Monday Poster Session
Category: Liver
P3644 - Primary Biliary Cholangitis: Second-Line Treatment and Outcomes at a Safety Net vs Tertiary Care Hospital Systems
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- SG
Saiabhiroop R. Govindu, BS (he/him/his)
University of Texas Southwestern Medical Center
Frisco, TX
Presenting Author(s)
Meena M. Tadros, MD1, Prajwal Gowda, MD2, Maryln J. Mayo, MD3, Mark R. Pedersen, MD3, Saiabhiroop R. Govindu, BS4
1University of Pennsylvania, Philadelphia, PA; 2University of California San Francisco, San Francisco, CA; 3University of Texas Southwestern Medical Center, Dallas, TX; 4University of Texas Southwestern Medical Center, Frisco, TX
Introduction: Primary Biliary Cholangitis (PBC) affects women of all racial and economic backgrounds and can lead to progressive liver damage and hepatic decompensation. Limited data exist regarding healthcare disparities and second-line therapy use in safety-net settings. We aimed to compare stages at diagnosis, biochemical responses, second-line therapy initiation rates, and clinical outcomes between patients at a safety-net hospital (SNH) and a tertiary care hospital (TCH) system.
Methods: We conducted a retrospective cohort study reviewing 240 adult patients diagnosed with PBC from 2015-2024 at a SNH (n=120) and a TCH (n=120) in Dallas, Texas. Data included demographics, laboratory values (alkaline phosphatase, bilirubin, albumin), insurance status, and therapy utilization. Outcomes measured were UDCA biochemical response rates, second-line therapy initiation, and hepatic complications. Statistical analyses included chi-square for categorical variables and T-test for continuous variables.
Results: Patients at the SNH were of similar age to those at TCH (53.0 vs 54.6 years) but had significantly higher rates of uninsured or Medicaid status (63% vs. 8.3%; p < 0.001), were predominantly Hispanic (78.7% vs. 15.0%, p < 0.001) and had AMA-negative disease diagnosed by biopsy more frequently (32.7% vs. 4.2% < 0.001). These patients were more likely to receive ursodeoxycholic acid (99.1% vs. 94.1%, p = 0.04), but also had a higher rate of cirrhosis at diagnosis (26.9% vs. 7.5%, p < 0.0009), higher alkaline phosphatase (280 vs 206 IU/L, p = 0.03) and lower albumin (3.7 vs 4.2 mg/dL, p < 0.001) at 1 year. 72.2% of patients at the SNH met Toronto criteria based on alkaline phosphatase at one year after baseline visit. Patients at the TCH who met criteria for second line therapy were more likely to receive second line therapy with obeticholic acid or fenofibrate (14/19 vs. 10/40, p = 0.02). However, when excluding the patients who had already decompensated the difference was not significant (82% vs 50%). Patients not receiving second-line therapy had trend toward increased hepatic decompensation (37.8% vs. 30.8%).
Discussion: Significant disparities in PBC management exist between SNH and TCH highlighted by more severe disease, with lower biochemical response rates, and increased financial barriers. In spite of these challenges, access to ursodeoxycholic acid and second line therapies is similar between the hospital systems.
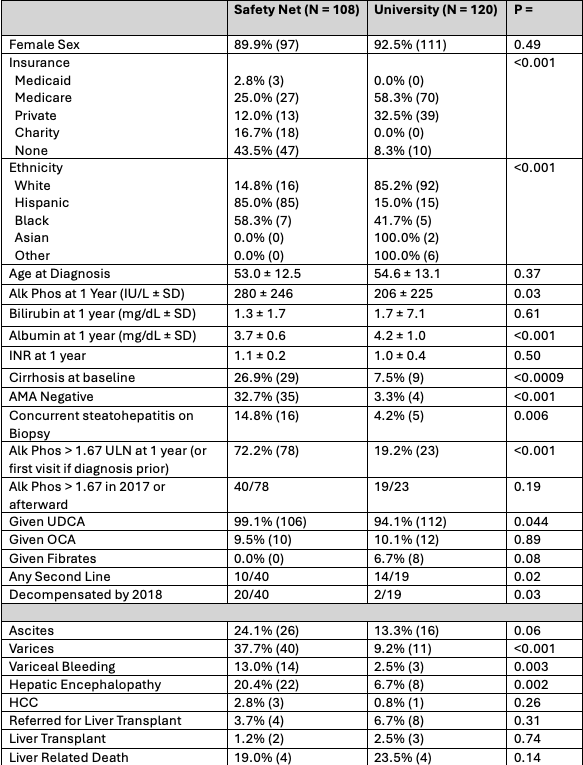
Figure: Table 1: Baseline characteristics and clinical outcomes comparing safety net and university patient populations.
Disclosures:
Meena Tadros indicated no relevant financial relationships.
Prajwal Gowda indicated no relevant financial relationships.
Maryln Mayo indicated no relevant financial relationships.
Mark Pedersen indicated no relevant financial relationships.
Saiabhiroop Govindu indicated no relevant financial relationships.
Meena M. Tadros, MD1, Prajwal Gowda, MD2, Maryln J. Mayo, MD3, Mark R. Pedersen, MD3, Saiabhiroop R. Govindu, BS4. P3644 - Primary Biliary Cholangitis: Second-Line Treatment and Outcomes at a Safety Net vs Tertiary Care Hospital Systems, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Pennsylvania, Philadelphia, PA; 2University of California San Francisco, San Francisco, CA; 3University of Texas Southwestern Medical Center, Dallas, TX; 4University of Texas Southwestern Medical Center, Frisco, TX
Introduction: Primary Biliary Cholangitis (PBC) affects women of all racial and economic backgrounds and can lead to progressive liver damage and hepatic decompensation. Limited data exist regarding healthcare disparities and second-line therapy use in safety-net settings. We aimed to compare stages at diagnosis, biochemical responses, second-line therapy initiation rates, and clinical outcomes between patients at a safety-net hospital (SNH) and a tertiary care hospital (TCH) system.
Methods: We conducted a retrospective cohort study reviewing 240 adult patients diagnosed with PBC from 2015-2024 at a SNH (n=120) and a TCH (n=120) in Dallas, Texas. Data included demographics, laboratory values (alkaline phosphatase, bilirubin, albumin), insurance status, and therapy utilization. Outcomes measured were UDCA biochemical response rates, second-line therapy initiation, and hepatic complications. Statistical analyses included chi-square for categorical variables and T-test for continuous variables.
Results: Patients at the SNH were of similar age to those at TCH (53.0 vs 54.6 years) but had significantly higher rates of uninsured or Medicaid status (63% vs. 8.3%; p < 0.001), were predominantly Hispanic (78.7% vs. 15.0%, p < 0.001) and had AMA-negative disease diagnosed by biopsy more frequently (32.7% vs. 4.2% < 0.001). These patients were more likely to receive ursodeoxycholic acid (99.1% vs. 94.1%, p = 0.04), but also had a higher rate of cirrhosis at diagnosis (26.9% vs. 7.5%, p < 0.0009), higher alkaline phosphatase (280 vs 206 IU/L, p = 0.03) and lower albumin (3.7 vs 4.2 mg/dL, p < 0.001) at 1 year. 72.2% of patients at the SNH met Toronto criteria based on alkaline phosphatase at one year after baseline visit. Patients at the TCH who met criteria for second line therapy were more likely to receive second line therapy with obeticholic acid or fenofibrate (14/19 vs. 10/40, p = 0.02). However, when excluding the patients who had already decompensated the difference was not significant (82% vs 50%). Patients not receiving second-line therapy had trend toward increased hepatic decompensation (37.8% vs. 30.8%).
Discussion: Significant disparities in PBC management exist between SNH and TCH highlighted by more severe disease, with lower biochemical response rates, and increased financial barriers. In spite of these challenges, access to ursodeoxycholic acid and second line therapies is similar between the hospital systems.
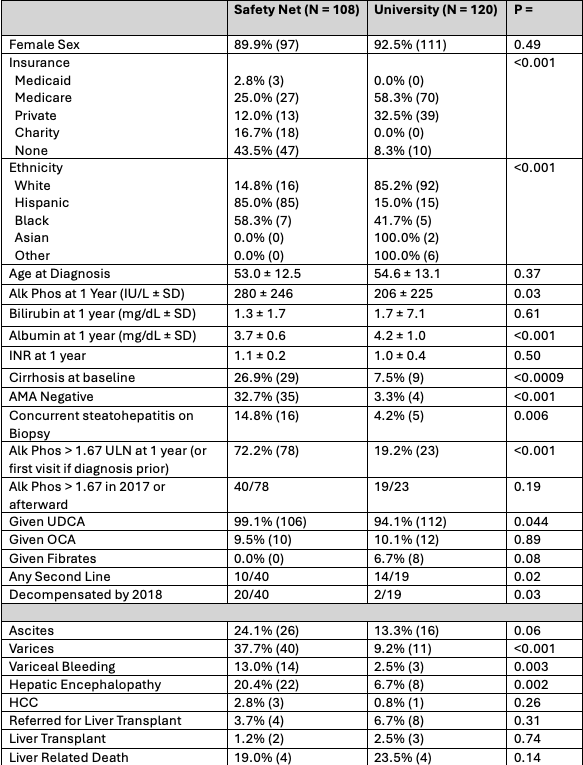
Figure: Table 1: Baseline characteristics and clinical outcomes comparing safety net and university patient populations.
Disclosures:
Meena Tadros indicated no relevant financial relationships.
Prajwal Gowda indicated no relevant financial relationships.
Maryln Mayo indicated no relevant financial relationships.
Mark Pedersen indicated no relevant financial relationships.
Saiabhiroop Govindu indicated no relevant financial relationships.
Meena M. Tadros, MD1, Prajwal Gowda, MD2, Maryln J. Mayo, MD3, Mark R. Pedersen, MD3, Saiabhiroop R. Govindu, BS4. P3644 - Primary Biliary Cholangitis: Second-Line Treatment and Outcomes at a Safety Net vs Tertiary Care Hospital Systems, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
