Monday Poster Session
Category: Liver
P3862 - The Clot Thickens: An Uncommon Cause of Portal Vein Thrombus
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ashley Dotson, MD (she/her/hers)
University of Washington
Seattle, WA
Presenting Author(s)
Ashley Dotson, MD1, Maya Biermann, MD1, Jabi Shriki, MD2, Ryan Kwok, MD3
1University of Washington, Seattle, WA; 2VA Puget Sound Health Care System, Seattle, WA; 3University of Washington School of Medicine and VA Puget Sound Health Care System, Seattle, WA
Introduction: Eltrombopag is thrombopoietin receptor agonist commonly used in immune thrombocytopenia (ITP) and thrombocytopenia secondary to chronic liver disease (CLD). We present a case of a patient with ITP and primary biliary cholangitis (PBC) associated cirrhosis complicated by hepatocellular carcinoma (HCC) treated with Y90 who was found to have symptomatic portal venous thrombus (PVT) attributed to high dose eltrombopag.
Case Description/
Methods: A 70-year-old male with a history of chronic ITP treated with eltrombopag and PBC-associated cirrhosis, complicated by HCC and treated with Y90, presented with a one-week history of right upper quadrant abdominal pain and generalized malaise. Admission CT demonstrated an occlusive PVT not seen on imaging performed 3 weeks earlier. Multiphasic liver CT revealed thrombus extension from the SMV and splenic vein confluence with complete occlusion of the right branches and near occlusion of the left branch of the portal vein (Figure 1). Radiologic appearance of the clot favored a non-malignant thrombus given the lack of discernible enhancement, vessel expansion, nor viable tumor in proximity to the clot. Chart review revealed prescription of an increased dose of eltrombopag shortly prior to presentation. This resulted in a rise in platelet count from a baseline of 6,000 – 7,000 to 222,000/mm3. After confirmation of non-malignant thrombus, eltrombopag was dose-reduced and anticoagulation was initiated. In accordance with current clinical recommendations,1 cross-sectional surveillance imaging was planned every 3 months to confirm thrombus resolution.
Discussion: PVT is an uncommon but potentially fatal complication of chronic liver disease. Despite their efficacy in the treatment of thrombocytopenia our case illustrates the risks associated with thrombopoietin receptor agonists. Eltrombopag has recently been evaluated for the treatment of portal hypertension associated thrombocytopenia in patients with CLD. Our case underscores the importance of closely monitoring platelet counts in this population when using this medication in patients with cirrhosis. Specifically, vigilance for thrombotic complications is warranted when platelet counts exceed 200,000/mm3. Furthermore, our case highlights the need for further study into the safety of eltrombopag in patients with ITP and CLD-related portal hypertension.
References
1Davis JPE et al. AGA update on portal vein thrombosis in cirrhosis. Gastroenterology. 2025;p. 396–404.
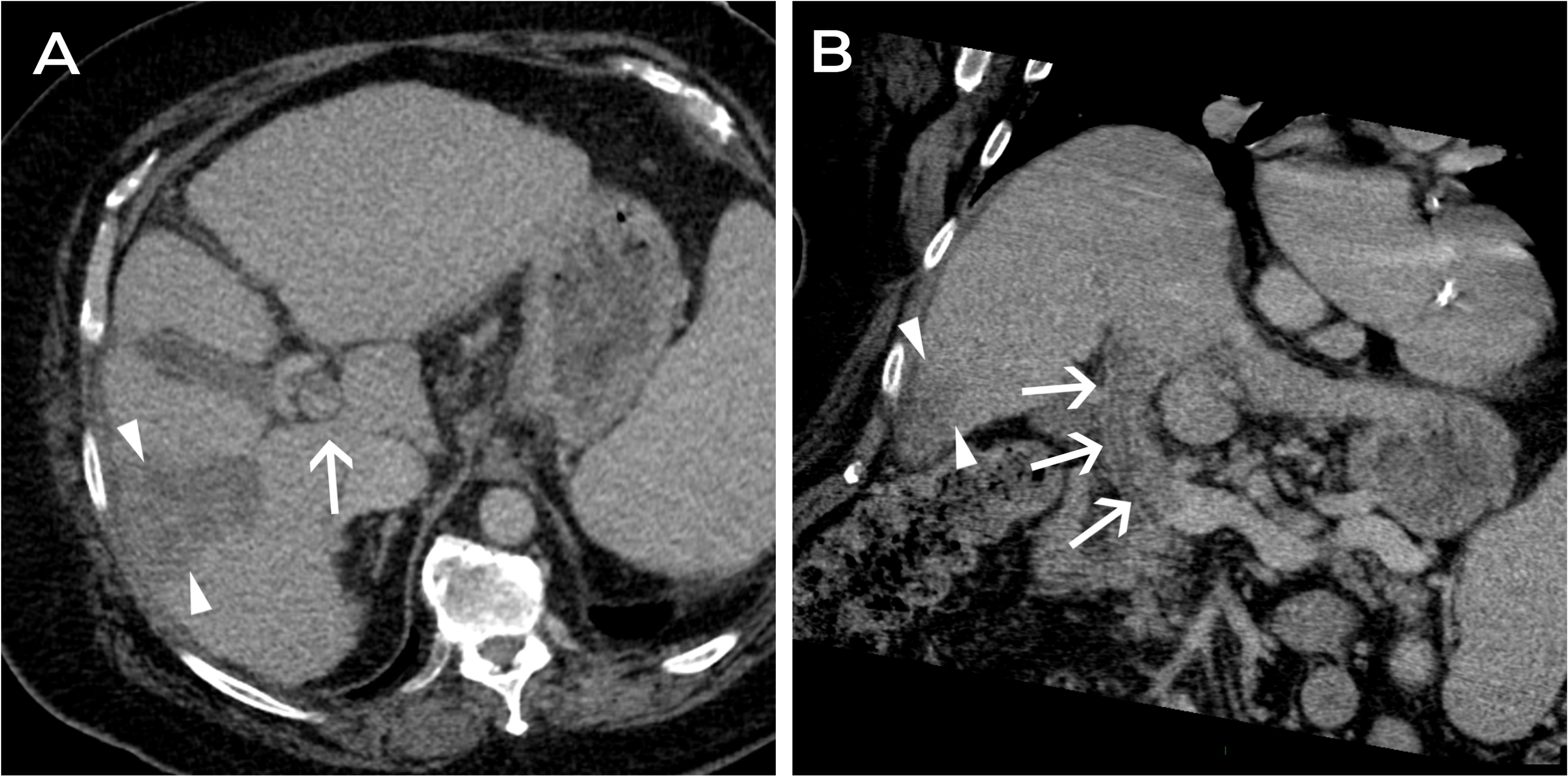
Figure: Initial multi-phase liver CT scan images (A-B) are shown in the transverse plane (A) and coronal oblique plane through the main portal vein (MPV). Images demonstrate the thrombus, seen as non-enhancement in the MPV (white arrows) as well as a persistent, wedge-shaped area of low attenuation (white arrowheads), corresponding to the area of post-treatment change in the periphery of the right posterior lobe of the liver.
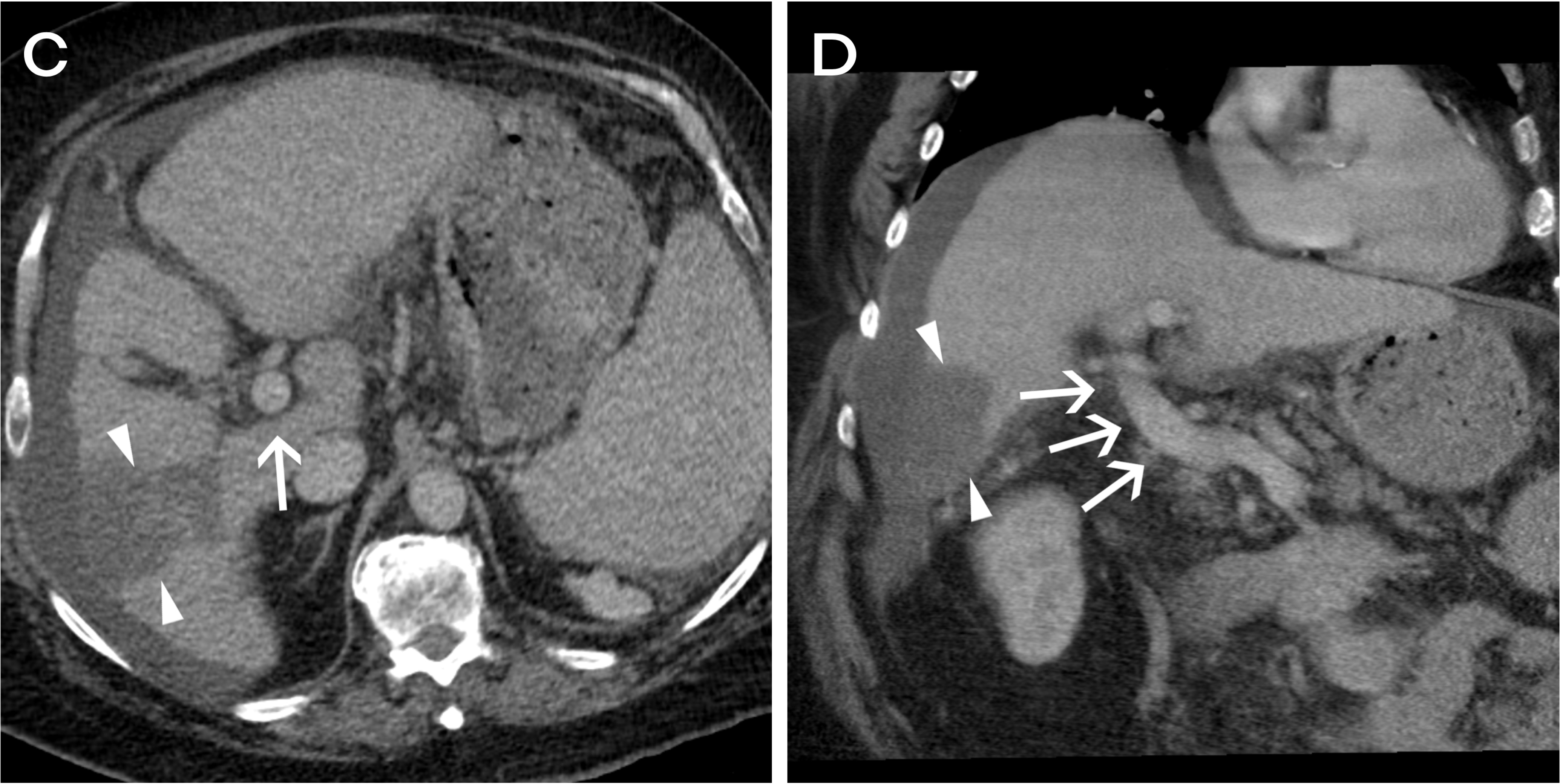
Figure: Three-month follow-up CT scan images (C-D) reveal subsequent resolution of the thrombus, with restoration of normal enhancement.
Disclosures:
Ashley Dotson indicated no relevant financial relationships.
Maya Biermann indicated no relevant financial relationships.
Jabi Shriki indicated no relevant financial relationships.
Ryan Kwok indicated no relevant financial relationships.
Ashley Dotson, MD1, Maya Biermann, MD1, Jabi Shriki, MD2, Ryan Kwok, MD3. P3862 - The Clot Thickens: An Uncommon Cause of Portal Vein Thrombus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Washington, Seattle, WA; 2VA Puget Sound Health Care System, Seattle, WA; 3University of Washington School of Medicine and VA Puget Sound Health Care System, Seattle, WA
Introduction: Eltrombopag is thrombopoietin receptor agonist commonly used in immune thrombocytopenia (ITP) and thrombocytopenia secondary to chronic liver disease (CLD). We present a case of a patient with ITP and primary biliary cholangitis (PBC) associated cirrhosis complicated by hepatocellular carcinoma (HCC) treated with Y90 who was found to have symptomatic portal venous thrombus (PVT) attributed to high dose eltrombopag.
Case Description/
Methods: A 70-year-old male with a history of chronic ITP treated with eltrombopag and PBC-associated cirrhosis, complicated by HCC and treated with Y90, presented with a one-week history of right upper quadrant abdominal pain and generalized malaise. Admission CT demonstrated an occlusive PVT not seen on imaging performed 3 weeks earlier. Multiphasic liver CT revealed thrombus extension from the SMV and splenic vein confluence with complete occlusion of the right branches and near occlusion of the left branch of the portal vein (Figure 1). Radiologic appearance of the clot favored a non-malignant thrombus given the lack of discernible enhancement, vessel expansion, nor viable tumor in proximity to the clot. Chart review revealed prescription of an increased dose of eltrombopag shortly prior to presentation. This resulted in a rise in platelet count from a baseline of 6,000 – 7,000 to 222,000/mm3. After confirmation of non-malignant thrombus, eltrombopag was dose-reduced and anticoagulation was initiated. In accordance with current clinical recommendations,1 cross-sectional surveillance imaging was planned every 3 months to confirm thrombus resolution.
Discussion: PVT is an uncommon but potentially fatal complication of chronic liver disease. Despite their efficacy in the treatment of thrombocytopenia our case illustrates the risks associated with thrombopoietin receptor agonists. Eltrombopag has recently been evaluated for the treatment of portal hypertension associated thrombocytopenia in patients with CLD. Our case underscores the importance of closely monitoring platelet counts in this population when using this medication in patients with cirrhosis. Specifically, vigilance for thrombotic complications is warranted when platelet counts exceed 200,000/mm3. Furthermore, our case highlights the need for further study into the safety of eltrombopag in patients with ITP and CLD-related portal hypertension.
References
1Davis JPE et al. AGA update on portal vein thrombosis in cirrhosis. Gastroenterology. 2025;p. 396–404.
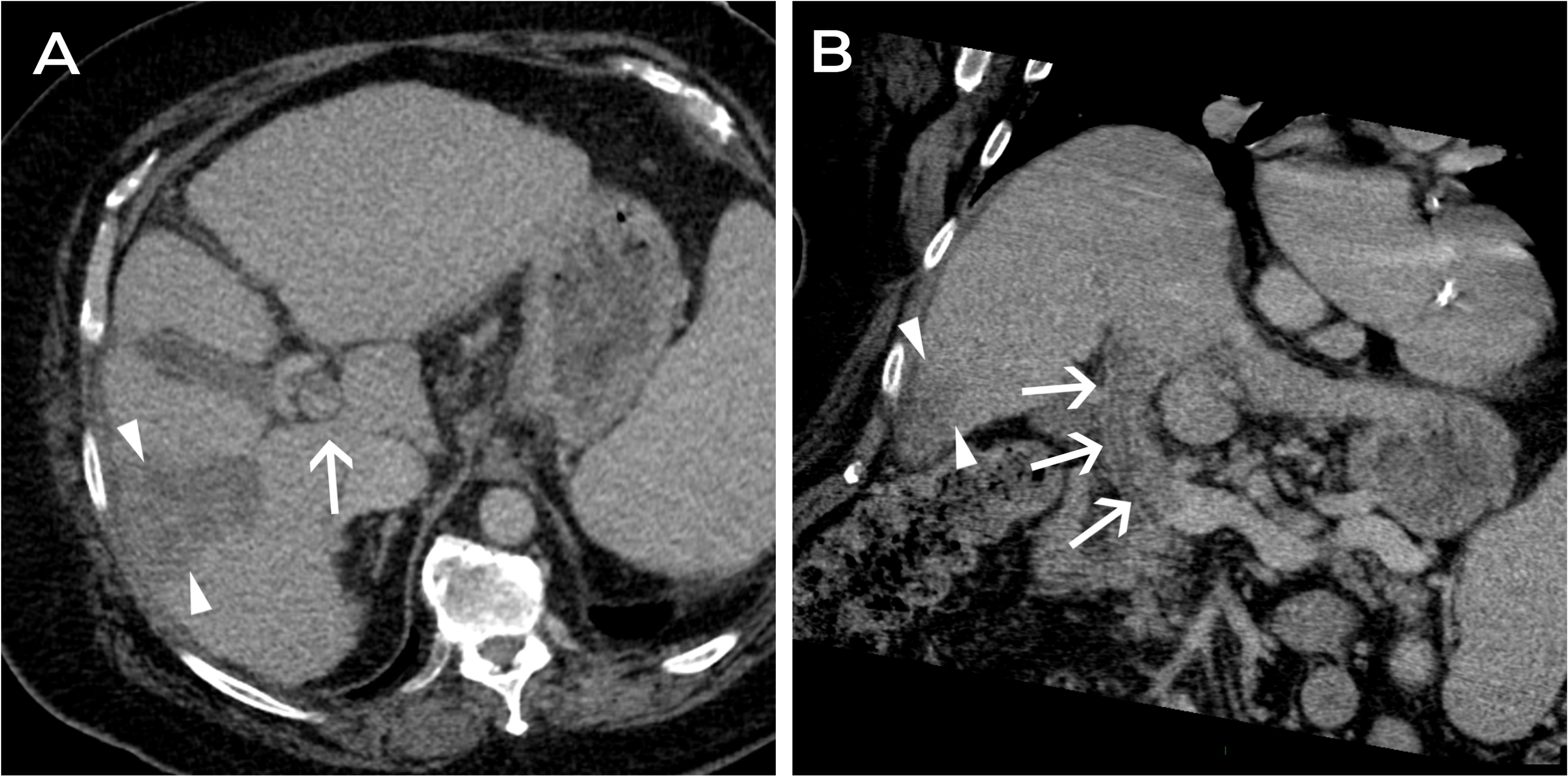
Figure: Initial multi-phase liver CT scan images (A-B) are shown in the transverse plane (A) and coronal oblique plane through the main portal vein (MPV). Images demonstrate the thrombus, seen as non-enhancement in the MPV (white arrows) as well as a persistent, wedge-shaped area of low attenuation (white arrowheads), corresponding to the area of post-treatment change in the periphery of the right posterior lobe of the liver.
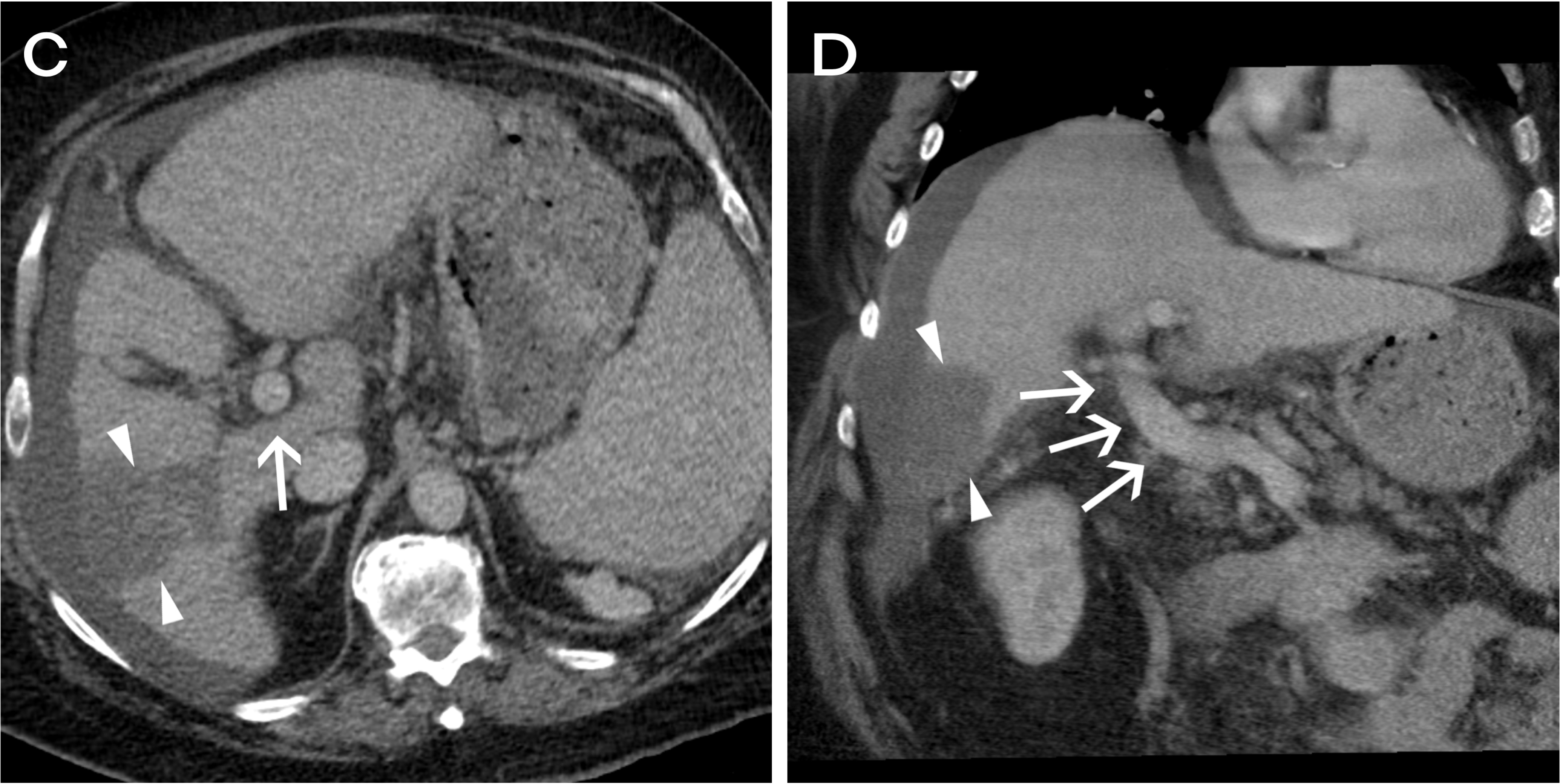
Figure: Three-month follow-up CT scan images (C-D) reveal subsequent resolution of the thrombus, with restoration of normal enhancement.
Disclosures:
Ashley Dotson indicated no relevant financial relationships.
Maya Biermann indicated no relevant financial relationships.
Jabi Shriki indicated no relevant financial relationships.
Ryan Kwok indicated no relevant financial relationships.
Ashley Dotson, MD1, Maya Biermann, MD1, Jabi Shriki, MD2, Ryan Kwok, MD3. P3862 - The Clot Thickens: An Uncommon Cause of Portal Vein Thrombus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

