Monday Poster Session
Category: Liver
P3960 - Recurrent Budd-Chiari Syndrome From Hepatic Outflow Obstruction in a Patient With Prior Hepatic Vein Stent
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Neel Shah, MD (he/him/his)
Baylor Scott & White Medical Center
Round Rock, TX
Presenting Author(s)
Neel Shah, MD1, Kalee Moore, DO1, Pavia Muringathuparambil, MD2, Chiranjeevi Gadiparthi, MD1, Rajiv Srinivasa, MD1
1Baylor Scott & White Medical Center, Round Rock, TX; 2Baylor Scott & White Medical Center - Round Rock, Round Rock, TX
Introduction: Budd-Chiari Syndrome (BCS) is a rare disorder defined as obstruction of hepatic venous outflow, most commonly due to thrombosis, hypercoagulable states, or primary venous pathology. Endovascular stenting might provide symptomatic relief in select cases, but long-term surveillance is often limited. Delayed complications, such as in-stent stenosis, may go unnoticed. We present a case of recurrent BCS nearly two decades after stent placement, in which in-stenosis was identified as a reversible etiology of hepatic congestion and thrombosis.
Case Description/
Methods: A 39-year-old female with a history of unprovoked inferior vena cava (IVC) thrombosis treated with warfarin at age 18 and hepatic vein stent placement at age 21 while living in Iran, presented with progressive abdominal bloating and periumbilical discomfort. She had been stable on anticoagulation for nearly two decades before warfarin was discontinued the prior year. Outpatient CT scan revealed nonocclusive thrombi involving the portal vein, superior mesenteric vein, IVC, and bilateral iliac vein with splenomegaly and ascites, prompting hospitalization. Liver chemistries were normal. Given her vascular history and signs of portal hypertension, transjugular liver biopsy was planned to evaluate for chronic liver disease.
Hepatic venography revealed a patent IVC with mild intrahepatic narrowing. Cannulation of her prior right hepatic vein stent showed focal, high-grade stenosis at its distal end (Figure 1). Extensive intrahepatic collateralization was noted. Manometry showed an elevated hepatic vein—right atrial gradient of 28 mmHg. Balloon angioplasty of the in-stent stenosis reduced pressure from 30 mmHg to 14 mmHg, normalizing the gradient to 3 mmHg. Post-intervention venography showed improved stent flow and a reduction in the size of collaterals. Liver biopsy deferred due to improvement.
Hypercoagulable workup was negative. Although her mother had a history of protein C deficiency, the patient had normal levels. The thrombi were attributed to mechanical hepatic outflow obstruction. Long-term anticoagulation was recommended.
Discussion: This case illustrates a rare case of hepatic vein in-stent stenosis as a delayed but reversible cause of BCS. In patients with hepatic vascular interventions, new ascites or splanchnic thrombosis should prompt evaluation for mechanical outflow obstruction. Hepatic venography was both diagnostic and therapeutic, leading to restoration of hepatic venous flow and preventing long-term complications.
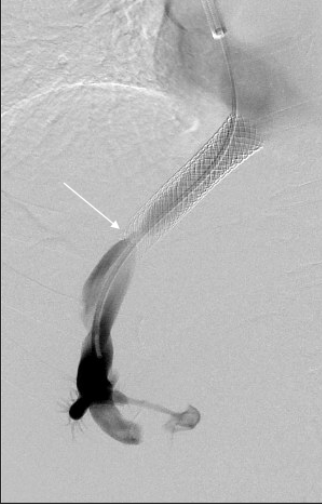
Figure: Figure 1: Pre-intervention venogram showing focal high-grade stenosis at the distal aspect of the right hepatic vein stent (white arrow)
Disclosures:
Neel Shah indicated no relevant financial relationships.
Kalee Moore indicated no relevant financial relationships.
Pavia Muringathuparambil indicated no relevant financial relationships.
Chiranjeevi Gadiparthi indicated no relevant financial relationships.
Rajiv Srinivasa indicated no relevant financial relationships.
Neel Shah, MD1, Kalee Moore, DO1, Pavia Muringathuparambil, MD2, Chiranjeevi Gadiparthi, MD1, Rajiv Srinivasa, MD1. P3960 - Recurrent Budd-Chiari Syndrome From Hepatic Outflow Obstruction in a Patient With Prior Hepatic Vein Stent, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Baylor Scott & White Medical Center, Round Rock, TX; 2Baylor Scott & White Medical Center - Round Rock, Round Rock, TX
Introduction: Budd-Chiari Syndrome (BCS) is a rare disorder defined as obstruction of hepatic venous outflow, most commonly due to thrombosis, hypercoagulable states, or primary venous pathology. Endovascular stenting might provide symptomatic relief in select cases, but long-term surveillance is often limited. Delayed complications, such as in-stent stenosis, may go unnoticed. We present a case of recurrent BCS nearly two decades after stent placement, in which in-stenosis was identified as a reversible etiology of hepatic congestion and thrombosis.
Case Description/
Methods: A 39-year-old female with a history of unprovoked inferior vena cava (IVC) thrombosis treated with warfarin at age 18 and hepatic vein stent placement at age 21 while living in Iran, presented with progressive abdominal bloating and periumbilical discomfort. She had been stable on anticoagulation for nearly two decades before warfarin was discontinued the prior year. Outpatient CT scan revealed nonocclusive thrombi involving the portal vein, superior mesenteric vein, IVC, and bilateral iliac vein with splenomegaly and ascites, prompting hospitalization. Liver chemistries were normal. Given her vascular history and signs of portal hypertension, transjugular liver biopsy was planned to evaluate for chronic liver disease.
Hepatic venography revealed a patent IVC with mild intrahepatic narrowing. Cannulation of her prior right hepatic vein stent showed focal, high-grade stenosis at its distal end (Figure 1). Extensive intrahepatic collateralization was noted. Manometry showed an elevated hepatic vein—right atrial gradient of 28 mmHg. Balloon angioplasty of the in-stent stenosis reduced pressure from 30 mmHg to 14 mmHg, normalizing the gradient to 3 mmHg. Post-intervention venography showed improved stent flow and a reduction in the size of collaterals. Liver biopsy deferred due to improvement.
Hypercoagulable workup was negative. Although her mother had a history of protein C deficiency, the patient had normal levels. The thrombi were attributed to mechanical hepatic outflow obstruction. Long-term anticoagulation was recommended.
Discussion: This case illustrates a rare case of hepatic vein in-stent stenosis as a delayed but reversible cause of BCS. In patients with hepatic vascular interventions, new ascites or splanchnic thrombosis should prompt evaluation for mechanical outflow obstruction. Hepatic venography was both diagnostic and therapeutic, leading to restoration of hepatic venous flow and preventing long-term complications.
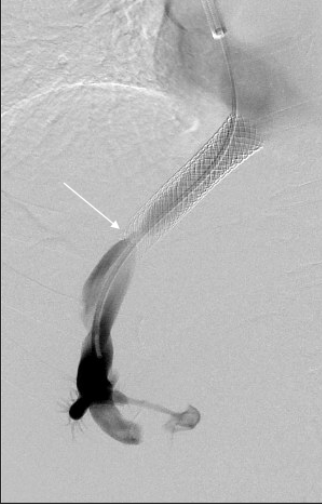
Figure: Figure 1: Pre-intervention venogram showing focal high-grade stenosis at the distal aspect of the right hepatic vein stent (white arrow)
Disclosures:
Neel Shah indicated no relevant financial relationships.
Kalee Moore indicated no relevant financial relationships.
Pavia Muringathuparambil indicated no relevant financial relationships.
Chiranjeevi Gadiparthi indicated no relevant financial relationships.
Rajiv Srinivasa indicated no relevant financial relationships.
Neel Shah, MD1, Kalee Moore, DO1, Pavia Muringathuparambil, MD2, Chiranjeevi Gadiparthi, MD1, Rajiv Srinivasa, MD1. P3960 - Recurrent Budd-Chiari Syndrome From Hepatic Outflow Obstruction in a Patient With Prior Hepatic Vein Stent, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

