Monday Poster Session
Category: Liver
P3961 - A Presumed Primary Hepatic Neuroendocrine Tumor Presenting With Disseminated Intravascular Coagulation
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Neel Shah, MD (he/him/his)
Baylor Scott & White Medical Center
Round Rock, TX
Presenting Author(s)
Neel Shah, MD1, Lindsay Mathys, 2, Tyler Tepfenhart, DO1, Dana Luu, 2
1Baylor Scott & White Medical Center, Round Rock, TX; 2Texas A&M School of Medicine, Round Rock, TX
Introduction: Primary hepatic neuroendocrine tumors (PHNETs) are exceedingly rare, accounting for less than 0.5% of primary liver malignancies. Unlike more common metastatic hepatic NETs, PHNETs originate in the liver and present with nonspecific symptoms, often leading to delayed or incorrect diagnosis. Histopathologic confirmation and exclusion of an extrahepatic primary site are required for definitive diagnosis, though this may be limited in critically ill patients.
Case Description/
Methods: A 74-year-old male with cirrhosis due to nonalcoholic steatohepatitis presented with three weeks of anorexia, nausea, and abdominal pain. Laboratory evaluation revealed elevated cholestatic liver enzymes, hyperbilirubinemia, and new-onset thrombocytopenia. Initial CT and ultrasound were inconclusive. MRI/MRCP revealed multiple hepatic nodular densities (Figure 1), and a hepatobiliary iminodiacetic acid scan demonstrated diffuse hepatic dysfunction. Infectious, autoimmune, and toxicologic workups were negative.
A transjugular liver biopsy performed on hospital day five revealed high-grade neuroendocrine carcinoma with small cell morphology involving portal tracts and sinusoidal spaces. Immunohistochemistry was positive for synaptophysin, chromogranin A, and keratin and negative for p40, CD45, and Sox10. A Ki-67 index and mitotic rate were not obtained. The background liver showed nodular architecture and focal ductular proliferation. No extrahepatic primary site was identified; however, further staging with PET or endoscopy was not performed due to clinical deterioration.
The patient’s condition worsened with progressive thrombocytopenia, elevated LDH, and D-dimer, consistent with disseminated intravascular coagulation (DIC). No precipitating infection, medication, or hematologic disorder was identified. Due to decompensated liver function, chemotherapy was deferred. He transitioned to hospice care and expired on hospital day sixteen.
Discussion: This case highlights a presumed PHNET complicated by DIC in the absence of systemic therapy or co-infection. While NET-associated DIC has been described in pancreatic primaries, this case expands the context to hepatic origin. Due to incomplete staging, metastatic disease could not be excluded. Clinicians must maintain a high level of suspicion for atypical hepatic lesions in cirrhotic patients and watch for early signs of coagulopathy in those with high-grade neuroendocrine tumors.
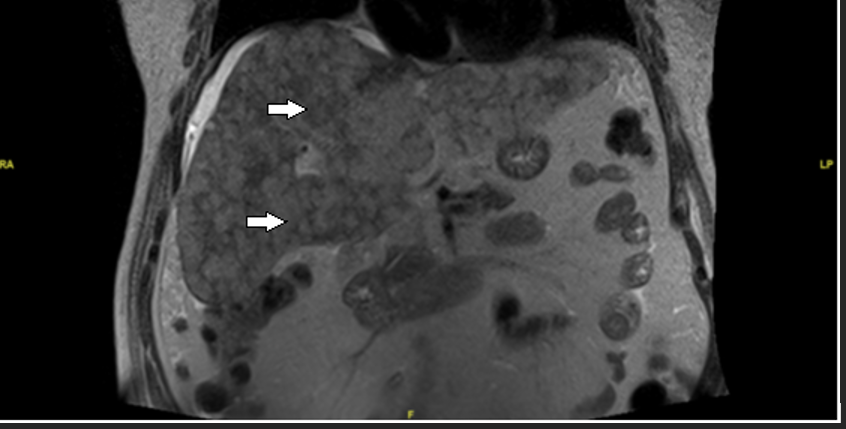
Figure: Figure 1. Coronal contrast-enhanced MRI/MRCP of abdomen and pelvis - shows diffusely abnormal appearance of the liver, arrows indicate multiple nodular densities
Disclosures:
Neel Shah indicated no relevant financial relationships.
Lindsay Mathys indicated no relevant financial relationships.
Tyler Tepfenhart indicated no relevant financial relationships.
Dana Luu indicated no relevant financial relationships.
Neel Shah, MD1, Lindsay Mathys, 2, Tyler Tepfenhart, DO1, Dana Luu, 2. P3961 - A Presumed Primary Hepatic Neuroendocrine Tumor Presenting With Disseminated Intravascular Coagulation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Baylor Scott & White Medical Center, Round Rock, TX; 2Texas A&M School of Medicine, Round Rock, TX
Introduction: Primary hepatic neuroendocrine tumors (PHNETs) are exceedingly rare, accounting for less than 0.5% of primary liver malignancies. Unlike more common metastatic hepatic NETs, PHNETs originate in the liver and present with nonspecific symptoms, often leading to delayed or incorrect diagnosis. Histopathologic confirmation and exclusion of an extrahepatic primary site are required for definitive diagnosis, though this may be limited in critically ill patients.
Case Description/
Methods: A 74-year-old male with cirrhosis due to nonalcoholic steatohepatitis presented with three weeks of anorexia, nausea, and abdominal pain. Laboratory evaluation revealed elevated cholestatic liver enzymes, hyperbilirubinemia, and new-onset thrombocytopenia. Initial CT and ultrasound were inconclusive. MRI/MRCP revealed multiple hepatic nodular densities (Figure 1), and a hepatobiliary iminodiacetic acid scan demonstrated diffuse hepatic dysfunction. Infectious, autoimmune, and toxicologic workups were negative.
A transjugular liver biopsy performed on hospital day five revealed high-grade neuroendocrine carcinoma with small cell morphology involving portal tracts and sinusoidal spaces. Immunohistochemistry was positive for synaptophysin, chromogranin A, and keratin and negative for p40, CD45, and Sox10. A Ki-67 index and mitotic rate were not obtained. The background liver showed nodular architecture and focal ductular proliferation. No extrahepatic primary site was identified; however, further staging with PET or endoscopy was not performed due to clinical deterioration.
The patient’s condition worsened with progressive thrombocytopenia, elevated LDH, and D-dimer, consistent with disseminated intravascular coagulation (DIC). No precipitating infection, medication, or hematologic disorder was identified. Due to decompensated liver function, chemotherapy was deferred. He transitioned to hospice care and expired on hospital day sixteen.
Discussion: This case highlights a presumed PHNET complicated by DIC in the absence of systemic therapy or co-infection. While NET-associated DIC has been described in pancreatic primaries, this case expands the context to hepatic origin. Due to incomplete staging, metastatic disease could not be excluded. Clinicians must maintain a high level of suspicion for atypical hepatic lesions in cirrhotic patients and watch for early signs of coagulopathy in those with high-grade neuroendocrine tumors.
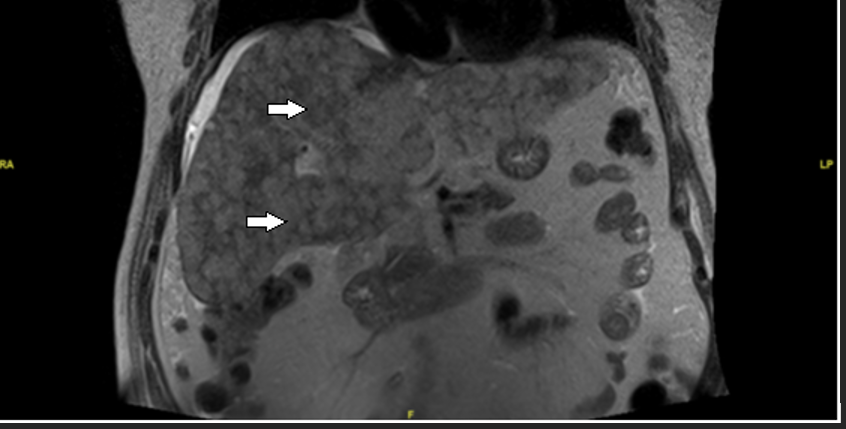
Figure: Figure 1. Coronal contrast-enhanced MRI/MRCP of abdomen and pelvis - shows diffusely abnormal appearance of the liver, arrows indicate multiple nodular densities
Disclosures:
Neel Shah indicated no relevant financial relationships.
Lindsay Mathys indicated no relevant financial relationships.
Tyler Tepfenhart indicated no relevant financial relationships.
Dana Luu indicated no relevant financial relationships.
Neel Shah, MD1, Lindsay Mathys, 2, Tyler Tepfenhart, DO1, Dana Luu, 2. P3961 - A Presumed Primary Hepatic Neuroendocrine Tumor Presenting With Disseminated Intravascular Coagulation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
