Monday Poster Session
Category: Liver
P3869 - Confronting the Complexity of PML: Difficult Management Decisions
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Ahmer Khan, MD
Einstein Healthcare Network
Philadelphia, PA
Presenting Author(s)
Ahmer Khan, MD1, Kinga Grzybowski, MD1, Sushma Paramashivaiah, MD1, Aheed Javaid, MD2, Saman Zafar, MD1, Maria Lagarde, MD1, Richard Kalman, MD1
1Einstein Healthcare Network, Philadelphia, PA; 2Jefferson Abington Hospital, Philadelphia, PA
Introduction: Progressive multifocal leukoencephalopathy (PML) is caused by reactivation of JC virus (JCV). Initial infection with JCV occurs in childhood and antibodies can be found in most adults. JCV remains latent in kidneys and lymphoid organs, but in the context of profound cellular immunosuppression, JCV can reactivate. We present a therapeutic dilemma in a patient post liver transplantation who presented with concerns for PML.
Case Description/
Methods: 56-year-old male with a past medical history of HCV cirrhosis post liver transplantation in early 2024 and multiple episodes of biopsy proven T-cell mediated rejection presented with a chief complaint of bilateral vision loss and intermittent confusion that were progressive over three weeks.
Current medications included mycophenolate and prednisone. Previously on tacrolimus, this was held due to development of PRESS. Physical examination and laboratory studies including liver function testing were unremarkable. An MRI of the brain demonstrated an increased burden of white matter signal abnormalities in multiple regions of the brain that were suspicious for PML. Other leading differentials included CNS immune reconstitution syndrome, atypical PRESS or posttransplant lymphoproliferative disorder. He underwent a lumbar puncture with CSF analysis as well as a brain biopsy. Unfortunately, his CSF PCR demonstrated JC virus, and a brain biopsy was consistent with PML. When we attempted to minimize his immunosuppression, his aminotransferases rose significantly, reflecting acute rejection which was reflected on a subsequent liver biopsy.
Discussion: PCR is the preferred approach to the diagnosis of PML. Brain biopsy remains the gold standard in patients who are difficult to diagnose. In patients without evidence of HIV infection who develop PML, the mainstay of therapy is discontinuation or reduction of any immunosuppressants when feasible. Unfortunately, when we attempted to reduce the doses of his immunosuppressants, he developed severe acute rejection with his ALT and AST rising to 2550 IU/L and 1600 IU/L respectively.
We were unable to reduce his immunosuppressants to suitable levels to treat his biopsy proven acute rejection and concurrently prevent progression of PML. After conversations with the patient's family, the decision was made to send him home on hospice without any of his immunosuppressive medications. This case highlights the difficult and rare balancing act that we encounter with HIV negative patients on immunosuppression who develop PML.
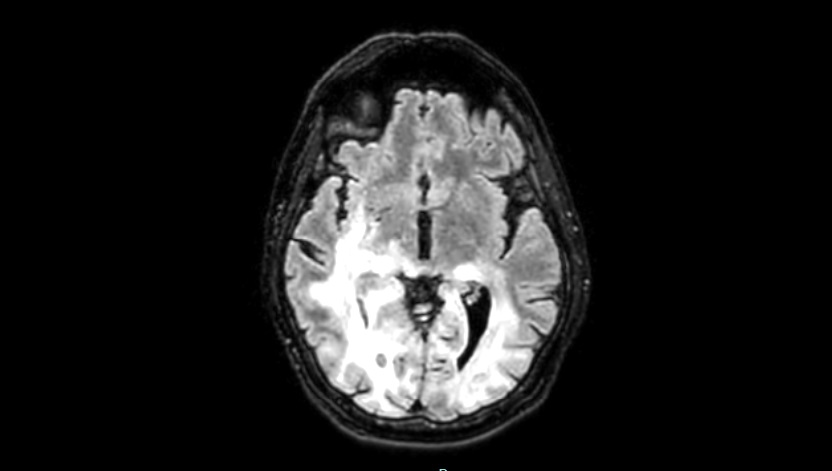
Figure: Diffuse white matter changes in the bilateral cerebral cortices on horizontal plane suggestive of PML.
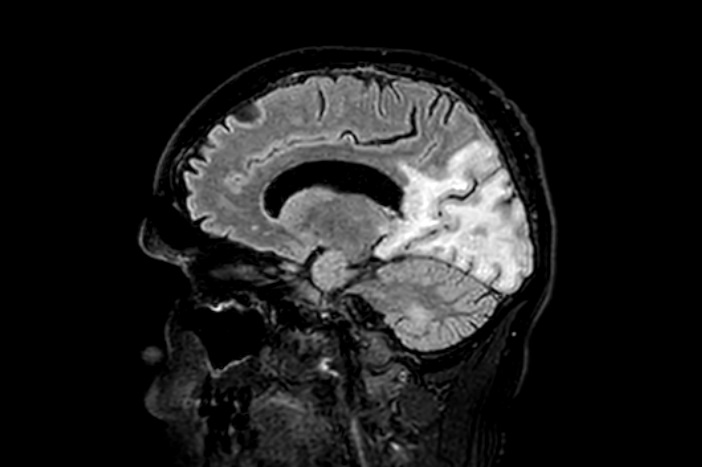
Figure: Diffuse white matter changes in the bilateral cerebral cortices on sagittal view suggestive of PML.
Disclosures:
Ahmer Khan indicated no relevant financial relationships.
Kinga Grzybowski indicated no relevant financial relationships.
Sushma Paramashivaiah indicated no relevant financial relationships.
Aheed Javaid indicated no relevant financial relationships.
Saman Zafar indicated no relevant financial relationships.
Maria Lagarde indicated no relevant financial relationships.
Richard Kalman indicated no relevant financial relationships.
Ahmer Khan, MD1, Kinga Grzybowski, MD1, Sushma Paramashivaiah, MD1, Aheed Javaid, MD2, Saman Zafar, MD1, Maria Lagarde, MD1, Richard Kalman, MD1. P3869 - Confronting the Complexity of PML: Difficult Management Decisions, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Einstein Healthcare Network, Philadelphia, PA; 2Jefferson Abington Hospital, Philadelphia, PA
Introduction: Progressive multifocal leukoencephalopathy (PML) is caused by reactivation of JC virus (JCV). Initial infection with JCV occurs in childhood and antibodies can be found in most adults. JCV remains latent in kidneys and lymphoid organs, but in the context of profound cellular immunosuppression, JCV can reactivate. We present a therapeutic dilemma in a patient post liver transplantation who presented with concerns for PML.
Case Description/
Methods: 56-year-old male with a past medical history of HCV cirrhosis post liver transplantation in early 2024 and multiple episodes of biopsy proven T-cell mediated rejection presented with a chief complaint of bilateral vision loss and intermittent confusion that were progressive over three weeks.
Current medications included mycophenolate and prednisone. Previously on tacrolimus, this was held due to development of PRESS. Physical examination and laboratory studies including liver function testing were unremarkable. An MRI of the brain demonstrated an increased burden of white matter signal abnormalities in multiple regions of the brain that were suspicious for PML. Other leading differentials included CNS immune reconstitution syndrome, atypical PRESS or posttransplant lymphoproliferative disorder. He underwent a lumbar puncture with CSF analysis as well as a brain biopsy. Unfortunately, his CSF PCR demonstrated JC virus, and a brain biopsy was consistent with PML. When we attempted to minimize his immunosuppression, his aminotransferases rose significantly, reflecting acute rejection which was reflected on a subsequent liver biopsy.
Discussion: PCR is the preferred approach to the diagnosis of PML. Brain biopsy remains the gold standard in patients who are difficult to diagnose. In patients without evidence of HIV infection who develop PML, the mainstay of therapy is discontinuation or reduction of any immunosuppressants when feasible. Unfortunately, when we attempted to reduce the doses of his immunosuppressants, he developed severe acute rejection with his ALT and AST rising to 2550 IU/L and 1600 IU/L respectively.
We were unable to reduce his immunosuppressants to suitable levels to treat his biopsy proven acute rejection and concurrently prevent progression of PML. After conversations with the patient's family, the decision was made to send him home on hospice without any of his immunosuppressive medications. This case highlights the difficult and rare balancing act that we encounter with HIV negative patients on immunosuppression who develop PML.
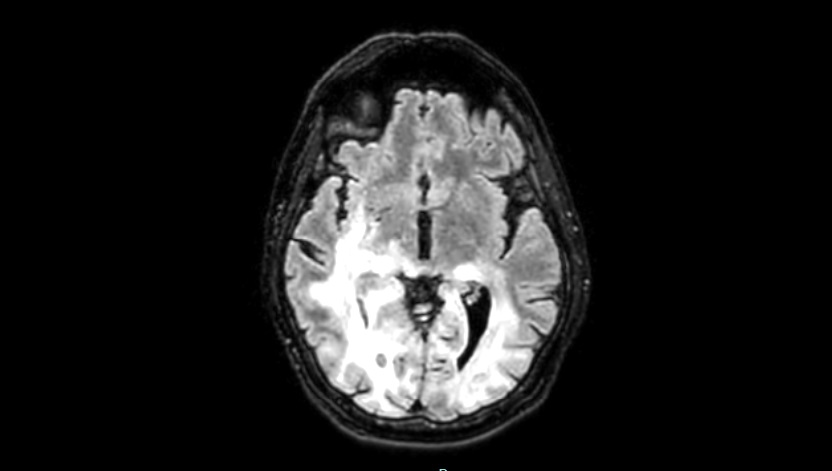
Figure: Diffuse white matter changes in the bilateral cerebral cortices on horizontal plane suggestive of PML.
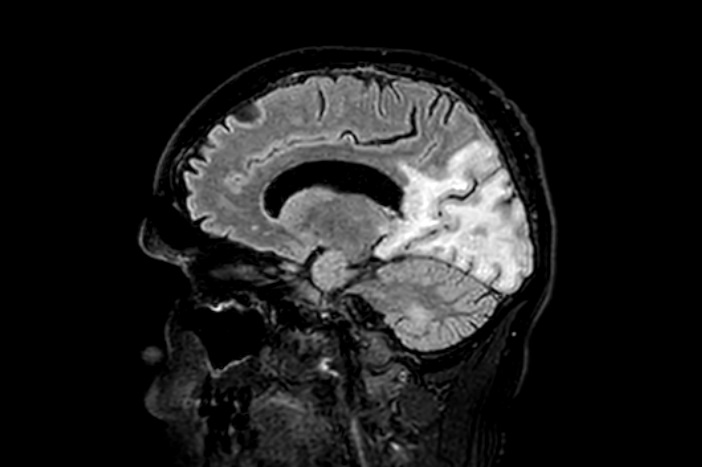
Figure: Diffuse white matter changes in the bilateral cerebral cortices on sagittal view suggestive of PML.
Disclosures:
Ahmer Khan indicated no relevant financial relationships.
Kinga Grzybowski indicated no relevant financial relationships.
Sushma Paramashivaiah indicated no relevant financial relationships.
Aheed Javaid indicated no relevant financial relationships.
Saman Zafar indicated no relevant financial relationships.
Maria Lagarde indicated no relevant financial relationships.
Richard Kalman indicated no relevant financial relationships.
Ahmer Khan, MD1, Kinga Grzybowski, MD1, Sushma Paramashivaiah, MD1, Aheed Javaid, MD2, Saman Zafar, MD1, Maria Lagarde, MD1, Richard Kalman, MD1. P3869 - Confronting the Complexity of PML: Difficult Management Decisions, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

