Monday Poster Session
Category: Liver
P3947 - Cholangiopathy in the Time of Corona: A Case of Post-COVID Cholangiopathy Resulting in Cirrhosis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Alexander Dile, MD (he/him/his)
University of Cincinnati
Cincinnati, OH
Presenting Author(s)
Alexander Dile, MD1, Ashley Eggert, MD2, Matthew Still, DO2, Anjali Ravee, MD2, Jordan Voss, MD1, Patrick J. Carey, MD1, Divya Sharma, MD2, Khurram Bari, MD1, Amoah Yeboah-Korang, MD1, Michael Schoech, MD1
1University of Cincinnati, Cincinnati, OH; 2University of Cincinnati Medical Center, Cincinnati, OH
Introduction: Post-COVID cholangiopathy is a complication following COVID-19 infection defined by cholestasis and bile duct injury. First reported at the height of the pandemic, it has received limited attention in recent years and is an underrecognized cause of cholestatic liver disease. This case illustrates a delayed presentation identified years after initial infection which resulted in progression to cirrhosis.
Case Description/
Methods: A 45-year-old female with a history of pancreatic neuroendocrine tumor underwent distal pancreatectomy, splenectomy, and partial bowel resection in 2006. She had no hepatologic complications until 2013 when follow-up imaging showed liver lesions concerning for metastatic recurrence although her LFTs remained normal. Liver biopsy showed only steatosis without fibrosis. The patient and her LFTs remained stable until hospitalization for COVID pneumonia in 2/2021. Beginning in 5/2021, she developed persistently elevated ALP (500–1000), mildly elevated AST/ALT (100s), and normal bilirubin. A liver biopsy in 12/2021 showed ductular proliferation, periportal fibrosis (F2), and no granulomas. LFTs remained elevated and a CT in 6/2023 showed normal liver morphology with mild retroperitoneal lymphadenopathy. Repeat biopsy demonstrated bridging fibrosis (F3–4) and chronic cholestasis. IgG4 and fungal stains were negative. MRI in 9/2023 confirmed advanced fibrosis/cirrhosis without features of sclerosing cholangitis. Extensive infectious and autoimmune workup was negative. Sarcoidosis was considered; however, given the absence of granulomas on the liver biopsies and lack of extrahepatic manifestations, this was ruled out. Amyloidosis was considered due to an elevated K/L ratio but ruled out based on lack of monoclonal pattern. PSC and PBC were unlikely given negative antimitochondrial, antinuclear, GP210, and Sp100 autoantibodies, and absence of diagnostic imaging/biopsy findings. DILI was considered but ruled out as no drug timeline fit. Post-COVID cholangiopathy is considered most likely given the timing of LFT rise post-infection and rapid fibrosis progression.
Discussion: Diagnosing post-COVID cholangiopathy remains challenging because of the need to exclude other causes and its non-specific findings. A high index of suspicion and careful history taking are required to elucidate the timing of injury in relation to infection. Improved recognition is needed to further elucidate the underlying pathophysiology and develop therapeutics.
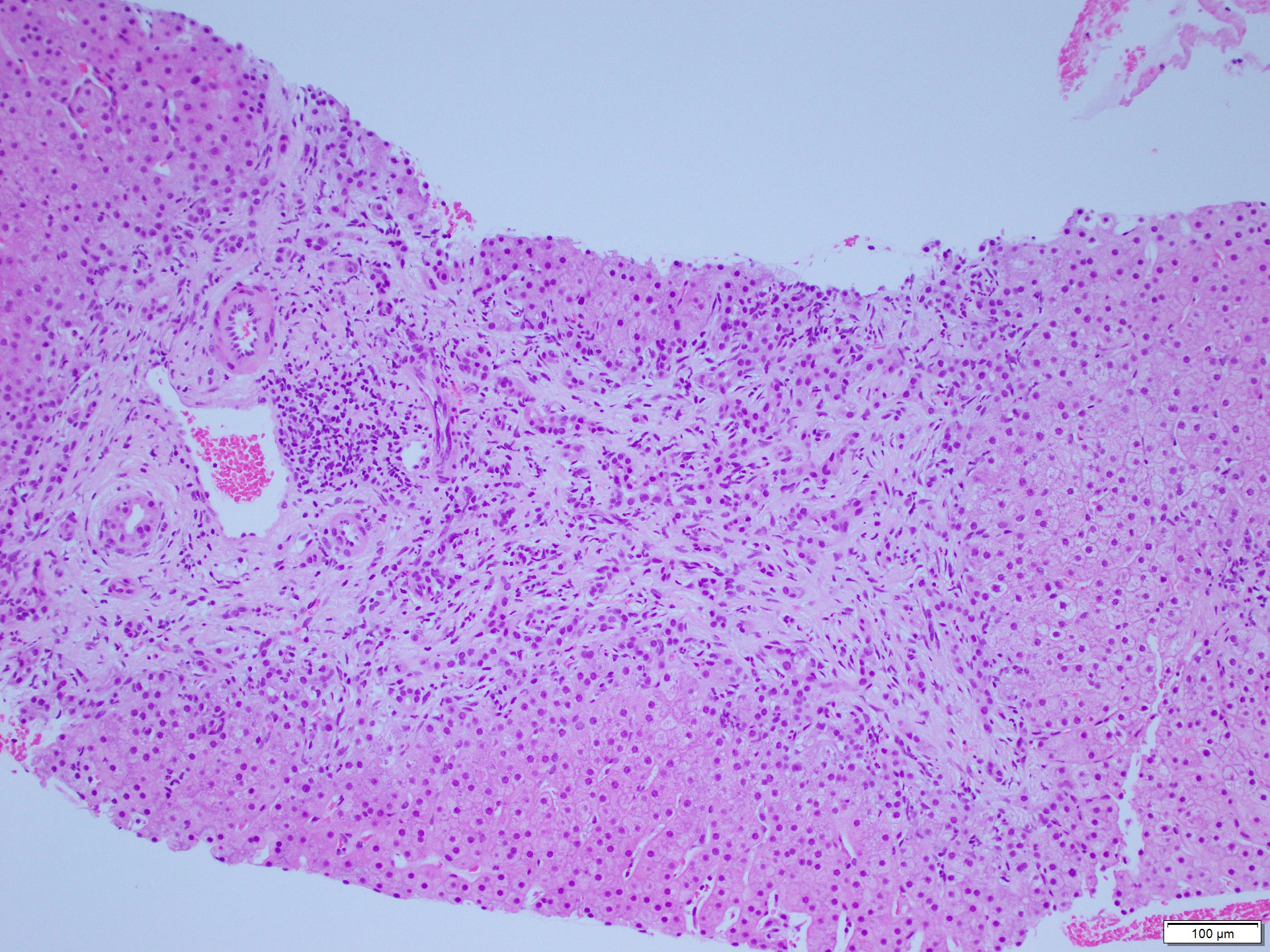
Figure: H&E-stained slide from 2023 liver biopsy showing bridging fibrosis (F3–4) and chronic cholestasis
Disclosures:
Alexander Dile indicated no relevant financial relationships.
Ashley Eggert indicated no relevant financial relationships.
Matthew Still indicated no relevant financial relationships.
Anjali Ravee indicated no relevant financial relationships.
Jordan Voss indicated no relevant financial relationships.
Patrick Carey indicated no relevant financial relationships.
Divya Sharma indicated no relevant financial relationships.
Khurram Bari indicated no relevant financial relationships.
Amoah Yeboah-Korang indicated no relevant financial relationships.
Michael Schoech indicated no relevant financial relationships.
Alexander Dile, MD1, Ashley Eggert, MD2, Matthew Still, DO2, Anjali Ravee, MD2, Jordan Voss, MD1, Patrick J. Carey, MD1, Divya Sharma, MD2, Khurram Bari, MD1, Amoah Yeboah-Korang, MD1, Michael Schoech, MD1. P3947 - Cholangiopathy in the Time of Corona: A Case of Post-COVID Cholangiopathy Resulting in Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Cincinnati, Cincinnati, OH; 2University of Cincinnati Medical Center, Cincinnati, OH
Introduction: Post-COVID cholangiopathy is a complication following COVID-19 infection defined by cholestasis and bile duct injury. First reported at the height of the pandemic, it has received limited attention in recent years and is an underrecognized cause of cholestatic liver disease. This case illustrates a delayed presentation identified years after initial infection which resulted in progression to cirrhosis.
Case Description/
Methods: A 45-year-old female with a history of pancreatic neuroendocrine tumor underwent distal pancreatectomy, splenectomy, and partial bowel resection in 2006. She had no hepatologic complications until 2013 when follow-up imaging showed liver lesions concerning for metastatic recurrence although her LFTs remained normal. Liver biopsy showed only steatosis without fibrosis. The patient and her LFTs remained stable until hospitalization for COVID pneumonia in 2/2021. Beginning in 5/2021, she developed persistently elevated ALP (500–1000), mildly elevated AST/ALT (100s), and normal bilirubin. A liver biopsy in 12/2021 showed ductular proliferation, periportal fibrosis (F2), and no granulomas. LFTs remained elevated and a CT in 6/2023 showed normal liver morphology with mild retroperitoneal lymphadenopathy. Repeat biopsy demonstrated bridging fibrosis (F3–4) and chronic cholestasis. IgG4 and fungal stains were negative. MRI in 9/2023 confirmed advanced fibrosis/cirrhosis without features of sclerosing cholangitis. Extensive infectious and autoimmune workup was negative. Sarcoidosis was considered; however, given the absence of granulomas on the liver biopsies and lack of extrahepatic manifestations, this was ruled out. Amyloidosis was considered due to an elevated K/L ratio but ruled out based on lack of monoclonal pattern. PSC and PBC were unlikely given negative antimitochondrial, antinuclear, GP210, and Sp100 autoantibodies, and absence of diagnostic imaging/biopsy findings. DILI was considered but ruled out as no drug timeline fit. Post-COVID cholangiopathy is considered most likely given the timing of LFT rise post-infection and rapid fibrosis progression.
Discussion: Diagnosing post-COVID cholangiopathy remains challenging because of the need to exclude other causes and its non-specific findings. A high index of suspicion and careful history taking are required to elucidate the timing of injury in relation to infection. Improved recognition is needed to further elucidate the underlying pathophysiology and develop therapeutics.
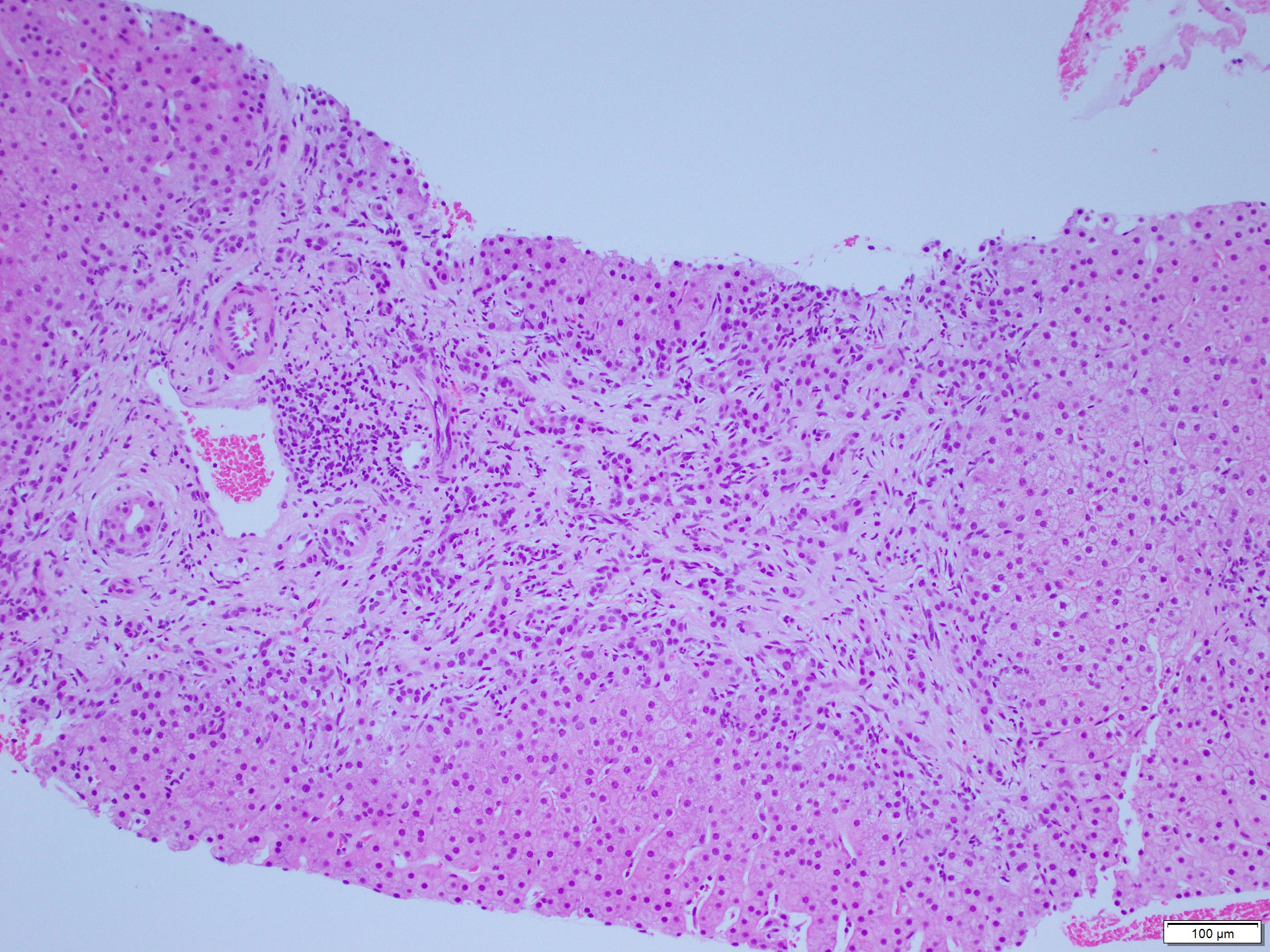
Figure: H&E-stained slide from 2023 liver biopsy showing bridging fibrosis (F3–4) and chronic cholestasis
Disclosures:
Alexander Dile indicated no relevant financial relationships.
Ashley Eggert indicated no relevant financial relationships.
Matthew Still indicated no relevant financial relationships.
Anjali Ravee indicated no relevant financial relationships.
Jordan Voss indicated no relevant financial relationships.
Patrick Carey indicated no relevant financial relationships.
Divya Sharma indicated no relevant financial relationships.
Khurram Bari indicated no relevant financial relationships.
Amoah Yeboah-Korang indicated no relevant financial relationships.
Michael Schoech indicated no relevant financial relationships.
Alexander Dile, MD1, Ashley Eggert, MD2, Matthew Still, DO2, Anjali Ravee, MD2, Jordan Voss, MD1, Patrick J. Carey, MD1, Divya Sharma, MD2, Khurram Bari, MD1, Amoah Yeboah-Korang, MD1, Michael Schoech, MD1. P3947 - Cholangiopathy in the Time of Corona: A Case of Post-COVID Cholangiopathy Resulting in Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

