Monday Poster Session
Category: Liver
P3870 - Post Orthotopic Liver Transplant Anastomotic Bile Leak Causing Bilothorax
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Nina Gautam, BS
University of Arizona College of Medicine Phoenix
Phoenix, AZ
Presenting Author(s)
Nina Gautam, BS1, Matthew J. Schlichting, BS2, Austin Mineer, BS1, Leith Ghani, DO3, Majd Aboona, MD4, Emily Mallin, MD4, Mark Wong, MD1
1University of Arizona College of Medicine Phoenix, Phoenix, AZ; 2The University of Arizona College of Medicine – Phoenix, Phoenix, AZ; 3Banner University Medical Center- P, Phoenix, AZ; 4University of Arizona College of Medicine - Phoenix, Phoenix, AZ
Introduction: Pleural effusions are common after orthotopic liver transplantation, occurring in up to 95% of patients within the first postoperative week. Most are benign and resolve spontaneously. However, a persistent or complicated pleural effusion, particularly in the absence of pulmonary infection, warrants further evaluation. We present a rare case of bilothorax as a postoperative complication of liver transplant.
Case Description/
Methods: A 67-year-old male who received an orthotopic liver transplant (OLT) with extensive adhesiolysis, portal vein thrombectomy, and transdiaphragmatic right thoracentesis presented to the emergency department 3 months post transplant with symptomatic anemia with worsening lightheadedness, dyspnea, chills, and fatigue. Computed tomography angiography of the abdomen/pelvis demonstrated rim-enhancing fluid in the right lower chest, and a thoracostomy tube was placed on hospital day (HD) 1. Initial fluid studies showed a complicated exudative effusion. Cultures revealed Enterococcus faecium and Clostridium clostridioforme; appropriate antibiotics were initiated. The chest tube continued to have output of >150cc. In the absence of a clear source of infection such as pneumonia, a pleural fluid-to-serum bilirubin ratio was obtained and found to be 1.6, indicative of bilothorax. Magnetic resonance cholangiopancreatography on HD5 showed discontinuity between the donor common bile duct (CBD) and native CBD, suggestive of high-grade anastomotic stricture. Percutaneous transhepatic cholangiogram performed on HD8 did not reveal stricture, but rather demonstrated delayed filling of the native CBD and anastomotic leak with a fistulous connection to the duodenum and superior extension suggestive of a pleurobiliary fistula. It was determined this was the most likely cause of the patient’s bilothorax. A 10Fr internal/external biliary drain was placed through the native CBD.
Discussion: Persistent pleural effusions, a common complication post OLT, are typically exudative by Light’s criteria. Bilothorax from a pleurobiliary fistula is a much rarer complication, with few cases documented in the literature. Imaging to assess biliary anastomotic patency and bilirubin pleural studies should be considered, particularly in patients with prior diaphragmatic manipulation.
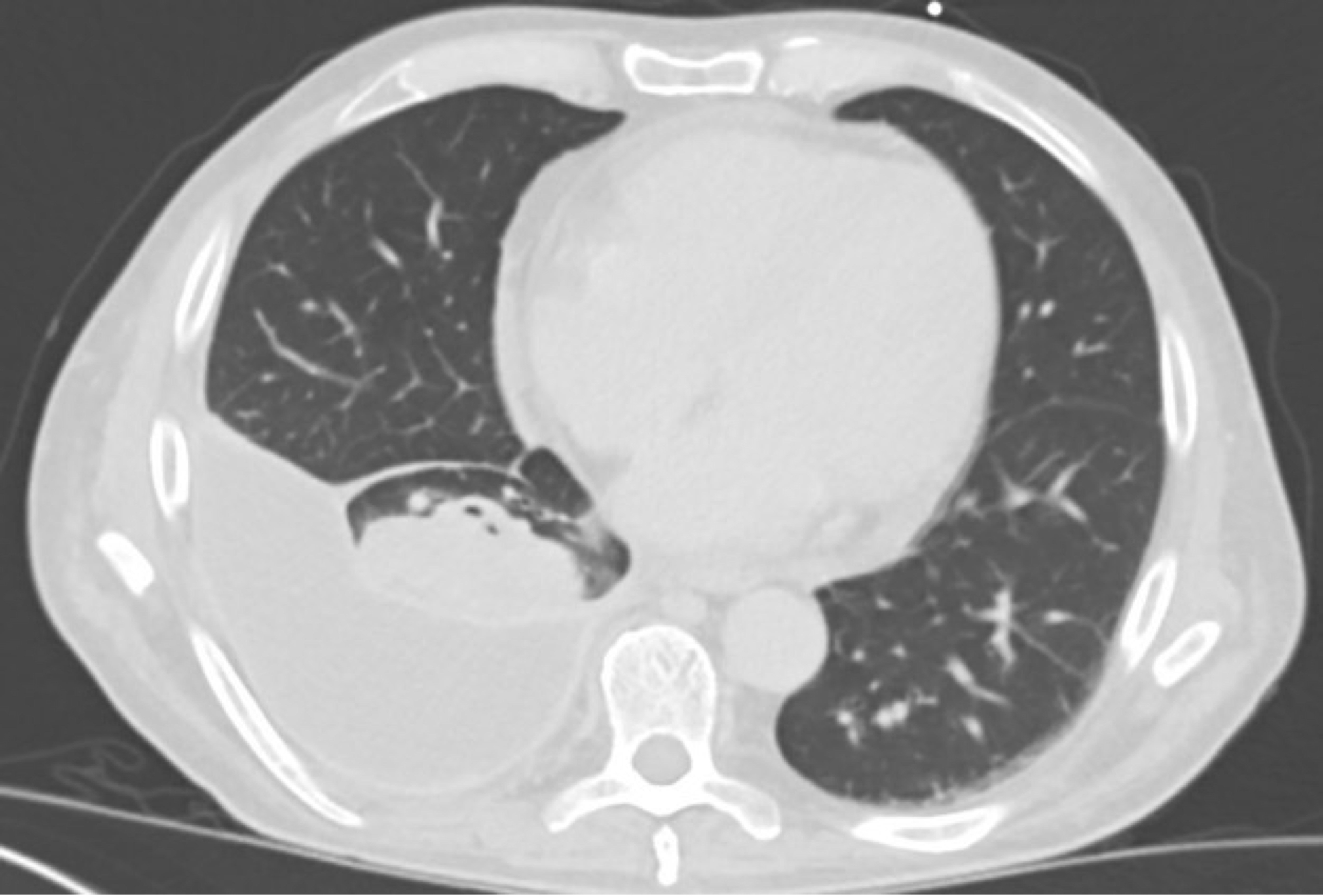
Figure: CTA of Abdomen/Pelvis revealing significant right pleural effusion.

Figure: Anastomotic bile leak with superior extension and fistula to duodenum.
Disclosures:
Nina Gautam indicated no relevant financial relationships.
Matthew Schlichting: Pfizer Inc. – Stock-publicly held company(excluding mutual/index funds). Viatris Inc. – Stock-publicly held company(excluding mutual/index funds).
Austin Mineer indicated no relevant financial relationships.
Leith Ghani indicated no relevant financial relationships.
Majd Aboona indicated no relevant financial relationships.
Emily Mallin indicated no relevant financial relationships.
Mark Wong indicated no relevant financial relationships.
Nina Gautam, BS1, Matthew J. Schlichting, BS2, Austin Mineer, BS1, Leith Ghani, DO3, Majd Aboona, MD4, Emily Mallin, MD4, Mark Wong, MD1. P3870 - Post Orthotopic Liver Transplant Anastomotic Bile Leak Causing Bilothorax, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Arizona College of Medicine Phoenix, Phoenix, AZ; 2The University of Arizona College of Medicine – Phoenix, Phoenix, AZ; 3Banner University Medical Center- P, Phoenix, AZ; 4University of Arizona College of Medicine - Phoenix, Phoenix, AZ
Introduction: Pleural effusions are common after orthotopic liver transplantation, occurring in up to 95% of patients within the first postoperative week. Most are benign and resolve spontaneously. However, a persistent or complicated pleural effusion, particularly in the absence of pulmonary infection, warrants further evaluation. We present a rare case of bilothorax as a postoperative complication of liver transplant.
Case Description/
Methods: A 67-year-old male who received an orthotopic liver transplant (OLT) with extensive adhesiolysis, portal vein thrombectomy, and transdiaphragmatic right thoracentesis presented to the emergency department 3 months post transplant with symptomatic anemia with worsening lightheadedness, dyspnea, chills, and fatigue. Computed tomography angiography of the abdomen/pelvis demonstrated rim-enhancing fluid in the right lower chest, and a thoracostomy tube was placed on hospital day (HD) 1. Initial fluid studies showed a complicated exudative effusion. Cultures revealed Enterococcus faecium and Clostridium clostridioforme; appropriate antibiotics were initiated. The chest tube continued to have output of >150cc. In the absence of a clear source of infection such as pneumonia, a pleural fluid-to-serum bilirubin ratio was obtained and found to be 1.6, indicative of bilothorax. Magnetic resonance cholangiopancreatography on HD5 showed discontinuity between the donor common bile duct (CBD) and native CBD, suggestive of high-grade anastomotic stricture. Percutaneous transhepatic cholangiogram performed on HD8 did not reveal stricture, but rather demonstrated delayed filling of the native CBD and anastomotic leak with a fistulous connection to the duodenum and superior extension suggestive of a pleurobiliary fistula. It was determined this was the most likely cause of the patient’s bilothorax. A 10Fr internal/external biliary drain was placed through the native CBD.
Discussion: Persistent pleural effusions, a common complication post OLT, are typically exudative by Light’s criteria. Bilothorax from a pleurobiliary fistula is a much rarer complication, with few cases documented in the literature. Imaging to assess biliary anastomotic patency and bilirubin pleural studies should be considered, particularly in patients with prior diaphragmatic manipulation.
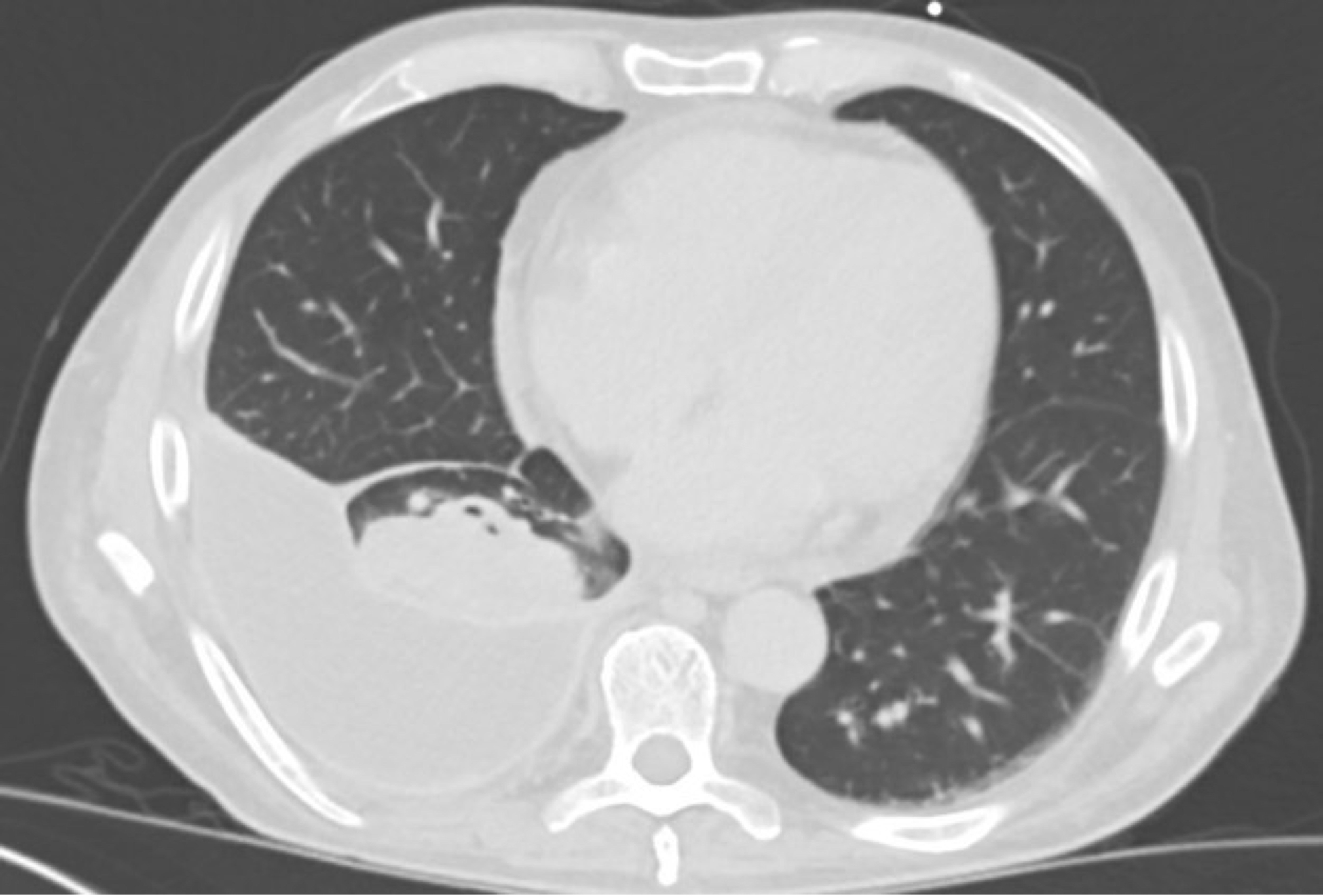
Figure: CTA of Abdomen/Pelvis revealing significant right pleural effusion.

Figure: Anastomotic bile leak with superior extension and fistula to duodenum.
Disclosures:
Nina Gautam indicated no relevant financial relationships.
Matthew Schlichting: Pfizer Inc. – Stock-publicly held company(excluding mutual/index funds). Viatris Inc. – Stock-publicly held company(excluding mutual/index funds).
Austin Mineer indicated no relevant financial relationships.
Leith Ghani indicated no relevant financial relationships.
Majd Aboona indicated no relevant financial relationships.
Emily Mallin indicated no relevant financial relationships.
Mark Wong indicated no relevant financial relationships.
Nina Gautam, BS1, Matthew J. Schlichting, BS2, Austin Mineer, BS1, Leith Ghani, DO3, Majd Aboona, MD4, Emily Mallin, MD4, Mark Wong, MD1. P3870 - Post Orthotopic Liver Transplant Anastomotic Bile Leak Causing Bilothorax, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
