, federated database of de-identified electronic health records from academic and community healthcare organizations across the U.S. We calculated annual incidence proportions and prevalence rates for POEM, laparoscopic Heller myotomy (LHM), pneumatic dilation (PD), and botulinum toxin injection (BT), defined per 100,000 patients with achalasia. Interrupted time series (ITS) analysis was used to assess the impact of the dedicated CPT code for POEM introduced in 2022. Procedure utilization trends were compared between academic and non-academic institutions and stratified by age group.
Results: Among 47,881 patients (mean age 66 ± 17 years; 53% female), achalasia diagnoses nearly doubled over the study period. POEM utilization rose sharply from 0.42% in 2014 to 3.21% in 2024, while LHM declined from 1.46% to 0.94%. BT use increased four-fold, whereas PD rates remained relatively stable. Despite the 2022 CPT code implementation, ITS analysis showed no significant change in POEM utilization slope or level (p > 0.30). In 2024, POEM rates were over four times higher in academic centers versus non-academic centers (4,112 vs 989 per 100,000 achalasia patients; p < 0.001). Age-based analysis revealed that younger patients (< 40 years) predominantly underwent POEM or LHM, whereas older adults ( >60 years) were more likely to receive PD or BT.
Discussion: Over the past decade, POEM has emerged as the leading therapy for achalasia in the U.S., with its adoption driven primarily by clinical efficacy and provider expertise rather than reimbursement or procedural coding changes, as demonstrated by our ITS analysis. However, substantial disparities persist across institutional settings and age groups, with academic centers exhibiting significantly higher and earlier adoption. These findings highlight the need for broader dissemination, enhanced training, and equitable access to advanced endoscopic therapies across all practice environments.
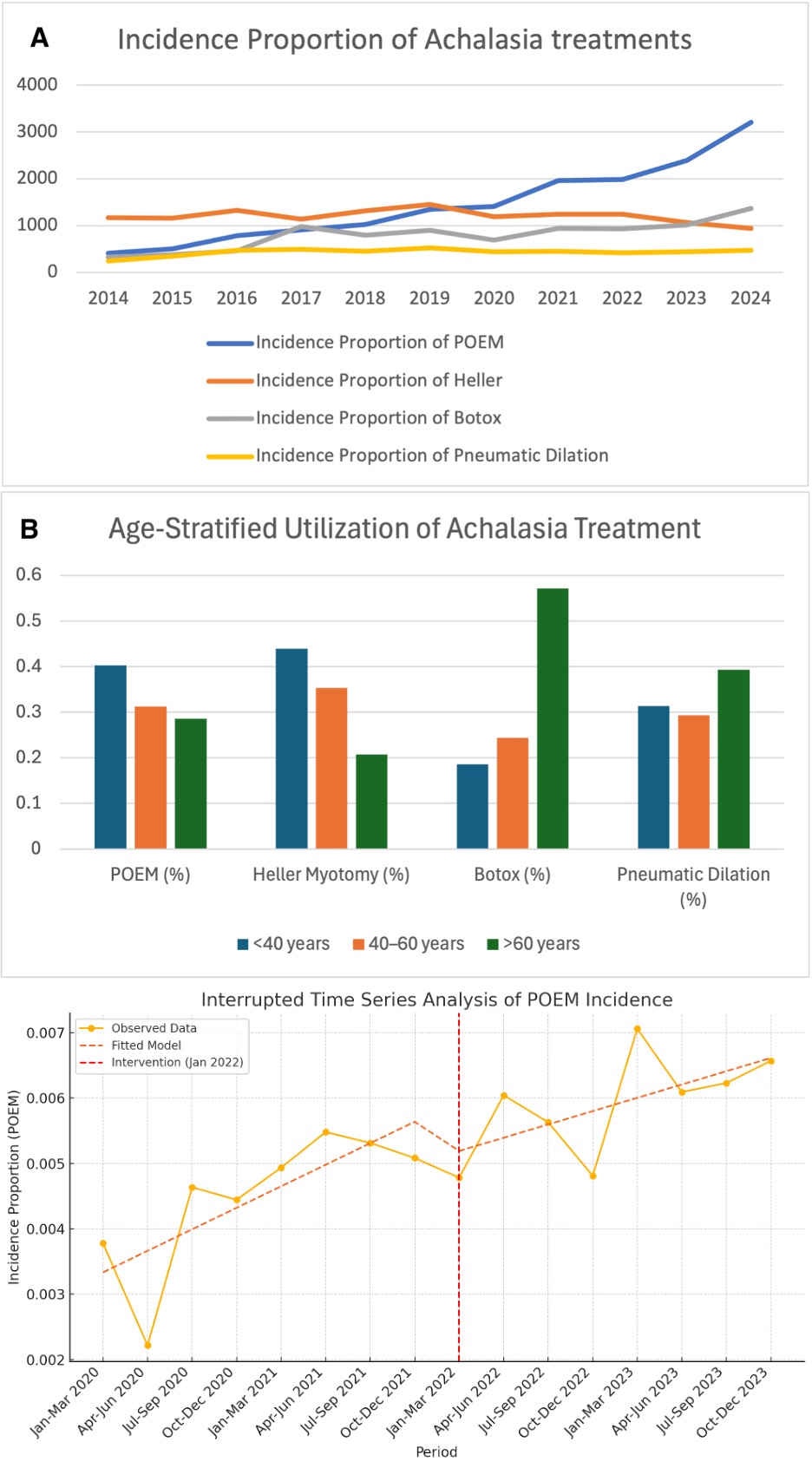
Figure: National Trends in Achalasia Treatment Utilization, Age Stratification, and Impact of CPT Coding (2014–2024).

Figure: Institutional Disparities in POEM and Other Achalasia Treatments Across Academic and Non-Academic Centers (2014–2024).
Disclosures:
Mohammad Abuassi indicated no relevant financial relationships.
Ashraf Almomani indicated no relevant financial relationships.
Kobina Essilfie-Quaye indicated no relevant financial relationships.
Carson Creamer indicated no relevant financial relationships.
Harsimran Kalsi indicated no relevant financial relationships.
Yeshika Thapa indicated no relevant financial relationships.
Tony Brar indicated no relevant financial relationships.
Yaseen Perbtani indicated no relevant financial relationships.
Mohammad Abuassi, MD1, Ashraf Almomani, MD2, Kobina Essilfie-Quaye, MD3, Carson Creamer, DO1, Harsimran Kalsi, MD3, Yeshika Thapa, MD3, Tony Brar, MD3, Yaseen Perbtani, DO1. P3553 - The Rise of POEM: Achalasia Treatment Trends, Institutional Disparities, and the Impact of CPT Coding in a Nationwide Cohort (2014-2024), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
