Monday Poster Session
Category: Small Intestine
P4104 - Gone With the Windsock Diverticulum: A Unique Clinical Presentation Leading to an Incidentally Discovered Intraluminal Duodenal Diverticulum
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Pierce L. Claassen, MD
Mayo Clinic
Scottsdale, AZ
Presenting Author(s)
Pierce L.. Claassen, MD1, Francisco C.. Ramirez, MD, MACG1, Terry L.. Jue, MD2
1Mayo Clinic, Scottsdale, AZ; 2Mayo Clinic Arizona, Scottsdale, AZ
Introduction: Endoscopists often identify incidental abnormalities when performing esophagogastroduodenoscopy (EGD). Intraluminal duodenal diverticuli (IDD) are rare entities with an estimated prevalence of less than 0.05%. Our case highlights an IDD diagnosed during EGD performed to evaluate a lady experiencing changes in bowel habits.
Case Description/
Methods: A 76-year-old-female was referred to gastroenterology for upper endoscopy due to changes in bowel habits. She endorsed diarrheal symptoms without postprandial pain, weight loss, anemia, or obstructive gastrointestinal (GI) symptoms. During EGD, we discovered an inverted IDD, also known as a windsock diverticulum, with an aperture at its apex. Soft, mobile, and with normal mucosa, the IDD arose from the medial wall of the second portion of the duodenum just proximal to the major papilla. We readily advanced the gastroscope into it. We recognized the classic appearance of the IDD and elected not to biopsy. As she did not report symptoms related to mechanical obstruction of the duodenum or major papilla, diverticulotomy or diverticulectomy was not proposed.
Discussion: IDD is a postulated congenital anomaly that arises in the 7th week of embryonic development due to aberrant recanalization of a duodenal diaphragm. Histologically, the tissue is vascular but there have been no cases published that suggest malignant potential. Our clinical vignette describes this uncommon endoscopic finding incidentally discovered during EGD for evaluation of diarrhea. Prior cases of IDD claim that patients may present with obstructive GI symptoms, pancreatitis, or bleeding. We will observe for symptoms of post-prandial duodenal obstruction, pancreatitis, and bleeding; and will consider the IDD as a cause of her diarrhea, though this association has not been reported. Gastroenterologists have performed snare diverticulectomy and have used endoscopic submucosal dissection (ESD) scissors and knives for incisional diverticulotomy. Immediate and delayed bleeding may occur requiring hemostatic clips and electrocautery, and close observation is recommended post intervention. In patients with acute small bowel obstruction, laparoscopic partial duodenectomy may be required. Recognizing this benign anomaly will avoid unnecessary diagnostic CT and endoscopic ultrasound exams and morbidity due to complications from endoscopic resection or surgery.
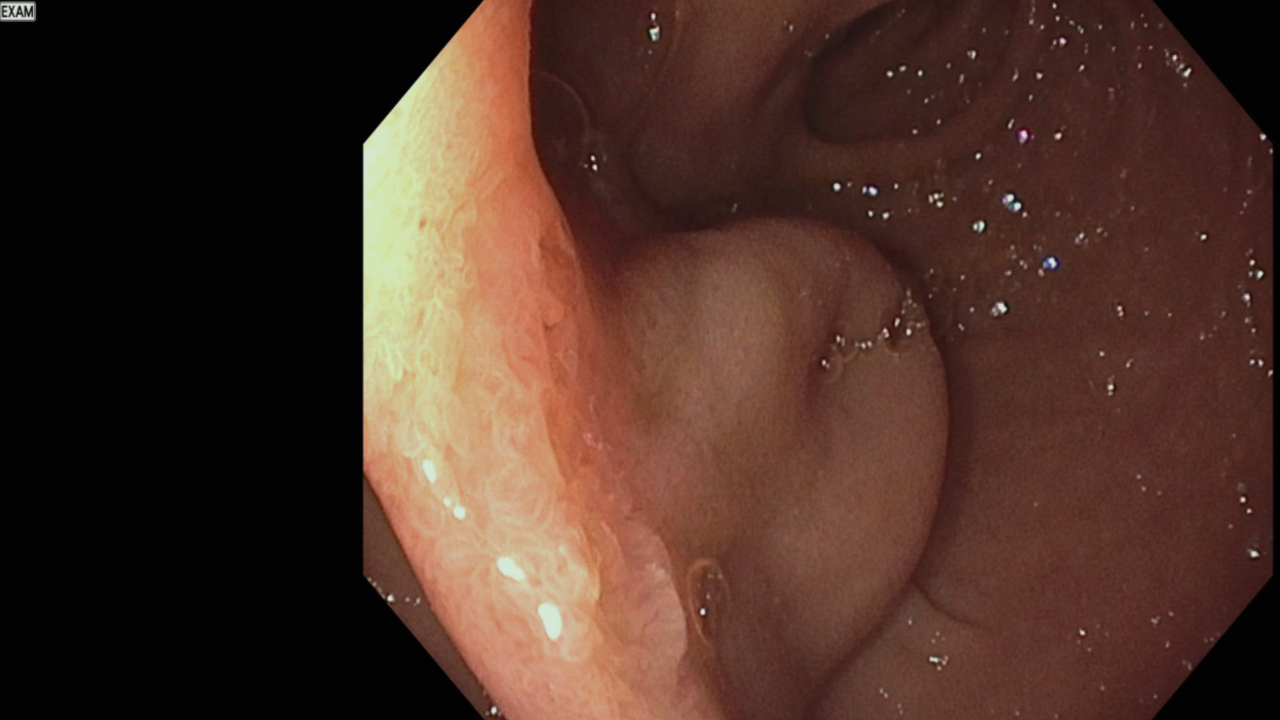
Figure: Endoscopic photograph of the dome and aperture of the IDD extending distally into the second portion of the duodenum.
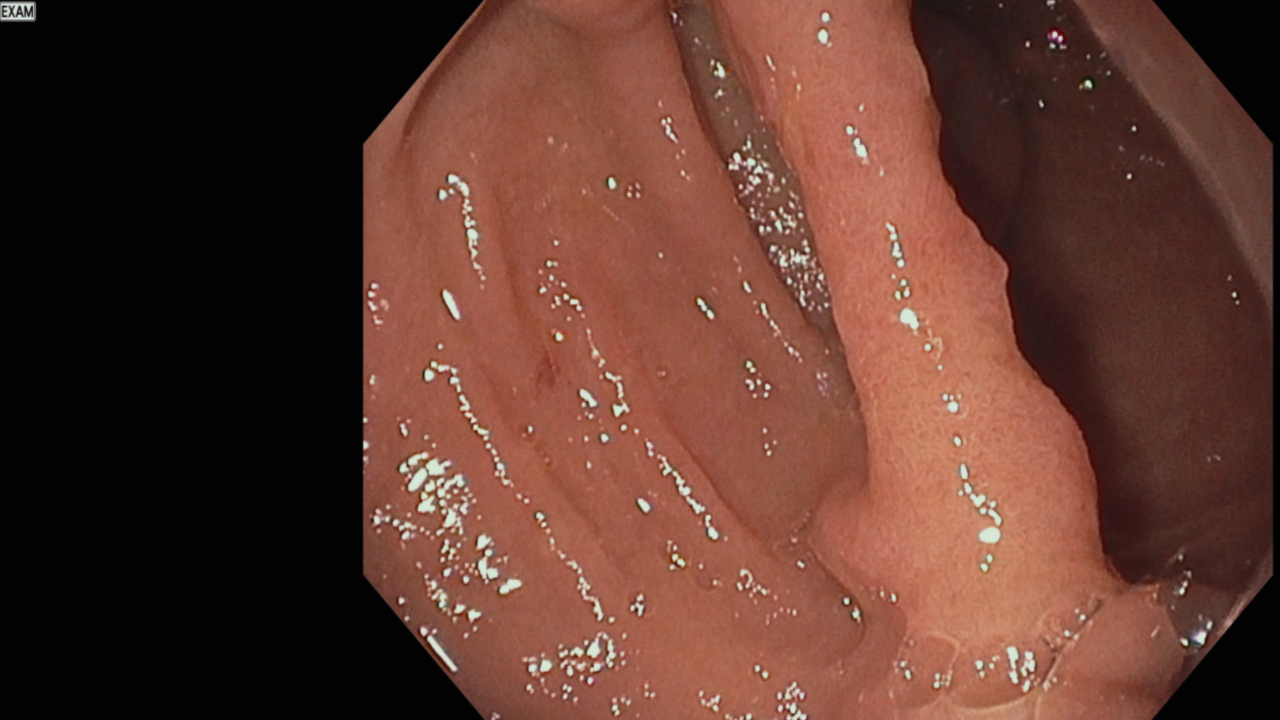
Figure: Endoscopic photograph of the base of the IDD with its proximal afferent origin on the left side of the image and the true duodenal lumen on the right side of the image.
Disclosures:
Pierce Claassen indicated no relevant financial relationships.
Francisco Ramirez indicated no relevant financial relationships.
Terry Jue: Boston Scientific – Jan 2024, Honorarium received for serving as an Instructor at Fellows' Tissue resection course.
Pierce L.. Claassen, MD1, Francisco C.. Ramirez, MD, MACG1, Terry L.. Jue, MD2. P4104 - Gone With the Windsock Diverticulum: A Unique Clinical Presentation Leading to an Incidentally Discovered Intraluminal Duodenal Diverticulum, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mayo Clinic, Scottsdale, AZ; 2Mayo Clinic Arizona, Scottsdale, AZ
Introduction: Endoscopists often identify incidental abnormalities when performing esophagogastroduodenoscopy (EGD). Intraluminal duodenal diverticuli (IDD) are rare entities with an estimated prevalence of less than 0.05%. Our case highlights an IDD diagnosed during EGD performed to evaluate a lady experiencing changes in bowel habits.
Case Description/
Methods: A 76-year-old-female was referred to gastroenterology for upper endoscopy due to changes in bowel habits. She endorsed diarrheal symptoms without postprandial pain, weight loss, anemia, or obstructive gastrointestinal (GI) symptoms. During EGD, we discovered an inverted IDD, also known as a windsock diverticulum, with an aperture at its apex. Soft, mobile, and with normal mucosa, the IDD arose from the medial wall of the second portion of the duodenum just proximal to the major papilla. We readily advanced the gastroscope into it. We recognized the classic appearance of the IDD and elected not to biopsy. As she did not report symptoms related to mechanical obstruction of the duodenum or major papilla, diverticulotomy or diverticulectomy was not proposed.
Discussion: IDD is a postulated congenital anomaly that arises in the 7th week of embryonic development due to aberrant recanalization of a duodenal diaphragm. Histologically, the tissue is vascular but there have been no cases published that suggest malignant potential. Our clinical vignette describes this uncommon endoscopic finding incidentally discovered during EGD for evaluation of diarrhea. Prior cases of IDD claim that patients may present with obstructive GI symptoms, pancreatitis, or bleeding. We will observe for symptoms of post-prandial duodenal obstruction, pancreatitis, and bleeding; and will consider the IDD as a cause of her diarrhea, though this association has not been reported. Gastroenterologists have performed snare diverticulectomy and have used endoscopic submucosal dissection (ESD) scissors and knives for incisional diverticulotomy. Immediate and delayed bleeding may occur requiring hemostatic clips and electrocautery, and close observation is recommended post intervention. In patients with acute small bowel obstruction, laparoscopic partial duodenectomy may be required. Recognizing this benign anomaly will avoid unnecessary diagnostic CT and endoscopic ultrasound exams and morbidity due to complications from endoscopic resection or surgery.
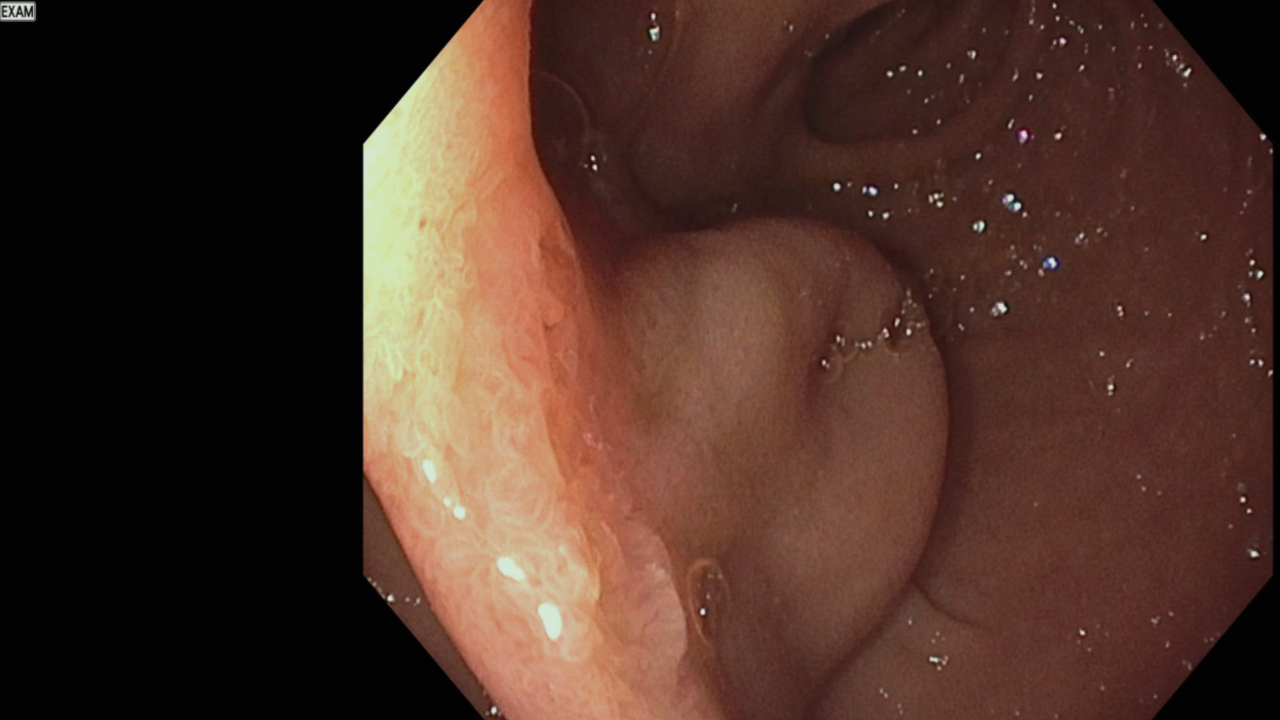
Figure: Endoscopic photograph of the dome and aperture of the IDD extending distally into the second portion of the duodenum.
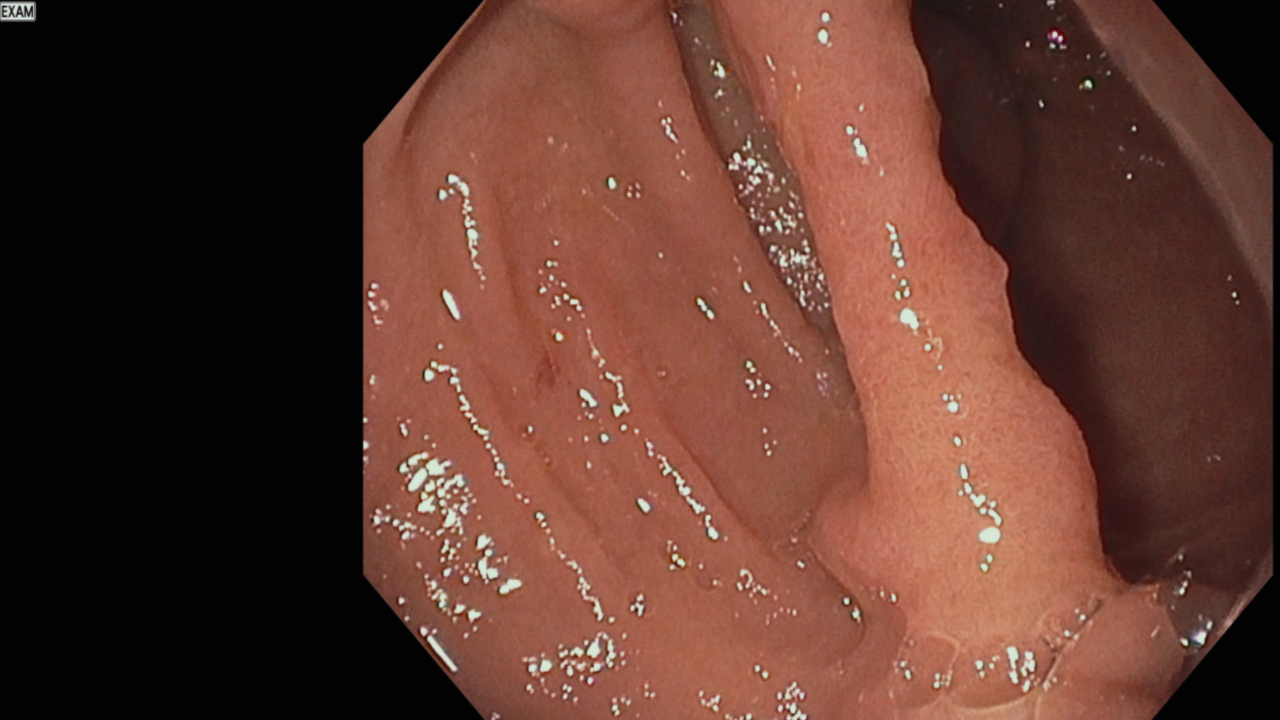
Figure: Endoscopic photograph of the base of the IDD with its proximal afferent origin on the left side of the image and the true duodenal lumen on the right side of the image.
Disclosures:
Pierce Claassen indicated no relevant financial relationships.
Francisco Ramirez indicated no relevant financial relationships.
Terry Jue: Boston Scientific – Jan 2024, Honorarium received for serving as an Instructor at Fellows' Tissue resection course.
Pierce L.. Claassen, MD1, Francisco C.. Ramirez, MD, MACG1, Terry L.. Jue, MD2. P4104 - Gone With the Windsock Diverticulum: A Unique Clinical Presentation Leading to an Incidentally Discovered Intraluminal Duodenal Diverticulum, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

