Monday Poster Session
Category: Liver
P3723 - A Standardized Cirrhosis Admission Order Set Improves Guideline-Directed Inpatient Care
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- LL
Laura Lavette, MD (she/her/hers)
University of Virginia Medical Center
Charlottesville, VA
Presenting Author(s)
Laura Lavette, MD1, Hannah Laird, MD1, Ashley Chipoletti, 2, Mira Sridharan, MD3, Jessica Dreicer, MD1, Andrew Barros, MD1, Zachary Henry, MD1
1University of Virginia Medical Center, Charlottesville, VA; 2University of Virginia School of Medicine, Charlottesville, VA; 3Boston Medical Center, Boston, MA
Introduction: The cirrhosis patient population is vulnerable with high hospitalization and readmission rates. We developed and implemented a cirrhosis order set with the goal of standardizing the admission process, encouraging guideline-directed medical care, and optimizing inpatient management of cirrhosis.
Methods: We used evidence-based practice guidelines to construct a cirrhosis order set for providers to use at time of admission. Our order set was created as a stand-alone order set and also embedded in the “General Admission” order set. We collected data on a cohort of patients with cirrhosis admitted to a general medicine service between February 2024 and January 2025. We divided our patients into two groups: those with and without order set use. Order set use was left to the discretion of the admitting team. Our primary outcomes included rates of 1) low sodium, high protein diet orders, and 2) diagnostic paracentesis performed during admission. Secondary outcomes included 7- and 30-day Emergency Department (ED) visits and readmissions.
Results: Overall, the order set was used in 45% (182/405) of admissions to our general medicine service for patients with cirrhosis. There was no significant difference in age or gender between groups. The “order set” group had significantly higher Model for End-Stage Liver Disease (MELD) scores, liver-related admissions, and prevalence of decompensated cirrhosis. Low sodium, high protein diet orders during admission were significantly higher in the order set group (93% vs 37%, p=0.001; 91% vs 37%, p=0.001). Similarly, performance of diagnostic paracentesis was more common in the order set group and done significantly earlier in the admission (46% vs 26%, p=0.001; 460 min vs 1210 min, p=0.03). There were no significant differences in length of stay (LOS), need for ICU transfer, 7-day ED visits, or readmissions; however, patients in the “order set” group were less likely to present to the ED within 30 days of hospital discharge despite higher MELD scores (32% vs 46%, p=0.006).
Discussion: The increasing prevalence of liver disease and associated healthcare costs highlight opportunities for improvement in quality care. Our findings show that use of an order set can have a significant impact on guideline-directed inpatient management; specifically, improved rates of low sodium, high protein diet and diagnostic paracentesis during admission. Next steps should include standardization of the discharge process with the goal of improving LOS and readmission rates.
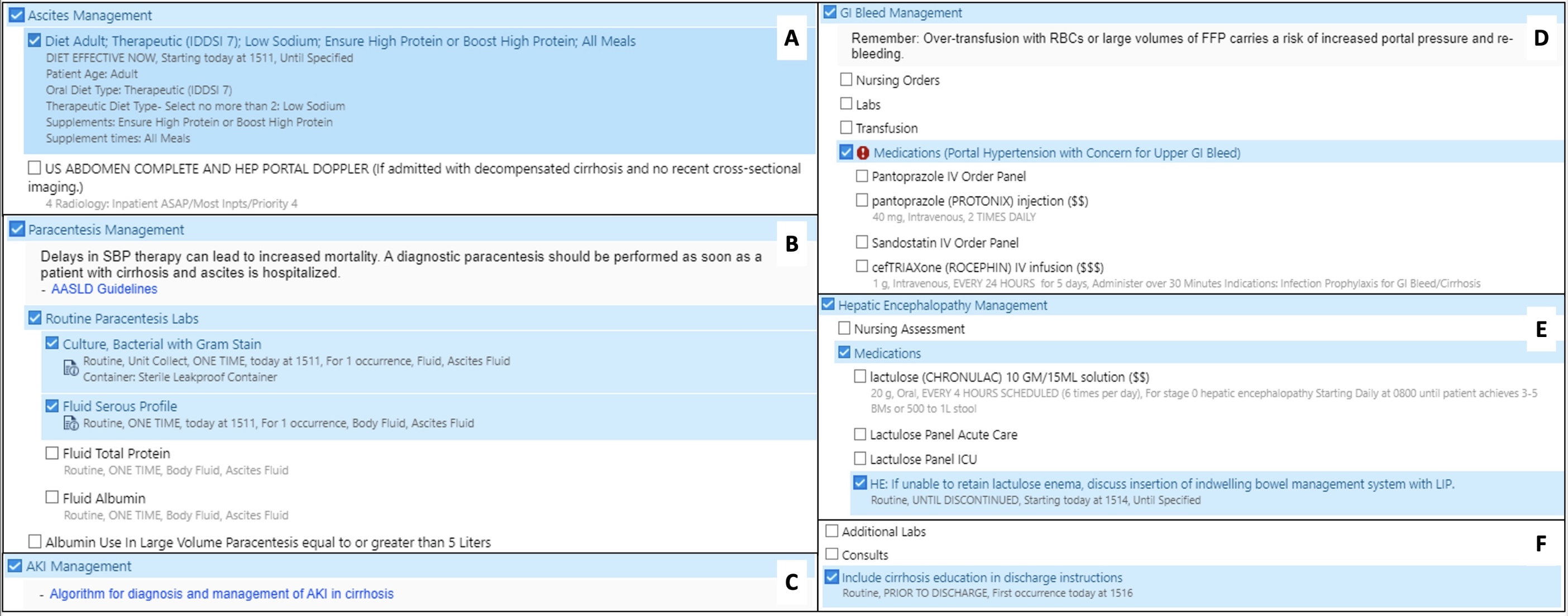
Figure: “Cirrhosis Management Panel” with categories including (A) ascites management, (B) paracentesis management, (C) acute kidney injury (AKI) management, (D) gastrointestinal bleed (GIB) management, (E) hepatic encephalopathy management, (F) labs, consults, and education.
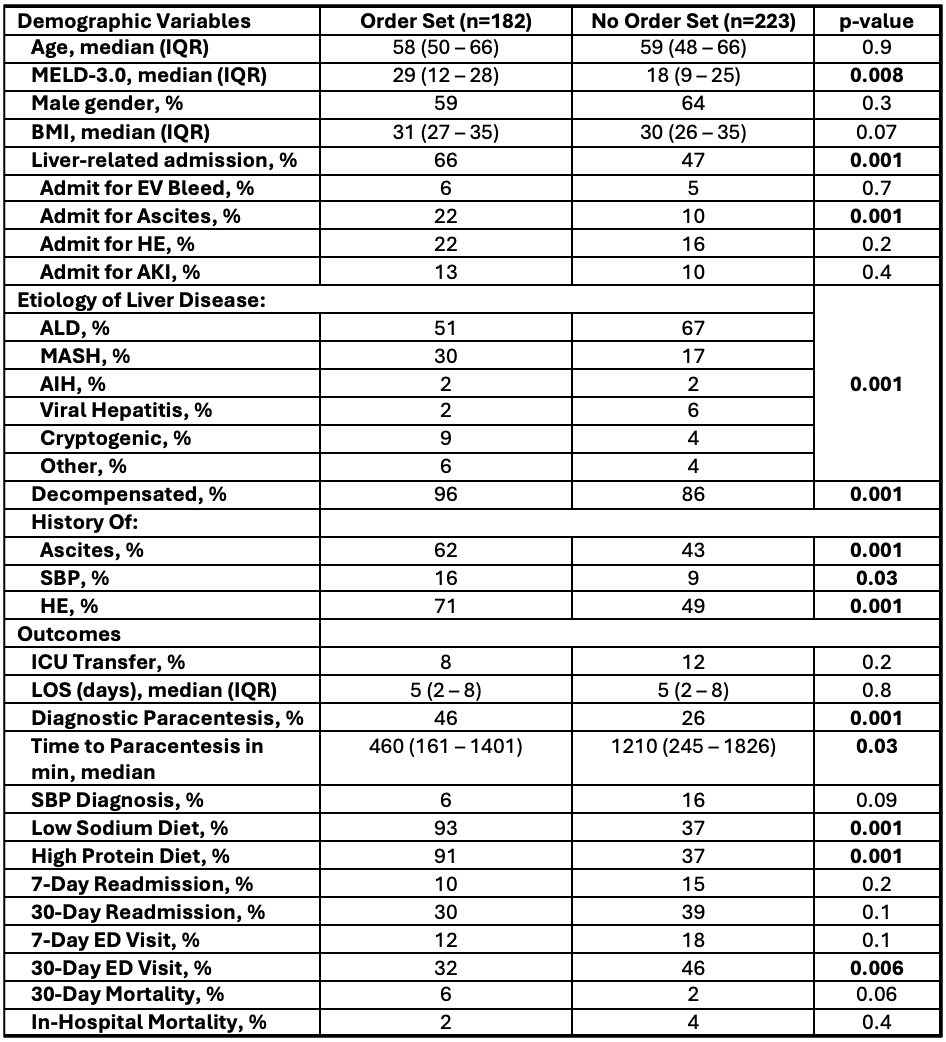
Figure: Demographic and outcome data between “Order Set” and “No Order Set” groups with associated p-values.
Disclosures:
Laura Lavette indicated no relevant financial relationships.
Hannah Laird indicated no relevant financial relationships.
Ashley Chipoletti indicated no relevant financial relationships.
Mira Sridharan indicated no relevant financial relationships.
Jessica Dreicer indicated no relevant financial relationships.
Andrew Barros indicated no relevant financial relationships.
Zachary Henry indicated no relevant financial relationships.
Laura Lavette, MD1, Hannah Laird, MD1, Ashley Chipoletti, 2, Mira Sridharan, MD3, Jessica Dreicer, MD1, Andrew Barros, MD1, Zachary Henry, MD1. P3723 - A Standardized Cirrhosis Admission Order Set Improves Guideline-Directed Inpatient Care, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Virginia Medical Center, Charlottesville, VA; 2University of Virginia School of Medicine, Charlottesville, VA; 3Boston Medical Center, Boston, MA
Introduction: The cirrhosis patient population is vulnerable with high hospitalization and readmission rates. We developed and implemented a cirrhosis order set with the goal of standardizing the admission process, encouraging guideline-directed medical care, and optimizing inpatient management of cirrhosis.
Methods: We used evidence-based practice guidelines to construct a cirrhosis order set for providers to use at time of admission. Our order set was created as a stand-alone order set and also embedded in the “General Admission” order set. We collected data on a cohort of patients with cirrhosis admitted to a general medicine service between February 2024 and January 2025. We divided our patients into two groups: those with and without order set use. Order set use was left to the discretion of the admitting team. Our primary outcomes included rates of 1) low sodium, high protein diet orders, and 2) diagnostic paracentesis performed during admission. Secondary outcomes included 7- and 30-day Emergency Department (ED) visits and readmissions.
Results: Overall, the order set was used in 45% (182/405) of admissions to our general medicine service for patients with cirrhosis. There was no significant difference in age or gender between groups. The “order set” group had significantly higher Model for End-Stage Liver Disease (MELD) scores, liver-related admissions, and prevalence of decompensated cirrhosis. Low sodium, high protein diet orders during admission were significantly higher in the order set group (93% vs 37%, p=0.001; 91% vs 37%, p=0.001). Similarly, performance of diagnostic paracentesis was more common in the order set group and done significantly earlier in the admission (46% vs 26%, p=0.001; 460 min vs 1210 min, p=0.03). There were no significant differences in length of stay (LOS), need for ICU transfer, 7-day ED visits, or readmissions; however, patients in the “order set” group were less likely to present to the ED within 30 days of hospital discharge despite higher MELD scores (32% vs 46%, p=0.006).
Discussion: The increasing prevalence of liver disease and associated healthcare costs highlight opportunities for improvement in quality care. Our findings show that use of an order set can have a significant impact on guideline-directed inpatient management; specifically, improved rates of low sodium, high protein diet and diagnostic paracentesis during admission. Next steps should include standardization of the discharge process with the goal of improving LOS and readmission rates.
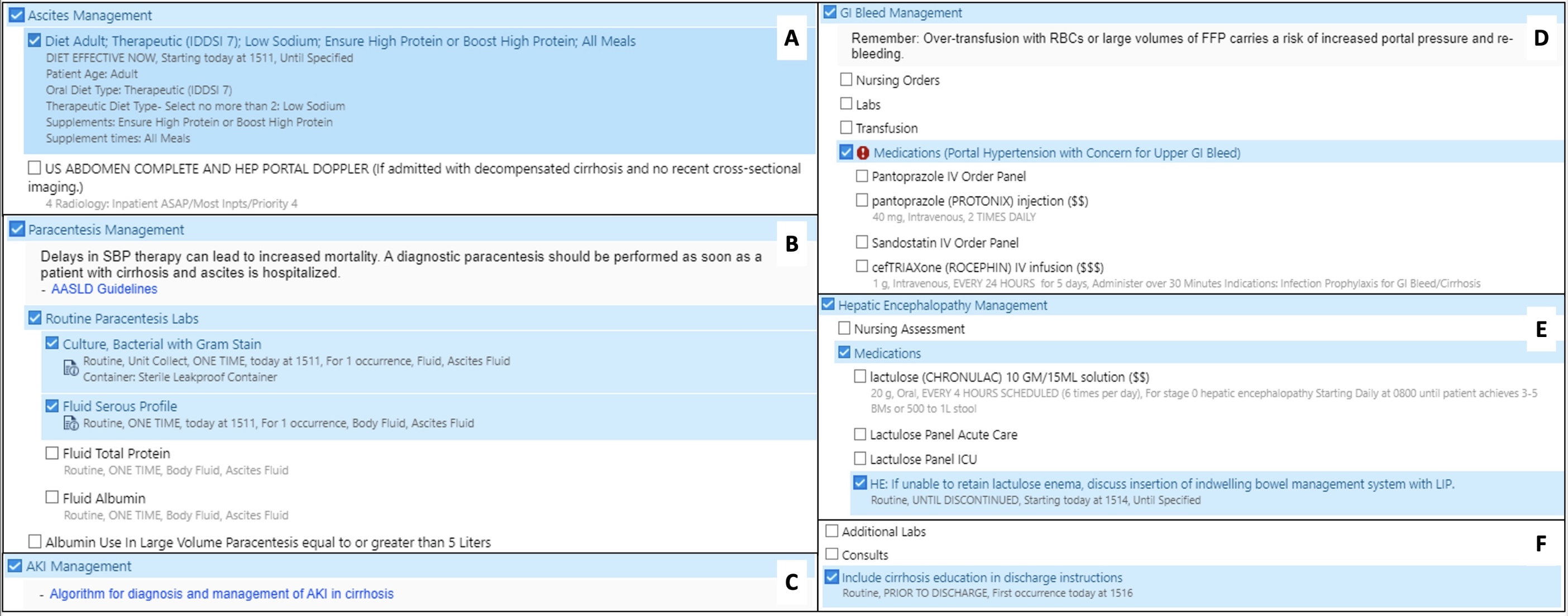
Figure: “Cirrhosis Management Panel” with categories including (A) ascites management, (B) paracentesis management, (C) acute kidney injury (AKI) management, (D) gastrointestinal bleed (GIB) management, (E) hepatic encephalopathy management, (F) labs, consults, and education.
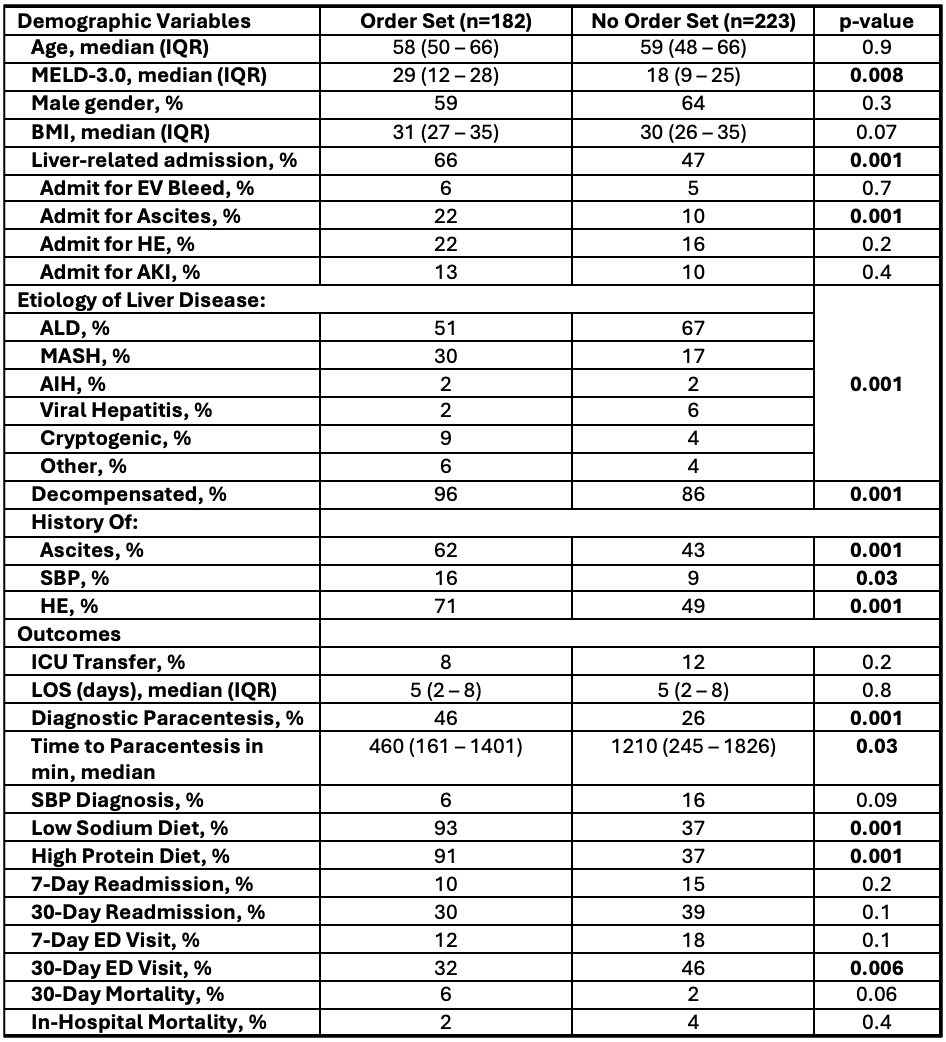
Figure: Demographic and outcome data between “Order Set” and “No Order Set” groups with associated p-values.
Disclosures:
Laura Lavette indicated no relevant financial relationships.
Hannah Laird indicated no relevant financial relationships.
Ashley Chipoletti indicated no relevant financial relationships.
Mira Sridharan indicated no relevant financial relationships.
Jessica Dreicer indicated no relevant financial relationships.
Andrew Barros indicated no relevant financial relationships.
Zachary Henry indicated no relevant financial relationships.
Laura Lavette, MD1, Hannah Laird, MD1, Ashley Chipoletti, 2, Mira Sridharan, MD3, Jessica Dreicer, MD1, Andrew Barros, MD1, Zachary Henry, MD1. P3723 - A Standardized Cirrhosis Admission Order Set Improves Guideline-Directed Inpatient Care, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
