Monday Poster Session
Category: Liver
P3949 - Post-Hepatectomy Portal Hypertensive Sequelae Treated With Splenic Embolization and Complicated by Formation of a Large Splenic Pseudocyst
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Christina Joya, DO
Valley Hospital Medical Center
Las Vegas, NV
Presenting Author(s)
Christina Joya, DO, Luis Muñoz, MD, Megan Hubbard, DO, Masuma Syed, MD, Scott Silver, DO, Vishvinder Sharma, MD
Valley Hospital Medical Center, Las Vegas, NV
Introduction: A Klatskin tumor is a rare malignancy occurring at the common hepatic duct bifurcation. About two-thirds of Klatskin tumors are resectable, often requiring bile duct resection and less commonly partial hepatectomy. Post-hepatectomy portal hypertension (PHPH) is a known complication with high morbidity and mortality. We present a case of a patient with PHPH who underwent splenic embolization, leading to the rare formation of a large symptomatic splenic pseudocyst.
Case Description/
Methods: 57-year-old male with history of a Klatskin tumor status post partial right hepatectomy presented with syncope, coffee ground emesis, and melena. Labs were significant for Hb 6.0, Hct 21.3, MCV 74.2, PLT 212, AST 39, ALT 37, alkaline phosphatase 226, total bilirubin 1.0, INR 1.2. CT imaging revealed chronic extrahepatic main portal vein occlusion with cavernous transformation, absent middle hepatic vein, gastrorenal shunt, gastric and esophageal varices, and splenomegaly. EGD confirmed gastric and esophageal varices with a large IGV1 gastric varix with high risk bleeding stigmata. Due to the complex anatomy, a transjugular intrahepatic portosystemic shunt (TIPS) procedure was deemed high risk. Coil-assisted or balloon-occluded retrograde transvenous obliteration (CRTO/BRTO) of the gastrorenal shunt was considered, but carried risk of worsening the patient’s esophageal varices. Ultimately, the patient underwent splenic artery embolization (50-60%) to reduce portal pressures and decrease re-bleeding risk. Two months later, the patient presented with left sided abdominal pain, vomiting, and a left pleural effusion. MRI showed an 18x21x23 cm splenic pseudocyst. A percutaneous drain was placed. Fluid cultures grew Enterococcus faecalis, treated with daptomycin.
Discussion: PHPH is linked to poorer long term survival and an increased post-hepatectomy liver failure. The development of PHPH can be predicted by the extent of the liver resection, with larger hepatectomies carrying higher risk. As seen in this case, understanding postsurgical anatomy and portosystemic changes is crucial when planning intervention. Splenic artery embolization is a minimally invasive approach to variceal bleeding, but it is not without risk. Post-embolization symptoms of nausea, vomiting, abdominal pain should be addressed promptly to reduce complications associated with pseudocysts - including superinfections of the cystic fluid. The challenges associated with PHPH and its management present a promising area for further research.
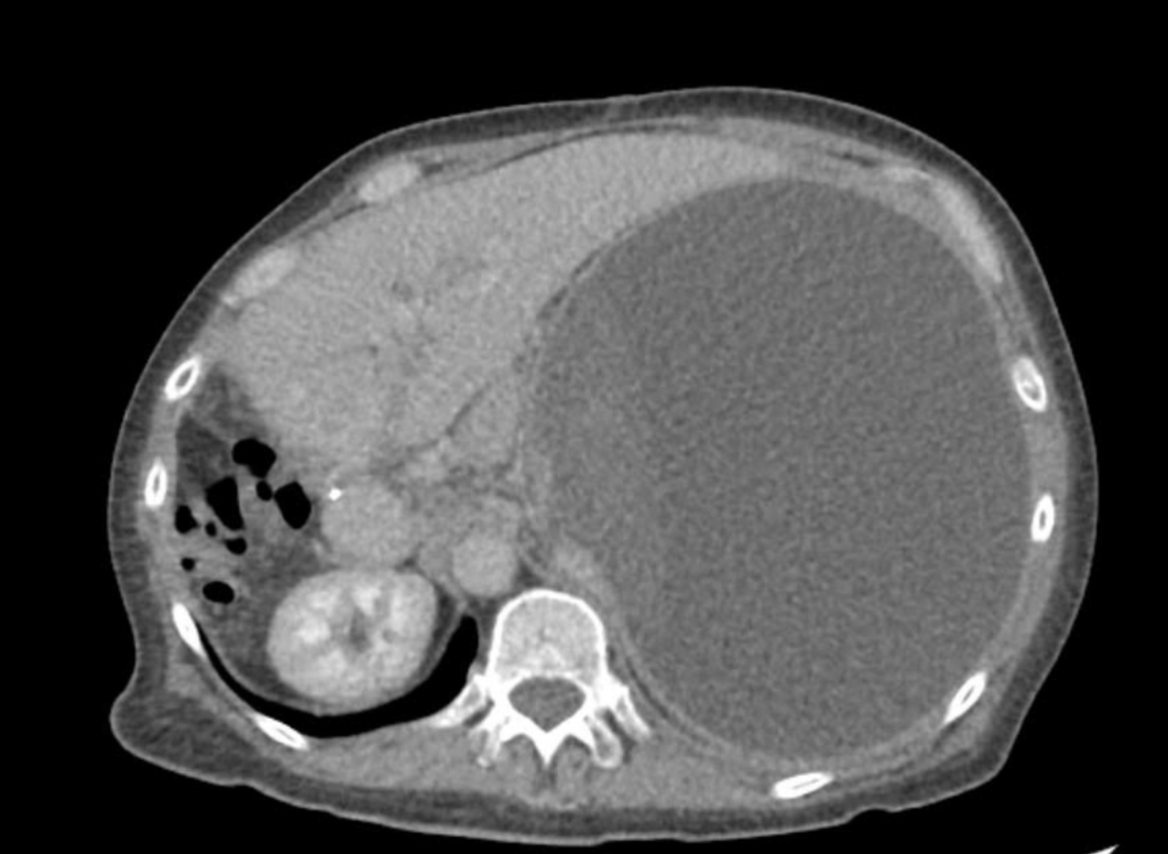
Figure: MRI of the abdomen showing an 18 x 21 x 23 cm splenic pseudocyst.
Disclosures:
Christina Joya indicated no relevant financial relationships.
Luis Muñoz indicated no relevant financial relationships.
Megan Hubbard indicated no relevant financial relationships.
Masuma Syed indicated no relevant financial relationships.
Scott Silver indicated no relevant financial relationships.
Vishvinder Sharma indicated no relevant financial relationships.
Christina Joya, DO, Luis Muñoz, MD, Megan Hubbard, DO, Masuma Syed, MD, Scott Silver, DO, Vishvinder Sharma, MD. P3949 - Post-Hepatectomy Portal Hypertensive Sequelae Treated With Splenic Embolization and Complicated by Formation of a Large Splenic Pseudocyst, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Valley Hospital Medical Center, Las Vegas, NV
Introduction: A Klatskin tumor is a rare malignancy occurring at the common hepatic duct bifurcation. About two-thirds of Klatskin tumors are resectable, often requiring bile duct resection and less commonly partial hepatectomy. Post-hepatectomy portal hypertension (PHPH) is a known complication with high morbidity and mortality. We present a case of a patient with PHPH who underwent splenic embolization, leading to the rare formation of a large symptomatic splenic pseudocyst.
Case Description/
Methods: 57-year-old male with history of a Klatskin tumor status post partial right hepatectomy presented with syncope, coffee ground emesis, and melena. Labs were significant for Hb 6.0, Hct 21.3, MCV 74.2, PLT 212, AST 39, ALT 37, alkaline phosphatase 226, total bilirubin 1.0, INR 1.2. CT imaging revealed chronic extrahepatic main portal vein occlusion with cavernous transformation, absent middle hepatic vein, gastrorenal shunt, gastric and esophageal varices, and splenomegaly. EGD confirmed gastric and esophageal varices with a large IGV1 gastric varix with high risk bleeding stigmata. Due to the complex anatomy, a transjugular intrahepatic portosystemic shunt (TIPS) procedure was deemed high risk. Coil-assisted or balloon-occluded retrograde transvenous obliteration (CRTO/BRTO) of the gastrorenal shunt was considered, but carried risk of worsening the patient’s esophageal varices. Ultimately, the patient underwent splenic artery embolization (50-60%) to reduce portal pressures and decrease re-bleeding risk. Two months later, the patient presented with left sided abdominal pain, vomiting, and a left pleural effusion. MRI showed an 18x21x23 cm splenic pseudocyst. A percutaneous drain was placed. Fluid cultures grew Enterococcus faecalis, treated with daptomycin.
Discussion: PHPH is linked to poorer long term survival and an increased post-hepatectomy liver failure. The development of PHPH can be predicted by the extent of the liver resection, with larger hepatectomies carrying higher risk. As seen in this case, understanding postsurgical anatomy and portosystemic changes is crucial when planning intervention. Splenic artery embolization is a minimally invasive approach to variceal bleeding, but it is not without risk. Post-embolization symptoms of nausea, vomiting, abdominal pain should be addressed promptly to reduce complications associated with pseudocysts - including superinfections of the cystic fluid. The challenges associated with PHPH and its management present a promising area for further research.
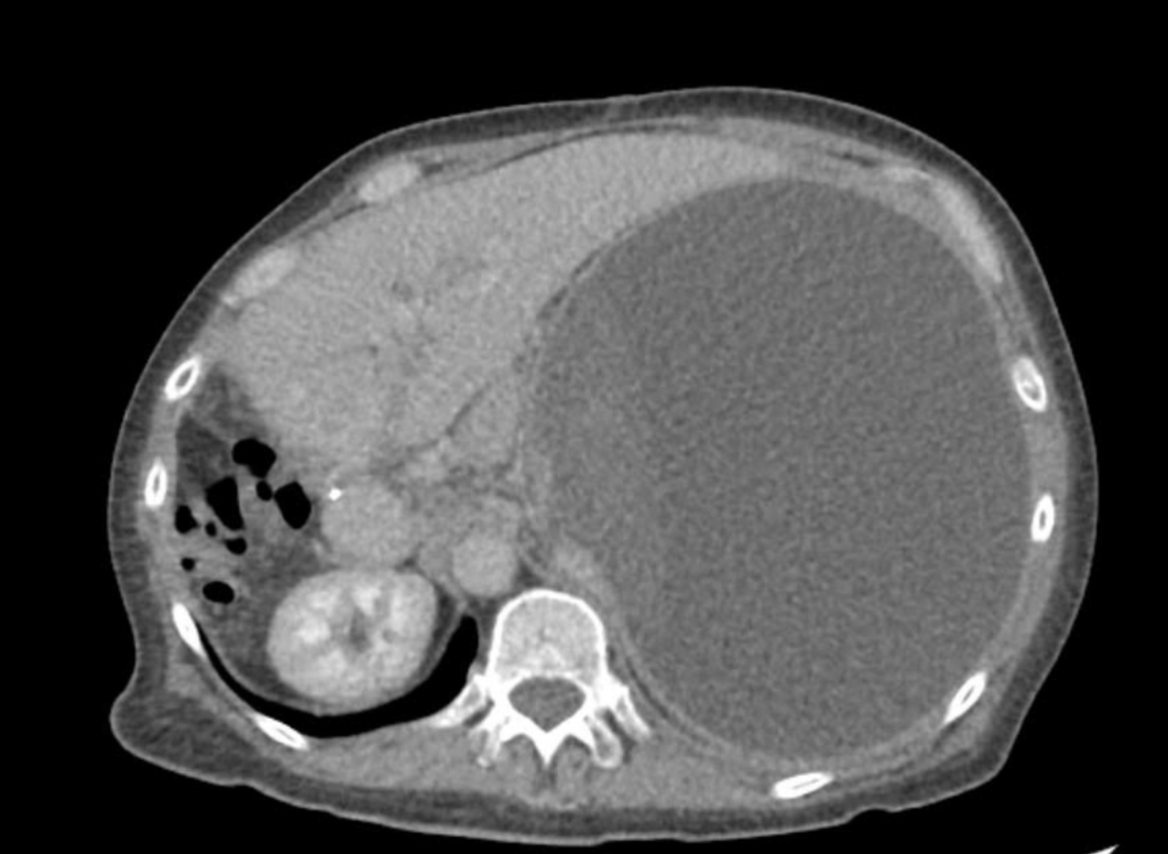
Figure: MRI of the abdomen showing an 18 x 21 x 23 cm splenic pseudocyst.
Disclosures:
Christina Joya indicated no relevant financial relationships.
Luis Muñoz indicated no relevant financial relationships.
Megan Hubbard indicated no relevant financial relationships.
Masuma Syed indicated no relevant financial relationships.
Scott Silver indicated no relevant financial relationships.
Vishvinder Sharma indicated no relevant financial relationships.
Christina Joya, DO, Luis Muñoz, MD, Megan Hubbard, DO, Masuma Syed, MD, Scott Silver, DO, Vishvinder Sharma, MD. P3949 - Post-Hepatectomy Portal Hypertensive Sequelae Treated With Splenic Embolization and Complicated by Formation of a Large Splenic Pseudocyst, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
