Monday Poster Session
Category: Liver
P3786 - Trends, Burden and Impact of Infections on Outcomes in Patients With Alcoholic Hepatitis: A Nationwide Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- CS
Carol Singh, MBBS
Dayanand Medical College and Hospital
New Jersey, NJ
Presenting Author(s)
Carol Singh, MBBS1, Sampada Bhasker, MBBS2, Bipneet Singh, MD3, Rahul Chikatimalla, MBBS4, Mohammad Naseem, MBBS5, Vikash Kumar, MD6, Aalam Sohal, MD6, Nilofar Najafian, MD6
1Dayanand Medical College and Hospital, New Jersey, NJ; 2Punjab Institute of Medical Sciences, Jalandhar, Punjab, India; 3Henry Ford Jackson Hospital, Jackson, MI; 4Kamineni Institute of Medical Sciences, Narketpalle, Telangana, India; 5Maulana Azad Medical College, New Delhi, Delhi, India; 6Creighton University School of Medicine, Phoenix, AZ
Introduction: Alcoholic hepatitis (AH) is characterized by severe inflammation of the liver among patients with alcohol use. It is associated with immune dysfunction and increased susceptibility to developing infections. This study evaluates the trends, burden, and impact of infections on the clinical course of AH.
Methods: Data from the 2016-2022 National Inpatient Sample database were used to identify adult patients with AH. Patients were stratified into two groups: those with and without infections. We collected data on patient demographics, hepatitis B/C, liver-related decompensations, comorbidities, and clinical outcomes (in-hospital mortality, sepsis, shock, acute kidney injury (AKI), intensive care unit (ICU) stay and thrombotic events). Multivariate logistic/linear regression analysis was used to assess the impact of infections on these outcomes.
Results: Among the 917,345 patients with AH, 186,655 (20.3%) developed infections. The most frequent infections observed included urinary tract infections (UTI) (9.0%), hospital-acquired pneumonia (HAP) (6.0%) and skin/soft tissue infections (2.7%). Between 2016 to 2022, overall infection rates remained stable but increasing trends were observed in HAP and spontaneous bacterial peritonitis (SBP), while Clostridioides difficile infection (CDI) rates declined (Figure 1). Highest mortality was observed in patients with HAP (22.5%), followed by UTI (14.6%). Presence of infection was associated with increased rates of mortality (9.2% vs. 2.9%), sepsis (7.6% vs 3.7%), AKI (36.9 vs. 19.2%), ICU admissions (16.3% vs. 5.5%), pulmonary embolism (PE) (0.8% vs. 0.4%) and deep vein thrombosis (DVT) (1.5% vs 0.6%). After adjusting for confounding factors, patients with infections had higher odds of in-hospital mortality(aOR-1.84, 95% CI-1.75–1.95,p< 0.001), sepsis(aOR-1.87, 95% CI- 1.77–1.97, p< 0.001), AKI(aOR-1.78, 95% CI- 1.73–1.84, p< 0.001), ICU admissions(aOR-2.52, 95% CI-2.42–2.63, p< 0.001), PE(aOR-2.02, 95% CI-1.74–2.35, p< 0.001) DVT(aOR-2.39, 95% CI-2.13–2.70, p< 0.001), longer length of stay(adj. coefficient- 3.35 days, 95% CI-3.24- 3.45,p< 0.001) and higher hospitalization charges(adj. Coefficient- $38773.48, 95% CI-$37048.46-$40498.51, p< 0.001)(Table 1).
Discussion: The development of systemic infections in patients with AH leads to worse clinical outcomes. Early identification, management, and prevention are necessary to prevent adverse clinical outcomes and improve the overall prognosis of these patients.
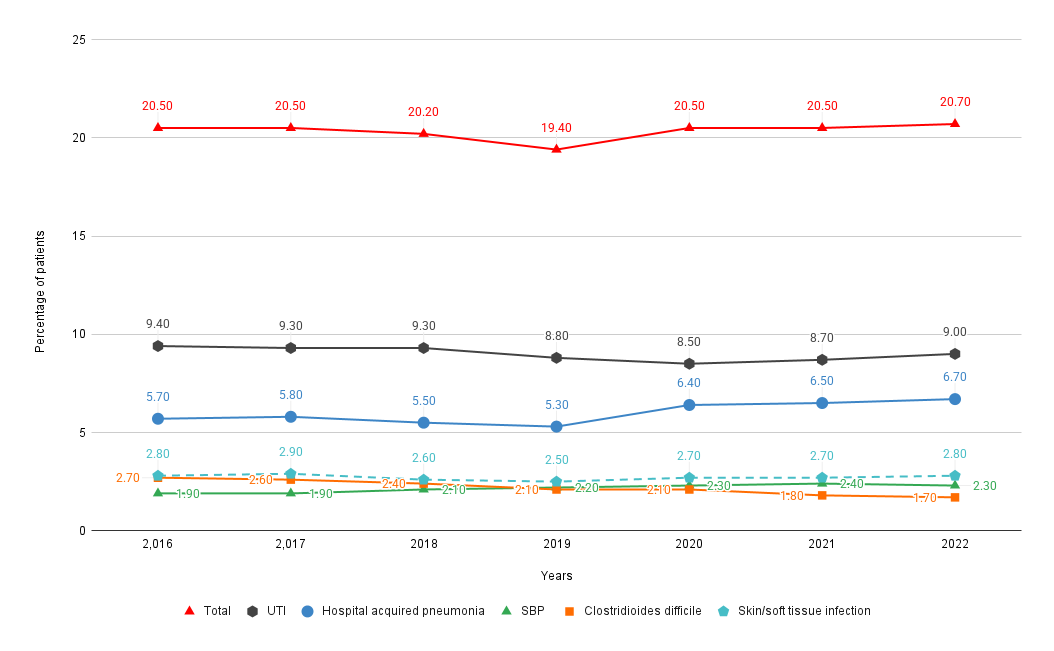
Figure: Figure 1. Rates of infections each year from 2016-2022.
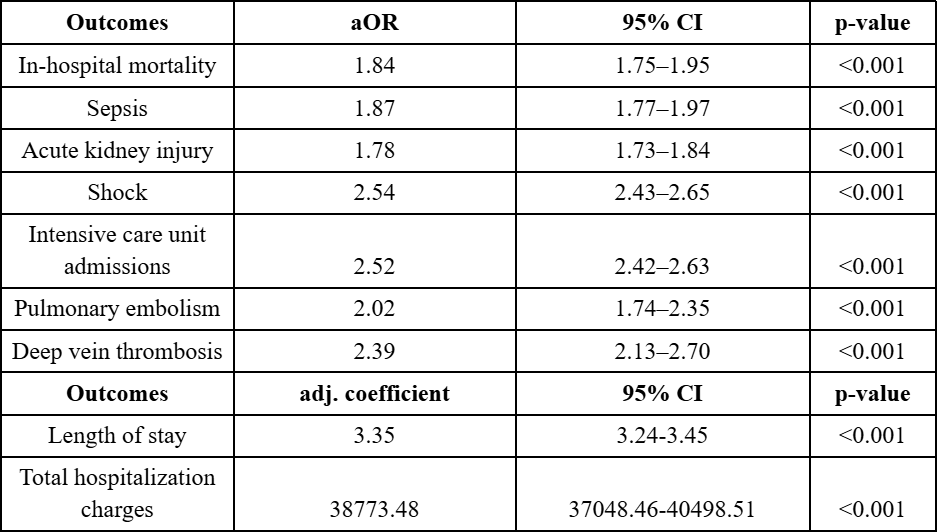
Figure: Table 1. Results of multivariate logistic regression, assessing the impact of infections on outcomes and resource utilization.
Disclosures:
Carol Singh indicated no relevant financial relationships.
Sampada Bhasker indicated no relevant financial relationships.
Bipneet Singh indicated no relevant financial relationships.
Rahul Chikatimalla indicated no relevant financial relationships.
Mohammad Naseem indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Aalam Sohal indicated no relevant financial relationships.
Nilofar Najafian indicated no relevant financial relationships.
Carol Singh, MBBS1, Sampada Bhasker, MBBS2, Bipneet Singh, MD3, Rahul Chikatimalla, MBBS4, Mohammad Naseem, MBBS5, Vikash Kumar, MD6, Aalam Sohal, MD6, Nilofar Najafian, MD6. P3786 - Trends, Burden and Impact of Infections on Outcomes in Patients With Alcoholic Hepatitis: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Dayanand Medical College and Hospital, New Jersey, NJ; 2Punjab Institute of Medical Sciences, Jalandhar, Punjab, India; 3Henry Ford Jackson Hospital, Jackson, MI; 4Kamineni Institute of Medical Sciences, Narketpalle, Telangana, India; 5Maulana Azad Medical College, New Delhi, Delhi, India; 6Creighton University School of Medicine, Phoenix, AZ
Introduction: Alcoholic hepatitis (AH) is characterized by severe inflammation of the liver among patients with alcohol use. It is associated with immune dysfunction and increased susceptibility to developing infections. This study evaluates the trends, burden, and impact of infections on the clinical course of AH.
Methods: Data from the 2016-2022 National Inpatient Sample database were used to identify adult patients with AH. Patients were stratified into two groups: those with and without infections. We collected data on patient demographics, hepatitis B/C, liver-related decompensations, comorbidities, and clinical outcomes (in-hospital mortality, sepsis, shock, acute kidney injury (AKI), intensive care unit (ICU) stay and thrombotic events). Multivariate logistic/linear regression analysis was used to assess the impact of infections on these outcomes.
Results: Among the 917,345 patients with AH, 186,655 (20.3%) developed infections. The most frequent infections observed included urinary tract infections (UTI) (9.0%), hospital-acquired pneumonia (HAP) (6.0%) and skin/soft tissue infections (2.7%). Between 2016 to 2022, overall infection rates remained stable but increasing trends were observed in HAP and spontaneous bacterial peritonitis (SBP), while Clostridioides difficile infection (CDI) rates declined (Figure 1). Highest mortality was observed in patients with HAP (22.5%), followed by UTI (14.6%). Presence of infection was associated with increased rates of mortality (9.2% vs. 2.9%), sepsis (7.6% vs 3.7%), AKI (36.9 vs. 19.2%), ICU admissions (16.3% vs. 5.5%), pulmonary embolism (PE) (0.8% vs. 0.4%) and deep vein thrombosis (DVT) (1.5% vs 0.6%). After adjusting for confounding factors, patients with infections had higher odds of in-hospital mortality(aOR-1.84, 95% CI-1.75–1.95,p< 0.001), sepsis(aOR-1.87, 95% CI- 1.77–1.97, p< 0.001), AKI(aOR-1.78, 95% CI- 1.73–1.84, p< 0.001), ICU admissions(aOR-2.52, 95% CI-2.42–2.63, p< 0.001), PE(aOR-2.02, 95% CI-1.74–2.35, p< 0.001) DVT(aOR-2.39, 95% CI-2.13–2.70, p< 0.001), longer length of stay(adj. coefficient- 3.35 days, 95% CI-3.24- 3.45,p< 0.001) and higher hospitalization charges(adj. Coefficient- $38773.48, 95% CI-$37048.46-$40498.51, p< 0.001)(Table 1).
Discussion: The development of systemic infections in patients with AH leads to worse clinical outcomes. Early identification, management, and prevention are necessary to prevent adverse clinical outcomes and improve the overall prognosis of these patients.
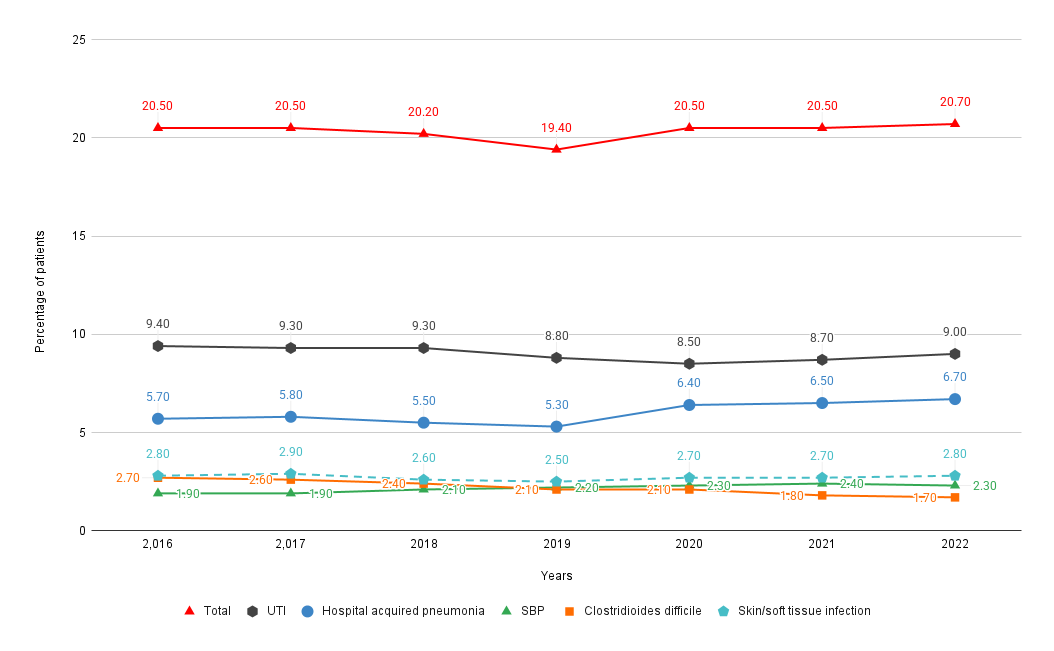
Figure: Figure 1. Rates of infections each year from 2016-2022.
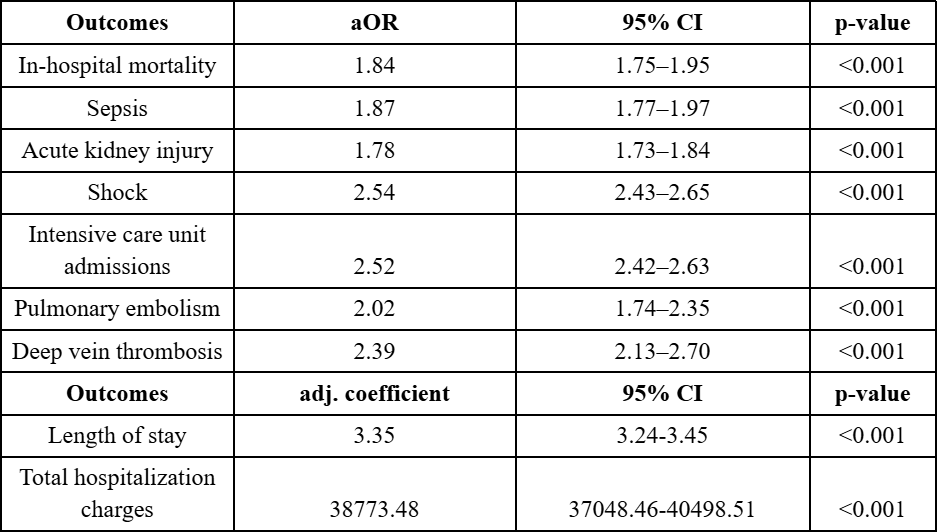
Figure: Table 1. Results of multivariate logistic regression, assessing the impact of infections on outcomes and resource utilization.
Disclosures:
Carol Singh indicated no relevant financial relationships.
Sampada Bhasker indicated no relevant financial relationships.
Bipneet Singh indicated no relevant financial relationships.
Rahul Chikatimalla indicated no relevant financial relationships.
Mohammad Naseem indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Aalam Sohal indicated no relevant financial relationships.
Nilofar Najafian indicated no relevant financial relationships.
Carol Singh, MBBS1, Sampada Bhasker, MBBS2, Bipneet Singh, MD3, Rahul Chikatimalla, MBBS4, Mohammad Naseem, MBBS5, Vikash Kumar, MD6, Aalam Sohal, MD6, Nilofar Najafian, MD6. P3786 - Trends, Burden and Impact of Infections on Outcomes in Patients With Alcoholic Hepatitis: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
