Monday Poster Session
Category: Liver
P3637 - Differential Overall Mortality and Healthcare Utilization for Liver Transplant Recipients by Regional, Hospital and Insurance Characteristics: Analysis of 47,175 Liver Transplant Recipients
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- TA
Tarek Aboursheid, MD
MedStar Georgetown University Hospital, Washington, DC, USA
Washington, DC
Presenting Author(s)
Mhd Kutaiba Albuni, MD1, Tarek Abou Rashid, MD2, Mohammed Abu-Rumaileh, MD3, Bisher Sawaf, MD4, Amine Rakab, MD5, Muhamad Hijazi, MD6, Aya Akhras, MD7, Elias Battikh, MD8, Muaz Alsabbagh, MD9, Yusuf Omar Hallak, MD3, Monica Tincopa, MD10
1Department of Internal Medicine, TriHealth Inc., Cincinnati, Cincinnati, OH; 2MedStar Georgetown University Hospital, Washington, DC, USA, Washington, DC; 3The University of Toledo, Toledo, OH; 4University of Toledo Medical Center, Toledo, OH; 5Division of Medical Education, Weill Cornell Medicine, Doha, Ad Dawhah, Qatar; 6TriHealth, Cincinnati, OH; 7HCA Florida Aventura Hospital, Aventura, FL; 8John H. Stroger, Jr. Hospital of Cook County, Toledo, OH; 9Detroit Medical Center/Wayne State University, Cleveland, OH; 10UCSD, San Diego, CA
Introduction: Liver transplantation (LT) is a lifesaving procedure for patients with end-stage liver disease. However, disparities in LT outcomes persist, resulting in barriers to health equity. The aim of this study was to evaluate associations of demographic, socioeconomic and hospital characteristics on post-LT outcomes including overall mortality and measures of healthcare utilization
Methods: We conducted a retrospective analysis of the National Inpatient Sample (NIS) database to identify adult LT recipients using ICD-10 coding. Demographic data, medical comorbidities, hospital characteristics, and socioeconomic indicators were examined. Outcomes included overall mortality, length of hospital stay (LOS), and total hospital charges (TOTCHG). Univariate and multivariate linear and logistic regression with propensity score matching assessed associations of covariates with outcomes of interest.
Results: A total of 47,175 LT recipients were identified. The mean age (±SE) was 59.1 (±0.48) years, with 63.1% male sex, 67.4% White and 15.9% Hispanic ethnicity. Multivariate analysis showed that overall mortality was significantly associated with age (OR 1.04, 95% CI 1.03-1.05), teaching hospitals (OR 0.68, 95% CI 0.51-0.91), comorbidity index (OR 1.39, 95% CI 1.33-1.45), insurance type (OR 0.77, 95% CI 0.66-0.90), and hospital location (OR 0.59 , 95% CI 0.38-0.91). Both length of stay (LOS) and total hospital charges (TOTCHG) were significantly associated with comorbidity burden (LOS β = +0.75 days, TOTCHG β = +$9,784; both p < 0.001). Insurance status significantly influenced outcomes, with Medicaid patients showing a markedly higher risk of overall mortality (OR: 9.78, p=0.003) and prolonged hospital stays. Regional variations in outcomes were also noted, with some regions demonstrating better survival rates and lower healthcare costs.
Discussion: Long term overall mortality and healthcare utilization post-LT are independently impacted by hospital characteristics, region and insurance type, posing potential barriers to health equity for this population. Characterizing underlying drivers of these disparate outcomes are urgently needed to ensure optimal healthcare outcomes and minimize healthcare costs.
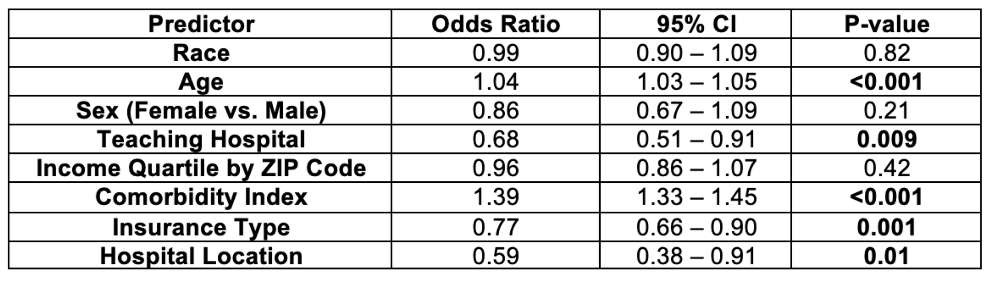
Figure: Table: Multivariate analysis showing predictors of overall mortality for liver transplant patients.
Disclosures:
Mhd Kutaiba Albuni indicated no relevant financial relationships.
Tarek Abou Rashid indicated no relevant financial relationships.
Mohammed Abu-Rumaileh indicated no relevant financial relationships.
Bisher Sawaf indicated no relevant financial relationships.
Amine Rakab indicated no relevant financial relationships.
Muhamad Hijazi indicated no relevant financial relationships.
Aya Akhras indicated no relevant financial relationships.
Elias Battikh indicated no relevant financial relationships.
Muaz Alsabbagh indicated no relevant financial relationships.
Yusuf Omar Hallak indicated no relevant financial relationships.
Monica Tincopa indicated no relevant financial relationships.
Mhd Kutaiba Albuni, MD1, Tarek Abou Rashid, MD2, Mohammed Abu-Rumaileh, MD3, Bisher Sawaf, MD4, Amine Rakab, MD5, Muhamad Hijazi, MD6, Aya Akhras, MD7, Elias Battikh, MD8, Muaz Alsabbagh, MD9, Yusuf Omar Hallak, MD3, Monica Tincopa, MD10. P3637 - Differential Overall Mortality and Healthcare Utilization for Liver Transplant Recipients by Regional, Hospital and Insurance Characteristics: Analysis of 47,175 Liver Transplant Recipients, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Department of Internal Medicine, TriHealth Inc., Cincinnati, Cincinnati, OH; 2MedStar Georgetown University Hospital, Washington, DC, USA, Washington, DC; 3The University of Toledo, Toledo, OH; 4University of Toledo Medical Center, Toledo, OH; 5Division of Medical Education, Weill Cornell Medicine, Doha, Ad Dawhah, Qatar; 6TriHealth, Cincinnati, OH; 7HCA Florida Aventura Hospital, Aventura, FL; 8John H. Stroger, Jr. Hospital of Cook County, Toledo, OH; 9Detroit Medical Center/Wayne State University, Cleveland, OH; 10UCSD, San Diego, CA
Introduction: Liver transplantation (LT) is a lifesaving procedure for patients with end-stage liver disease. However, disparities in LT outcomes persist, resulting in barriers to health equity. The aim of this study was to evaluate associations of demographic, socioeconomic and hospital characteristics on post-LT outcomes including overall mortality and measures of healthcare utilization
Methods: We conducted a retrospective analysis of the National Inpatient Sample (NIS) database to identify adult LT recipients using ICD-10 coding. Demographic data, medical comorbidities, hospital characteristics, and socioeconomic indicators were examined. Outcomes included overall mortality, length of hospital stay (LOS), and total hospital charges (TOTCHG). Univariate and multivariate linear and logistic regression with propensity score matching assessed associations of covariates with outcomes of interest.
Results: A total of 47,175 LT recipients were identified. The mean age (±SE) was 59.1 (±0.48) years, with 63.1% male sex, 67.4% White and 15.9% Hispanic ethnicity. Multivariate analysis showed that overall mortality was significantly associated with age (OR 1.04, 95% CI 1.03-1.05), teaching hospitals (OR 0.68, 95% CI 0.51-0.91), comorbidity index (OR 1.39, 95% CI 1.33-1.45), insurance type (OR 0.77, 95% CI 0.66-0.90), and hospital location (OR 0.59 , 95% CI 0.38-0.91). Both length of stay (LOS) and total hospital charges (TOTCHG) were significantly associated with comorbidity burden (LOS β = +0.75 days, TOTCHG β = +$9,784; both p < 0.001). Insurance status significantly influenced outcomes, with Medicaid patients showing a markedly higher risk of overall mortality (OR: 9.78, p=0.003) and prolonged hospital stays. Regional variations in outcomes were also noted, with some regions demonstrating better survival rates and lower healthcare costs.
Discussion: Long term overall mortality and healthcare utilization post-LT are independently impacted by hospital characteristics, region and insurance type, posing potential barriers to health equity for this population. Characterizing underlying drivers of these disparate outcomes are urgently needed to ensure optimal healthcare outcomes and minimize healthcare costs.
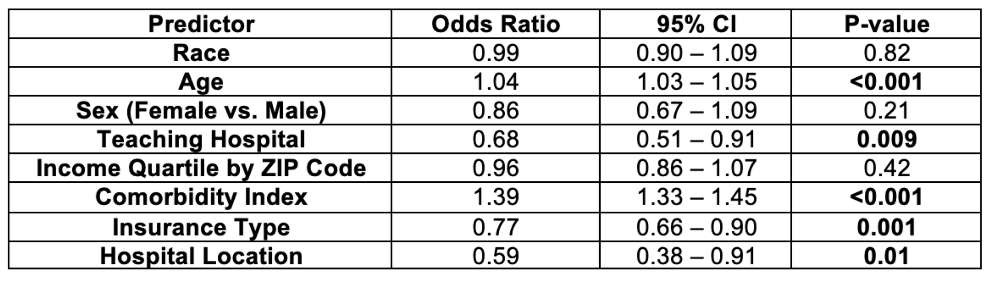
Figure: Table: Multivariate analysis showing predictors of overall mortality for liver transplant patients.
Disclosures:
Mhd Kutaiba Albuni indicated no relevant financial relationships.
Tarek Abou Rashid indicated no relevant financial relationships.
Mohammed Abu-Rumaileh indicated no relevant financial relationships.
Bisher Sawaf indicated no relevant financial relationships.
Amine Rakab indicated no relevant financial relationships.
Muhamad Hijazi indicated no relevant financial relationships.
Aya Akhras indicated no relevant financial relationships.
Elias Battikh indicated no relevant financial relationships.
Muaz Alsabbagh indicated no relevant financial relationships.
Yusuf Omar Hallak indicated no relevant financial relationships.
Monica Tincopa indicated no relevant financial relationships.
Mhd Kutaiba Albuni, MD1, Tarek Abou Rashid, MD2, Mohammed Abu-Rumaileh, MD3, Bisher Sawaf, MD4, Amine Rakab, MD5, Muhamad Hijazi, MD6, Aya Akhras, MD7, Elias Battikh, MD8, Muaz Alsabbagh, MD9, Yusuf Omar Hallak, MD3, Monica Tincopa, MD10. P3637 - Differential Overall Mortality and Healthcare Utilization for Liver Transplant Recipients by Regional, Hospital and Insurance Characteristics: Analysis of 47,175 Liver Transplant Recipients, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
