Monday Poster Session
Category: Liver
P3634 - Clinical Outcomes of GLP-1 Agonists on Patients With Compensated Cirrhosis and Type 2 Diabetes Mellitus: A Propensity Score-Matched Study Demonstrating a Reduction in Decompensated Cirrhosis From a Multinetwork Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Tinsae Anebo, MD (he/him/his)
Thomas Jefferson University
Philadelphia, PA
Presenting Author(s)
Tinsae Anebo, MD1, Laith Alomari, MD1, Karecia Byfield, MBBS2, Phuuwadith Wattanachayakul, MD3, Ghideon Ezaz, MD1
1Thomas Jefferson University, Philadelphia, PA; 2Jefferson Einstein Hospital, Philadelphia, PA; 3Albert Einstein Medical Center, Philadelphia, PA
Introduction: Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) play a key role in managing type 2 diabetes mellitus (T2DM), offering benefits in glycemic control, weight loss, and cardiovascular risk reduction.While their efficacy is well-established in non-cirrhotic populations, data on their impact in cirrhotic patients remain limited.This study evaluates the association between GLP-1 RA therapy and the risk of decompensation in cirrhotic patients with T2DM.
Methods: We used the US Collaborative Network-Trinetx database to identify patients diagnosed with diabetes mellitus and liver cirrhosis between January 1, 2015, and December 31, 2024. Decompensated cirrhosis was defined as cirrhosis with esophageal variceal bleeding, ascites, hepatic encephalopathy, or jaundice, while compensated cirrhosis included cases without these complications. Exclusion criteria included missing age/sex data, age < 18, type 1 diabetes, dialysis, decompensated cirrhosis, liver failure, liver transplant, or hepatocellular carcinoma (HCC). The comorbid date was the first record of coexisting T2DM and compensated cirrhosis. Patients initiating GLP-1 RAs after this date were classified as users, while those never exposed were non-users. Propensity score matching (1:1) ensured cohort comparability based on age, ethnicity, obesity, dyslipidemia, hypertension, chronic kidney disease, and medications (oral antidiabetics, insulin, antihypertensives, statins, and aspirin). Outcomes assessed included all-cause mortality, hospitalization, ischemic heart disease, stroke/TIA, heart failure, hepatic encephalopathy, ascites, variceal bleeding, jaundice, and HCC. Generalized linear models were used to estimate associations, with results presented as risk ratios/hazard ratios and 95% confidence intervals. A p-value < 0.05 was considered significant.
Results: Following propensity score matching, each cohort included 29,397 patients. GLP-1 RA use in compensated cirrhotic patients with T2DM was associated with significantly lower risks of all-cause mortality, hospitalization, ischemic heart disease, stroke/TIA, heart failure, hepatic encephalopathy, ascites, and jaundice. However, reductions in variceal bleeding (p = 0.0534) and HCC (p = 0.0884) were not statistically significant.
Discussion: GLP-1 RA use in cirrhotic patients with T2DM was linked to significant reductions in key liver-related outcomes. These findings suggest that GLP-1 RAs may offer substantial benefits in this high-risk population, warranting further prospective studies.
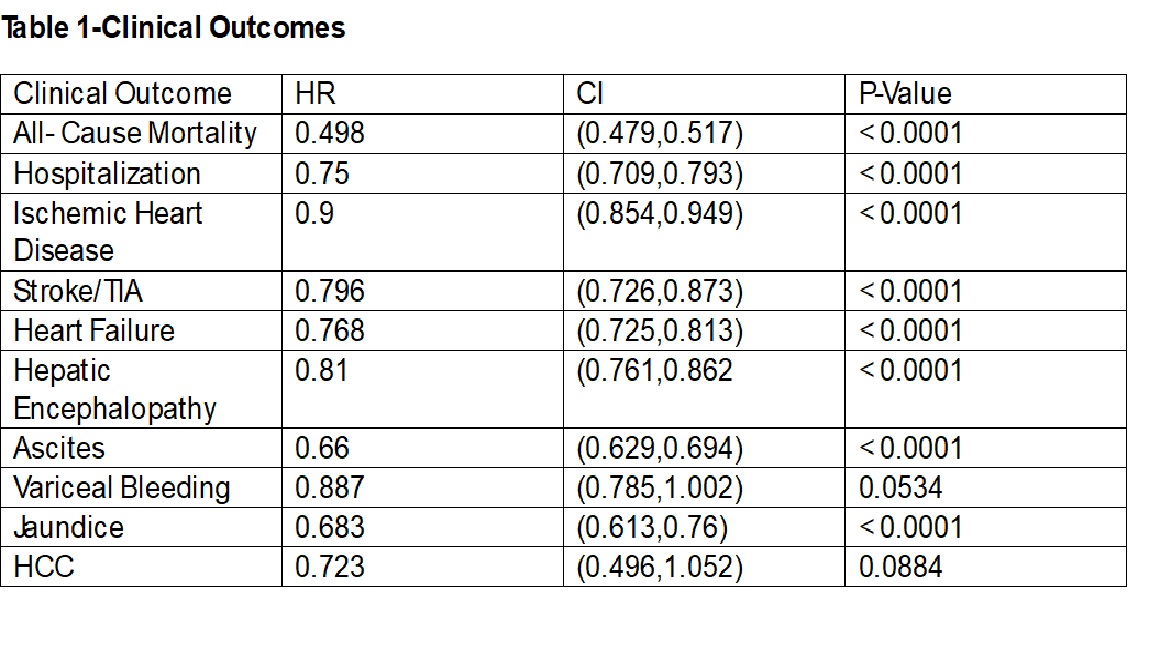
Figure: Table 1-CLINCAL OUTCOMES
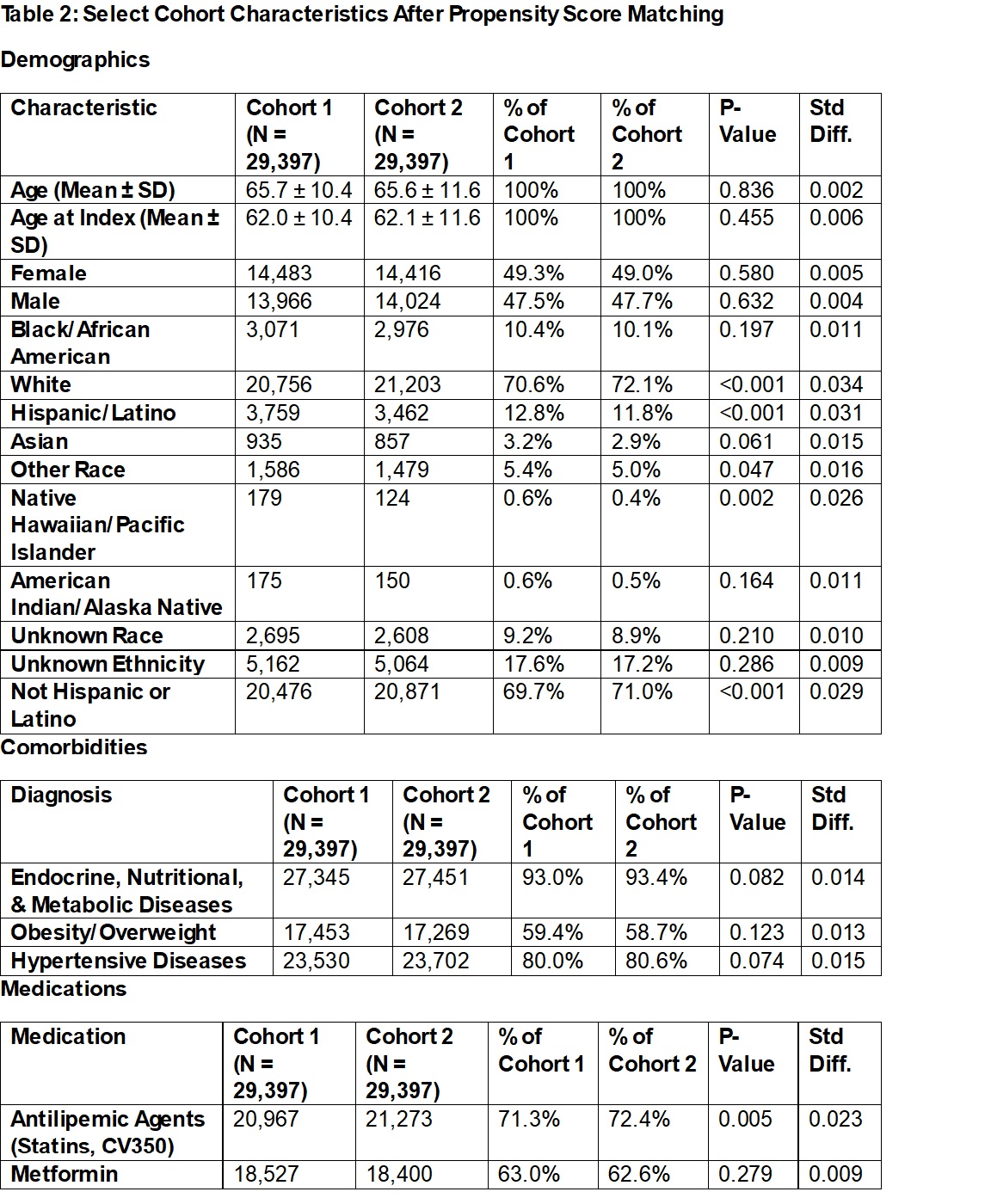
Figure: Table 2-Select Cohort Characteristic's
Disclosures:
Tinsae Anebo indicated no relevant financial relationships.
Laith Alomari indicated no relevant financial relationships.
Karecia Byfield indicated no relevant financial relationships.
Phuuwadith Wattanachayakul indicated no relevant financial relationships.
Ghideon Ezaz indicated no relevant financial relationships.
Tinsae Anebo, MD1, Laith Alomari, MD1, Karecia Byfield, MBBS2, Phuuwadith Wattanachayakul, MD3, Ghideon Ezaz, MD1. P3634 - Clinical Outcomes of GLP-1 Agonists on Patients With Compensated Cirrhosis and Type 2 Diabetes Mellitus: A Propensity Score-Matched Study Demonstrating a Reduction in Decompensated Cirrhosis From a Multinetwork Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Thomas Jefferson University, Philadelphia, PA; 2Jefferson Einstein Hospital, Philadelphia, PA; 3Albert Einstein Medical Center, Philadelphia, PA
Introduction: Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) play a key role in managing type 2 diabetes mellitus (T2DM), offering benefits in glycemic control, weight loss, and cardiovascular risk reduction.While their efficacy is well-established in non-cirrhotic populations, data on their impact in cirrhotic patients remain limited.This study evaluates the association between GLP-1 RA therapy and the risk of decompensation in cirrhotic patients with T2DM.
Methods: We used the US Collaborative Network-Trinetx database to identify patients diagnosed with diabetes mellitus and liver cirrhosis between January 1, 2015, and December 31, 2024. Decompensated cirrhosis was defined as cirrhosis with esophageal variceal bleeding, ascites, hepatic encephalopathy, or jaundice, while compensated cirrhosis included cases without these complications. Exclusion criteria included missing age/sex data, age < 18, type 1 diabetes, dialysis, decompensated cirrhosis, liver failure, liver transplant, or hepatocellular carcinoma (HCC). The comorbid date was the first record of coexisting T2DM and compensated cirrhosis. Patients initiating GLP-1 RAs after this date were classified as users, while those never exposed were non-users. Propensity score matching (1:1) ensured cohort comparability based on age, ethnicity, obesity, dyslipidemia, hypertension, chronic kidney disease, and medications (oral antidiabetics, insulin, antihypertensives, statins, and aspirin). Outcomes assessed included all-cause mortality, hospitalization, ischemic heart disease, stroke/TIA, heart failure, hepatic encephalopathy, ascites, variceal bleeding, jaundice, and HCC. Generalized linear models were used to estimate associations, with results presented as risk ratios/hazard ratios and 95% confidence intervals. A p-value < 0.05 was considered significant.
Results: Following propensity score matching, each cohort included 29,397 patients. GLP-1 RA use in compensated cirrhotic patients with T2DM was associated with significantly lower risks of all-cause mortality, hospitalization, ischemic heart disease, stroke/TIA, heart failure, hepatic encephalopathy, ascites, and jaundice. However, reductions in variceal bleeding (p = 0.0534) and HCC (p = 0.0884) were not statistically significant.
Discussion: GLP-1 RA use in cirrhotic patients with T2DM was linked to significant reductions in key liver-related outcomes. These findings suggest that GLP-1 RAs may offer substantial benefits in this high-risk population, warranting further prospective studies.
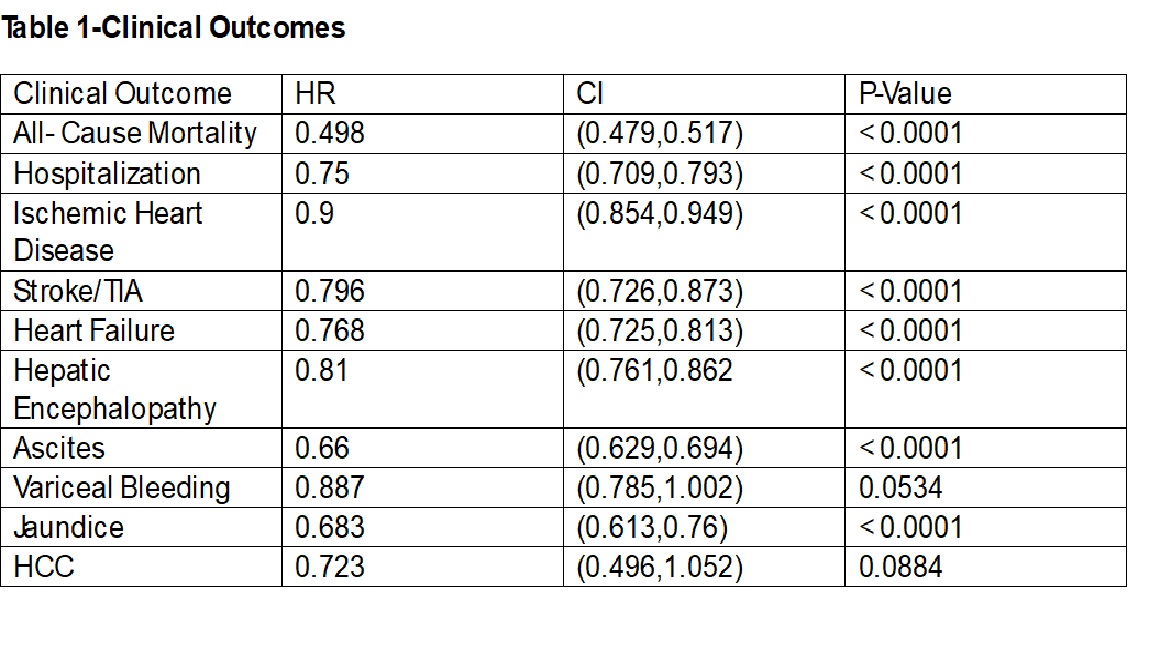
Figure: Table 1-CLINCAL OUTCOMES
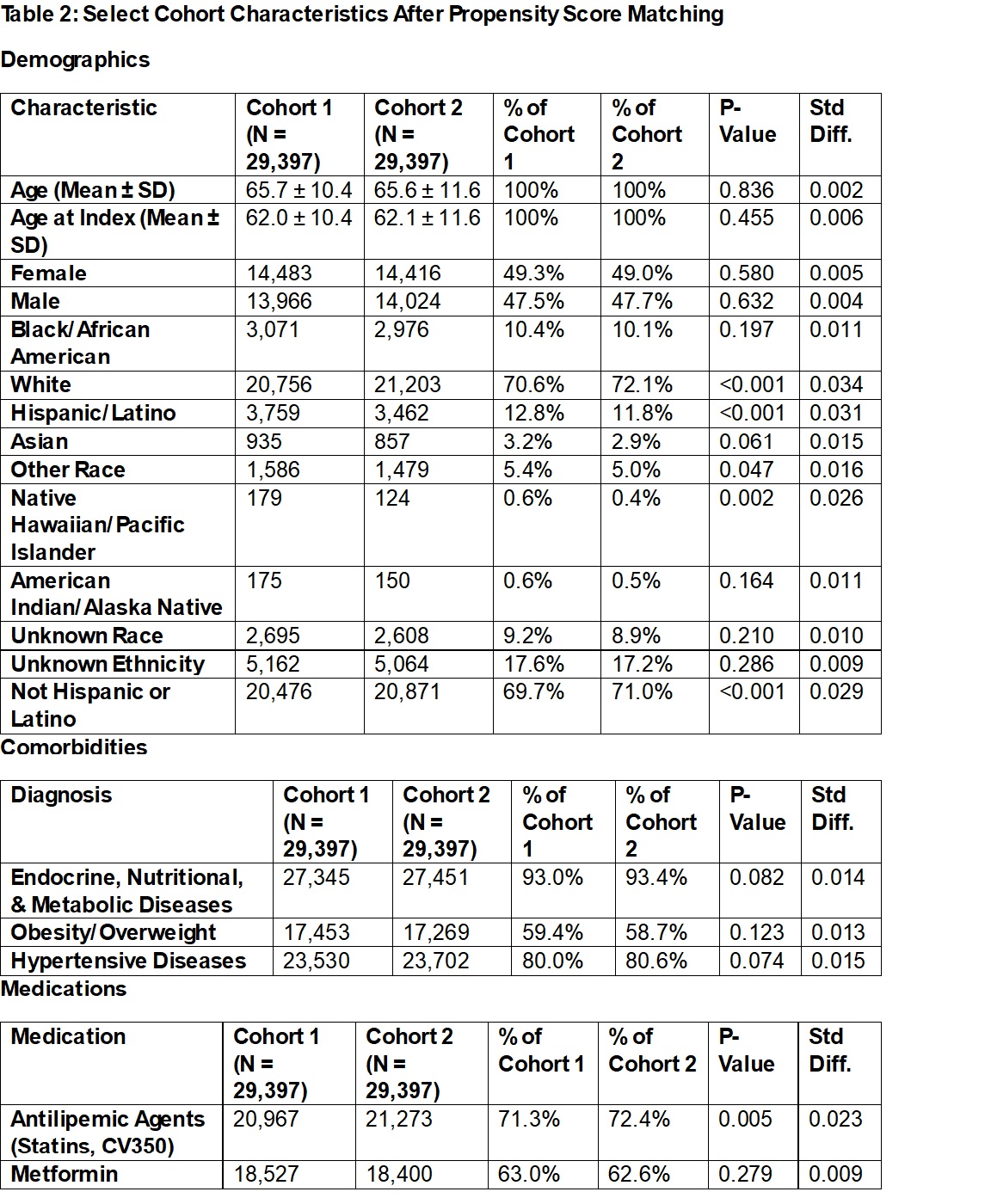
Figure: Table 2-Select Cohort Characteristic's
Disclosures:
Tinsae Anebo indicated no relevant financial relationships.
Laith Alomari indicated no relevant financial relationships.
Karecia Byfield indicated no relevant financial relationships.
Phuuwadith Wattanachayakul indicated no relevant financial relationships.
Ghideon Ezaz indicated no relevant financial relationships.
Tinsae Anebo, MD1, Laith Alomari, MD1, Karecia Byfield, MBBS2, Phuuwadith Wattanachayakul, MD3, Ghideon Ezaz, MD1. P3634 - Clinical Outcomes of GLP-1 Agonists on Patients With Compensated Cirrhosis and Type 2 Diabetes Mellitus: A Propensity Score-Matched Study Demonstrating a Reduction in Decompensated Cirrhosis From a Multinetwork Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
