Monday Poster Session
Category: Liver
P3956 - Liver Cirrhosis and Interstitial Lung Disease in Short Telomere Syndrome: A Case Highlighting the Importance of Early Detection and Transplant Candidacy Challenges
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

M Housam Nanah, MD
Cleveland Clinic
Cleveland, OH
Presenting Author(s)
M Housam Nanah, MD1, Tesfaye Yadete, MD2, Abdullah Hafeez, MD3, Jamile Wakim-Fleming, MD1
1Cleveland Clinic, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH; 3Landmark Medical Center, Woonsocket, RI
Introduction: Short telomere syndrome (STS) is a rare, inherited disorder caused by mutations in telomere maintenance genes, leading to progressive multiorgan dysfunction. Common features include pulmonary fibrosis, bone marrow failure, and cirrhosis. Due to its heterogeneity, diagnosis is often delayed. We present a case of a 57-year-old male with STS and interstitial lung disease, evaluated for combined lung-liver transplantation.
Case Description/
Methods: A 57-year-old male with ILD and cryptogenic cirrhosis complicated by Grade 3 esophageal varices (s/p banding 2/2023), ascites, hepatic encephalopathy, and hepatopulmonary syndrome presented with fever, abdominal distension, and melena. Labs: platelets 88,000, hemoglobin 6.7 g/dL, INR 1.7, total bilirubin 4.4 mg/dL. CT showed extensive fibrosis with subpleural reticular and ground-glass opacities, traction bronchiectasis, and architectural distortion, basilar and peripheral. Genetic testing confirmed STS with critically short telomeres (lymphocytes 1–10%, granulocytes < 1%). He was started on prednisone for suspected ILD flare and empiric antibiotics, and transferred for lung-liver transplant evaluation. During workup, he developed progressive respiratory failure and died from rapid deterioration. Autopsy showed bilateral lung diffuse interstitial fibrosis with repair, focal pneumonia and hemorrhage, right lower lung lobe subpleural scarring, and bilateral lungs focal petechial hemorrhages, liver diffuse fibrosis with surface nodularity, normocellular bone marrow with Megakaryocyte hypoplasia, and cardiomegaly with bilateral atrial enlargement and ventricular moderate interstitial fibrosis.
Discussion: STS is a rare, autosomal dominant disorder with highly variable clinical expression. Its presentation often overlaps with other more common diseases, leading to underdiagnosis or delayed recognition. Pulmonary disease is the most common manifestation and liver transplant is essential for survival.
This case illustrates the aggressive and multisystem progression of STS and the critical importance of early suspicion, diagnosis, and referral—especially for transplant eligibility. Genetic testing and telomere length analysis are essential for confirmation. Additionally, due to genetic anticipation, early family screening and counseling are warranted. The case underscores the need for standardized protocols for early recognition, transplant timing, and comprehensive multidisciplinary management.
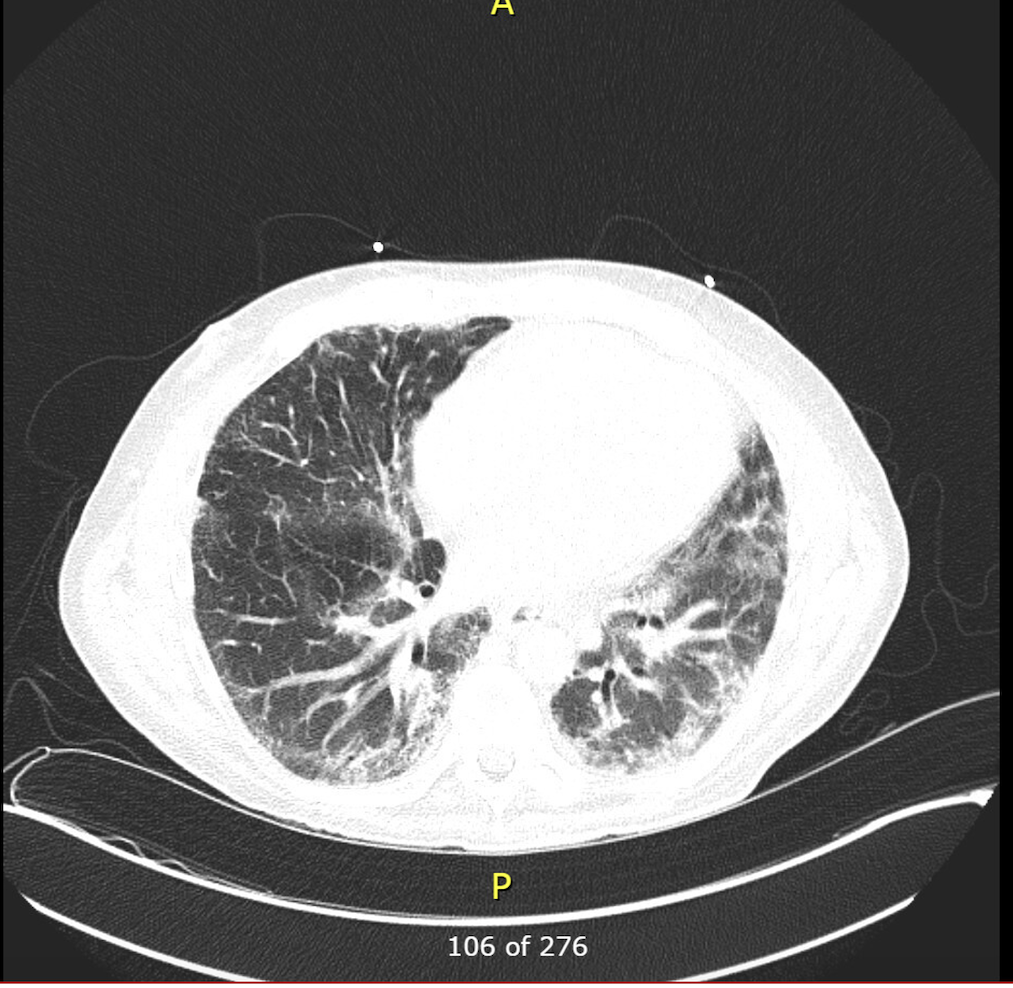
Figure: CT scan showing pulmonary involvement (extensive fibrotic changes with subpleural reticular and
groundglass opacities).
Disclosures:
M Housam Nanah indicated no relevant financial relationships.
Tesfaye Yadete indicated no relevant financial relationships.
Abdullah Hafeez indicated no relevant financial relationships.
Jamile Wakim-Fleming indicated no relevant financial relationships.
M Housam Nanah, MD1, Tesfaye Yadete, MD2, Abdullah Hafeez, MD3, Jamile Wakim-Fleming, MD1. P3956 - Liver Cirrhosis and Interstitial Lung Disease in Short Telomere Syndrome: A Case Highlighting the Importance of Early Detection and Transplant Candidacy Challenges, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cleveland Clinic, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH; 3Landmark Medical Center, Woonsocket, RI
Introduction: Short telomere syndrome (STS) is a rare, inherited disorder caused by mutations in telomere maintenance genes, leading to progressive multiorgan dysfunction. Common features include pulmonary fibrosis, bone marrow failure, and cirrhosis. Due to its heterogeneity, diagnosis is often delayed. We present a case of a 57-year-old male with STS and interstitial lung disease, evaluated for combined lung-liver transplantation.
Case Description/
Methods: A 57-year-old male with ILD and cryptogenic cirrhosis complicated by Grade 3 esophageal varices (s/p banding 2/2023), ascites, hepatic encephalopathy, and hepatopulmonary syndrome presented with fever, abdominal distension, and melena. Labs: platelets 88,000, hemoglobin 6.7 g/dL, INR 1.7, total bilirubin 4.4 mg/dL. CT showed extensive fibrosis with subpleural reticular and ground-glass opacities, traction bronchiectasis, and architectural distortion, basilar and peripheral. Genetic testing confirmed STS with critically short telomeres (lymphocytes 1–10%, granulocytes < 1%). He was started on prednisone for suspected ILD flare and empiric antibiotics, and transferred for lung-liver transplant evaluation. During workup, he developed progressive respiratory failure and died from rapid deterioration. Autopsy showed bilateral lung diffuse interstitial fibrosis with repair, focal pneumonia and hemorrhage, right lower lung lobe subpleural scarring, and bilateral lungs focal petechial hemorrhages, liver diffuse fibrosis with surface nodularity, normocellular bone marrow with Megakaryocyte hypoplasia, and cardiomegaly with bilateral atrial enlargement and ventricular moderate interstitial fibrosis.
Discussion: STS is a rare, autosomal dominant disorder with highly variable clinical expression. Its presentation often overlaps with other more common diseases, leading to underdiagnosis or delayed recognition. Pulmonary disease is the most common manifestation and liver transplant is essential for survival.
This case illustrates the aggressive and multisystem progression of STS and the critical importance of early suspicion, diagnosis, and referral—especially for transplant eligibility. Genetic testing and telomere length analysis are essential for confirmation. Additionally, due to genetic anticipation, early family screening and counseling are warranted. The case underscores the need for standardized protocols for early recognition, transplant timing, and comprehensive multidisciplinary management.
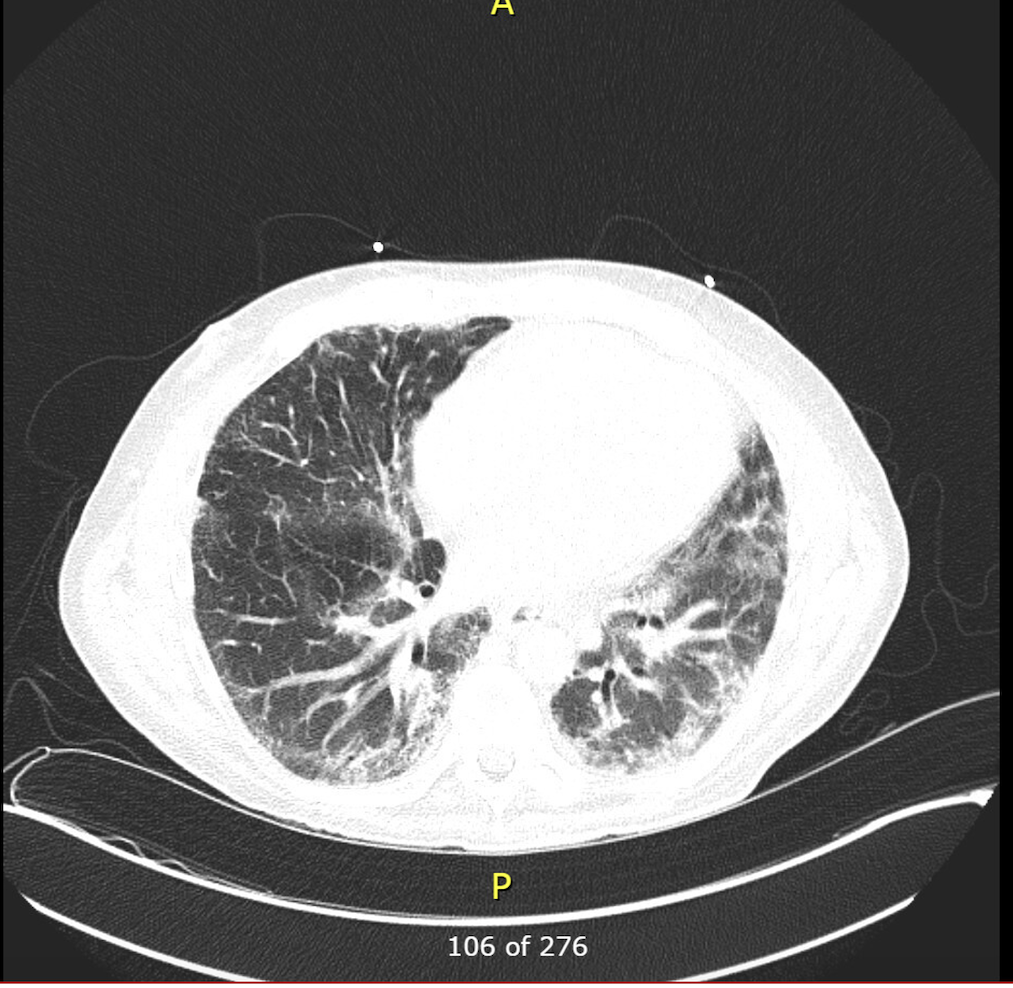
Figure: CT scan showing pulmonary involvement (extensive fibrotic changes with subpleural reticular and
groundglass opacities).
Disclosures:
M Housam Nanah indicated no relevant financial relationships.
Tesfaye Yadete indicated no relevant financial relationships.
Abdullah Hafeez indicated no relevant financial relationships.
Jamile Wakim-Fleming indicated no relevant financial relationships.
M Housam Nanah, MD1, Tesfaye Yadete, MD2, Abdullah Hafeez, MD3, Jamile Wakim-Fleming, MD1. P3956 - Liver Cirrhosis and Interstitial Lung Disease in Short Telomere Syndrome: A Case Highlighting the Importance of Early Detection and Transplant Candidacy Challenges, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
