Monday Poster Session
Category: Liver
P3709 - Racial Disparities in Hepatorenal Syndrome Incidence and Outcomes Among Cirrhotic Patients: Insights From a Large Retrospective Cohort Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Komlan Guedze, MD (he/him/his)
Franciscan Health
Olympia Fields, IL
Presenting Author(s)
Kojo-Frimpong B. Awuah, MD1, Komlan E.B. Guedze, MD2, Mutabi Erasmus, MD1, Chidera Onwuzo, MD3, Tyrell Daniel, MD4, Rashid Abdel-Razeq, MD5
1Allegheny Health Network, Pittsburgh, PA; 2Franciscan Alliance, Olympia Fields, IL; 3State University of New York Upstate Medical University, Syracuse, NY; 4Sentara Northern Virginia Medical Center, Woodbridge, VA; 5Cleveland Clinic Foundation, Cleveland, OH
Introduction: Hepatorenal syndrome (HRS) represents a life-threatening complication in cirrhosis, with significant racial disparities in incidence and outcomes. Black and Native American patients face disproportionate barriers to advanced liver care, contributing to suboptimal outcomes. This study investigates racial and ethnic disparities in HRS among cirrhotic patients, aiming to identify contributing factors and underscore the need for targeted interventions to improve equity in healthcare delivery.
Methods: Using the TriNetX database, we conducted a retrospective analysis of 34,885 cirrhotic patients diagnosed with HRS between 2000 and 2024. Patients were stratified by race/ethnicity (American Indian or Alaska Native, Asian, Black, Native Hawaiian or Other Pacific Islander, White, and Other). HRS incidence was calculated as the proportion of new cases among cirrhotic patients. Chi-square tests were employed to examine racial disparities, adjusting for confounders such as age, sex, and liver disease severity. Mortality and survival data from existing literature provided contextual insights into outcome disparities.
Results: Among cirrhotic patients, 5.6% developed HRS, with the highest incidence observed in American Indian or Alaska Native patients (9.35%), followed by White (6.10%) and Other Race (6.21%) groups. Black and American Indian patients exhibited disproportionately poor survival rates post-HRS diagnosis (p < 0.05), even after controlling for age and comorbid conditions , reflecting systemic barriers, including reduced access to nephrology care and renal replacement therapies . Socioeconomic challenges and healthcare inequities were identified as key contributors to these disparities.
Discussion: This study highlights stark racial disparities in the incidence and outcomes of HRS among cirrhotic patients, emphasizing the disproportionate burden on American Indian and Black populations. Addressing these inequities requires systemic reforms to improve early detection, expand access to renal replacement therapies, and mitigate socioeconomic barriers. These findings underscore the critical need for equity-focused interventions to enhance care delivery and outcomes for marginalized populations.
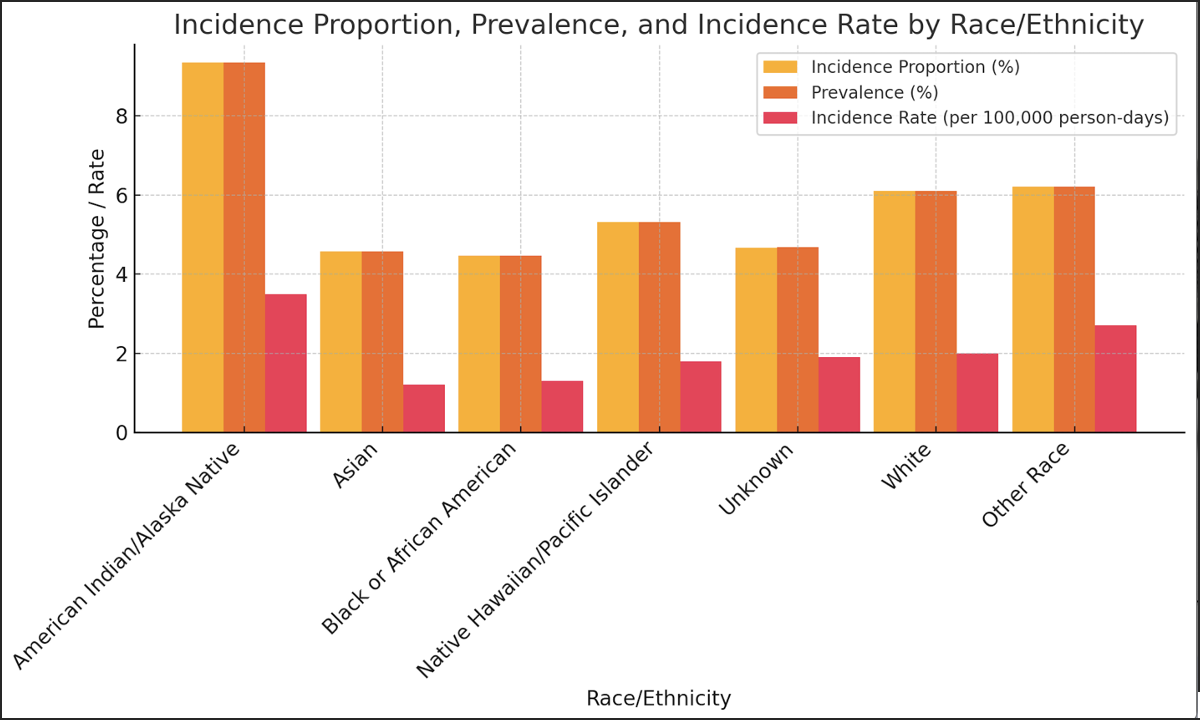
Figure: Figure 1: Incidence Proportion, Prevalence, and Incidence Rate by Race/Ethnicity
This bar graph compares the incidence proportion (%), prevalence (%), and incidence rate (per 100,000 person-days) across racial and ethnic groups. American Indian/Alaska Native individuals have the highest values for incidence proportion (9.35%) and prevalence (9.35%), along with the highest incidence rate (35 cases per 100,000 person-days). In contrast, Asian individuals exhibit the lowest incidence proportion (4.57%), prevalence (4.57%), and incidence rate (12 cases per 100,000 person-days). These results underscore significant racial and ethnic disparities in disease metrics.
Disclosures:
Kojo-Frimpong B. Awuah indicated no relevant financial relationships.
Komlan Guedze indicated no relevant financial relationships.
Mutabi Erasmus indicated no relevant financial relationships.
Chidera Onwuzo indicated no relevant financial relationships.
Tyrell Daniel indicated no relevant financial relationships.
Rashid Abdel-Razeq indicated no relevant financial relationships.
Kojo-Frimpong B. Awuah, MD1, Komlan E.B. Guedze, MD2, Mutabi Erasmus, MD1, Chidera Onwuzo, MD3, Tyrell Daniel, MD4, Rashid Abdel-Razeq, MD5. P3709 - Racial Disparities in Hepatorenal Syndrome Incidence and Outcomes Among Cirrhotic Patients: Insights From a Large Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Allegheny Health Network, Pittsburgh, PA; 2Franciscan Alliance, Olympia Fields, IL; 3State University of New York Upstate Medical University, Syracuse, NY; 4Sentara Northern Virginia Medical Center, Woodbridge, VA; 5Cleveland Clinic Foundation, Cleveland, OH
Introduction: Hepatorenal syndrome (HRS) represents a life-threatening complication in cirrhosis, with significant racial disparities in incidence and outcomes. Black and Native American patients face disproportionate barriers to advanced liver care, contributing to suboptimal outcomes. This study investigates racial and ethnic disparities in HRS among cirrhotic patients, aiming to identify contributing factors and underscore the need for targeted interventions to improve equity in healthcare delivery.
Methods: Using the TriNetX database, we conducted a retrospective analysis of 34,885 cirrhotic patients diagnosed with HRS between 2000 and 2024. Patients were stratified by race/ethnicity (American Indian or Alaska Native, Asian, Black, Native Hawaiian or Other Pacific Islander, White, and Other). HRS incidence was calculated as the proportion of new cases among cirrhotic patients. Chi-square tests were employed to examine racial disparities, adjusting for confounders such as age, sex, and liver disease severity. Mortality and survival data from existing literature provided contextual insights into outcome disparities.
Results: Among cirrhotic patients, 5.6% developed HRS, with the highest incidence observed in American Indian or Alaska Native patients (9.35%), followed by White (6.10%) and Other Race (6.21%) groups. Black and American Indian patients exhibited disproportionately poor survival rates post-HRS diagnosis (p < 0.05), even after controlling for age and comorbid conditions , reflecting systemic barriers, including reduced access to nephrology care and renal replacement therapies . Socioeconomic challenges and healthcare inequities were identified as key contributors to these disparities.
Discussion: This study highlights stark racial disparities in the incidence and outcomes of HRS among cirrhotic patients, emphasizing the disproportionate burden on American Indian and Black populations. Addressing these inequities requires systemic reforms to improve early detection, expand access to renal replacement therapies, and mitigate socioeconomic barriers. These findings underscore the critical need for equity-focused interventions to enhance care delivery and outcomes for marginalized populations.
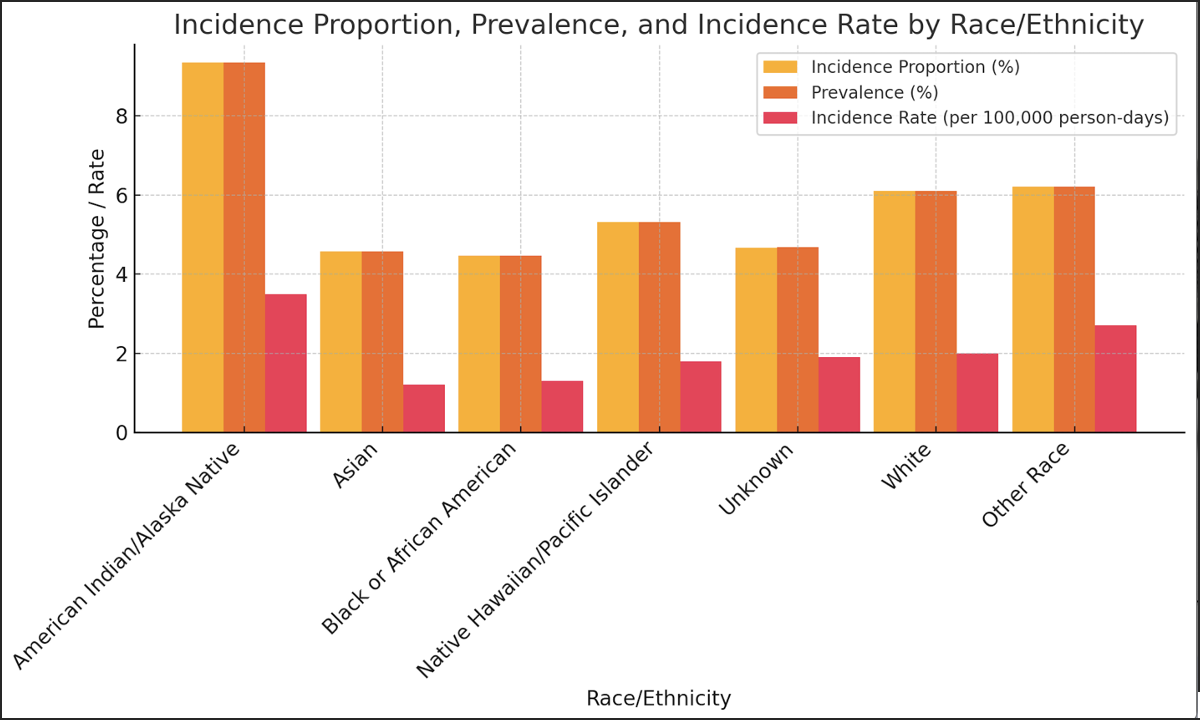
Figure: Figure 1: Incidence Proportion, Prevalence, and Incidence Rate by Race/Ethnicity
This bar graph compares the incidence proportion (%), prevalence (%), and incidence rate (per 100,000 person-days) across racial and ethnic groups. American Indian/Alaska Native individuals have the highest values for incidence proportion (9.35%) and prevalence (9.35%), along with the highest incidence rate (35 cases per 100,000 person-days). In contrast, Asian individuals exhibit the lowest incidence proportion (4.57%), prevalence (4.57%), and incidence rate (12 cases per 100,000 person-days). These results underscore significant racial and ethnic disparities in disease metrics.
Disclosures:
Kojo-Frimpong B. Awuah indicated no relevant financial relationships.
Komlan Guedze indicated no relevant financial relationships.
Mutabi Erasmus indicated no relevant financial relationships.
Chidera Onwuzo indicated no relevant financial relationships.
Tyrell Daniel indicated no relevant financial relationships.
Rashid Abdel-Razeq indicated no relevant financial relationships.
Kojo-Frimpong B. Awuah, MD1, Komlan E.B. Guedze, MD2, Mutabi Erasmus, MD1, Chidera Onwuzo, MD3, Tyrell Daniel, MD4, Rashid Abdel-Razeq, MD5. P3709 - Racial Disparities in Hepatorenal Syndrome Incidence and Outcomes Among Cirrhotic Patients: Insights From a Large Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
