Monday Poster Session
Category: Small Intestine
P4092 - An Unusual Cause of Gastric Outlet Obstruction: Gastric Heterotopic Mucosa After Gastroduodenal Embolization
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- YR
Yasamin Rastgar, BSA
John Sealy School of Medicine, University of Texas Medical Branch
Galveston, TX
Presenting Author(s)
Migara Jayasekera, MD1, Yasamin Rastgar, BSA2, Christo Mathew, MD3
1University of Texas Medical Branch, Galveston, TX; 2John Sealy School of Medicine, University of Texas Medical Branch, Galveston, TX; 3University of Texas Medical Branch, Department of Gastroenterology and Hepatology, Galveston, TX
Introduction: Gastric outlet obstruction (GOO) occurs when a blockage impairs gastric emptying, often affecting the distal stomach, pylorus, or proximal duodenum. While malignancy causes most modern cases, benign etiologies—such as peptic ulcer disease (PUD), Crohn's disease, NSAID-induced strictures, or bezoars—remain relevant. We present a rare mechanical cause of GOO due to gastric heterotopic mucosa, likely linked to prior ischemic injury.
Case Description/
Methods: A 60-year-old incarcerated male with decompensated cirrhosis, prior upper gastrointestinal (GI) bleeding treated by gastroduodenal embolization, and chronic hepatitis C presented with 12 days of persistent nausea and vomiting. He vomited multiple times daily without relief from antiemetics. On admission, the patient had a leukocytosis, hypokalemia (2.4 mmol/L), hypochloremia (64 mmol/L), and acute pre-renal kidney injury. Abdominal computed tomography (CT) revealed gastric distension with air-fluid levels, raising suspicion for GOO. The patient received conservative treatment for the small bowel obstruction. Esophagogastroduodenoscopy (EGD) revealed obstructing lesions in the duodenal bulb. Biopsy of the lesion showed gastric heterotopic mucosa with ulceration and reactive changes. A second EGD revealed a 2.5 cm stricture at D1/D2 with 90% luminal narrowing. Repeat biopsies taken to rule out malignancy again revealed heterotopic mucosa. We suspected the stricture resulted from ischemia due to embolization or post-ulcer fibrosis, given the proximity to the embolized site. Attempts to deploy a luminal stent failed due to the severity of narrowing, thus, surgery was consulted for gastrojejunostomy and vagotomy. The patient's symptoms resolved shortly post-operatively.
Discussion: This case underscores a rare cause of GOO not evident on imaging and demonstrates the critical role of endoscopy in diagnosing and guiding management. We confirmed the mechanical obstruction from heterotopic gastric mucosa and navigated a complex clinical scenario through a multidisciplinary approach. This case also demonstrates the potential risk of stricturing and obstruction due to gastrointestinal embolizations, a common practice in cases of hemorrhage.
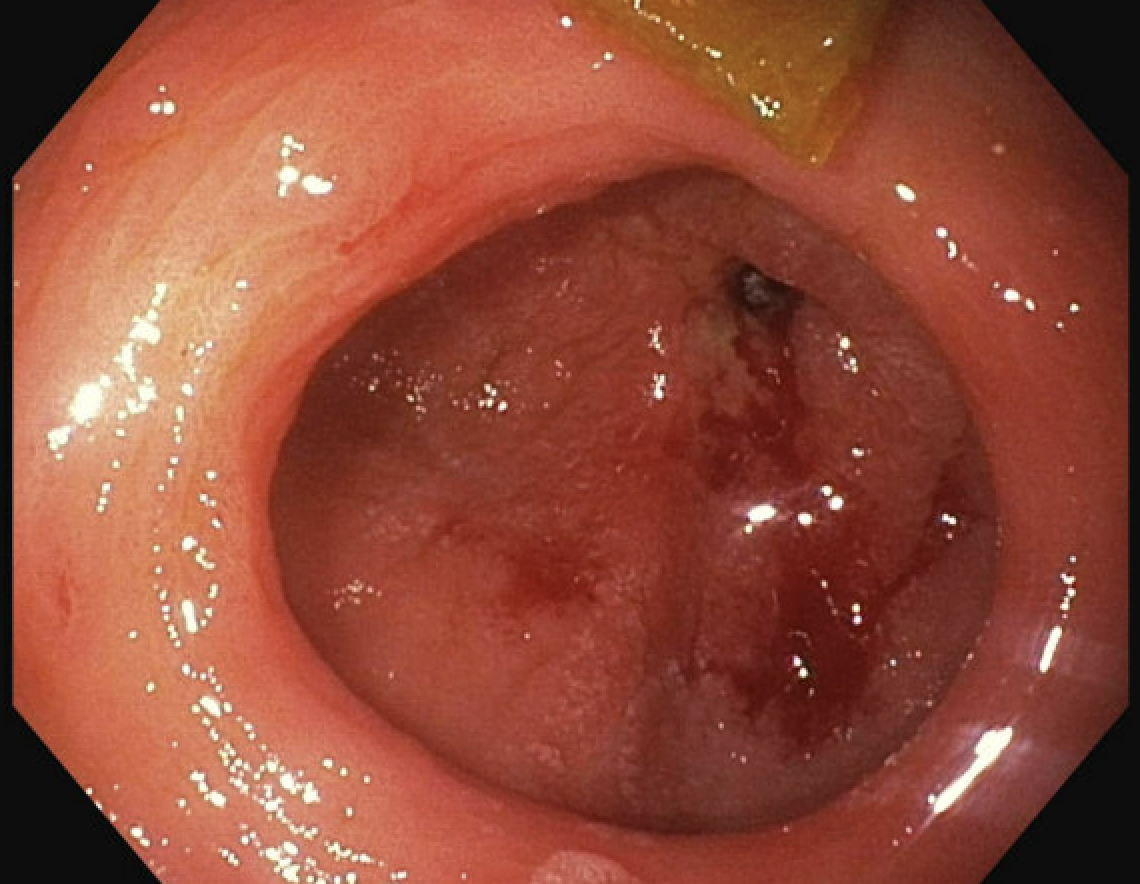
Figure: EGD visualization of Duodenal bulb stricture
Disclosures:
Migara Jayasekera indicated no relevant financial relationships.
Yasamin Rastgar indicated no relevant financial relationships.
Christo Mathew indicated no relevant financial relationships.
Migara Jayasekera, MD1, Yasamin Rastgar, BSA2, Christo Mathew, MD3. P4092 - An Unusual Cause of Gastric Outlet Obstruction: Gastric Heterotopic Mucosa After Gastroduodenal Embolization, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas Medical Branch, Galveston, TX; 2John Sealy School of Medicine, University of Texas Medical Branch, Galveston, TX; 3University of Texas Medical Branch, Department of Gastroenterology and Hepatology, Galveston, TX
Introduction: Gastric outlet obstruction (GOO) occurs when a blockage impairs gastric emptying, often affecting the distal stomach, pylorus, or proximal duodenum. While malignancy causes most modern cases, benign etiologies—such as peptic ulcer disease (PUD), Crohn's disease, NSAID-induced strictures, or bezoars—remain relevant. We present a rare mechanical cause of GOO due to gastric heterotopic mucosa, likely linked to prior ischemic injury.
Case Description/
Methods: A 60-year-old incarcerated male with decompensated cirrhosis, prior upper gastrointestinal (GI) bleeding treated by gastroduodenal embolization, and chronic hepatitis C presented with 12 days of persistent nausea and vomiting. He vomited multiple times daily without relief from antiemetics. On admission, the patient had a leukocytosis, hypokalemia (2.4 mmol/L), hypochloremia (64 mmol/L), and acute pre-renal kidney injury. Abdominal computed tomography (CT) revealed gastric distension with air-fluid levels, raising suspicion for GOO. The patient received conservative treatment for the small bowel obstruction. Esophagogastroduodenoscopy (EGD) revealed obstructing lesions in the duodenal bulb. Biopsy of the lesion showed gastric heterotopic mucosa with ulceration and reactive changes. A second EGD revealed a 2.5 cm stricture at D1/D2 with 90% luminal narrowing. Repeat biopsies taken to rule out malignancy again revealed heterotopic mucosa. We suspected the stricture resulted from ischemia due to embolization or post-ulcer fibrosis, given the proximity to the embolized site. Attempts to deploy a luminal stent failed due to the severity of narrowing, thus, surgery was consulted for gastrojejunostomy and vagotomy. The patient's symptoms resolved shortly post-operatively.
Discussion: This case underscores a rare cause of GOO not evident on imaging and demonstrates the critical role of endoscopy in diagnosing and guiding management. We confirmed the mechanical obstruction from heterotopic gastric mucosa and navigated a complex clinical scenario through a multidisciplinary approach. This case also demonstrates the potential risk of stricturing and obstruction due to gastrointestinal embolizations, a common practice in cases of hemorrhage.
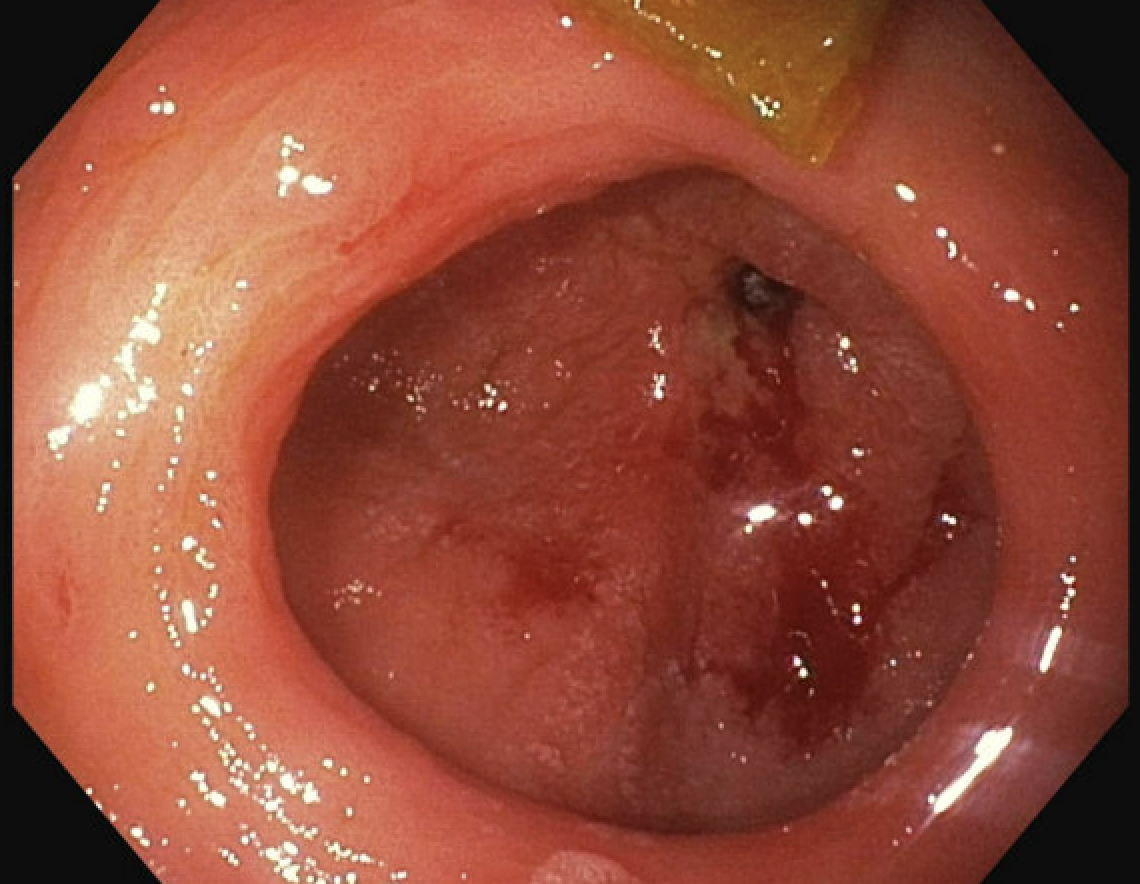
Figure: EGD visualization of Duodenal bulb stricture
Disclosures:
Migara Jayasekera indicated no relevant financial relationships.
Yasamin Rastgar indicated no relevant financial relationships.
Christo Mathew indicated no relevant financial relationships.
Migara Jayasekera, MD1, Yasamin Rastgar, BSA2, Christo Mathew, MD3. P4092 - An Unusual Cause of Gastric Outlet Obstruction: Gastric Heterotopic Mucosa After Gastroduodenal Embolization, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

