Monday Poster Session
Category: Small Intestine
P4087 - Post-Traumatic Duodenal Compression from Retroperitoneal Hematoma Causing Delayed Gastric Outlet Obstruction: A Diagnostic and Nutritional Challenge
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Tushaar V. Shrimanker, MD, MRCP (he/him/his)
University of Massachusetts Chan Medical School-Baystate Medical Center
Enfield, CT
Presenting Author(s)
Tushaar V. Shrimanker, MD, MRCP1, Syed Hamza Sohail, MD2, Aizaz Khan, MD2, Cristina Batarseh, MD3, Kevin Groudan, MD4, Tiago Martins, DO2, Rony Ghaoui, MD5
1University of Massachusetts Chan Medical School-Baystate Medical Center, Enfield, CT; 2University of Massachusetts Chan Medical School - Baystate Health, Springfield, MA; 3University of Massachusetts Chan Medical School-Baystate Medical Center, Chicopee, MA; 4University of Massachusetts Chan Medical School - Baystate Health, East Windsor, CT; 5University of Massachusetts Chan Medical School - Baystate Health, Westfield, MA
Introduction: Gastric outlet obstruction (GOO) is commonly associated with peptic ulcer disease or malignancy but may also occur due to extrinsic compression. Retroperitoneal hematomas following blunt abdominal trauma are an uncommon but important cause of delayed GOO. We present a case of GOO secondary to duodenal compression from a periduodenal hematoma following a kayaking injury.
Case Description/
Methods: A 66-year-old woman presented with progressive abdominal pain, nausea, and vomiting following blunt abdominal trauma sustained during a kayaking incident. Initial CT imaging at an outside facility showed a periduodenal hematoma and hemoperitoneum. She was transferred for trauma evaluation and initially managed conservatively with analgesia. An upper GI series showed a normal duodenal contour, and she was discharged with symptomatic improvement.
However, 8 days post-discharge, she experienced recurrent symptoms after ingesting food, followed by vomiting, back pain, and decreased bowel movements. Repeat CT revealed interval reduction in hematoma size but continued evidence of narrowing in the second/third portions of the duodenum, with mild gastric distention concerning for partial GOO.
Upper endoscopy revealed erosive esophagitis and retained food debris. The duodenum showed external compression at the D2/D3 junction, preventing endoscope passage. Fluoroscopy-guided contrast injection confirmed a 5 cm duodenal stricture (Figure 1a). A guidewire was advanced into the jejunum, and a nasojejunal (NJ) tube was placed for enteral nutrition (Figure 1b). Gastric decompression via NG tube was used to assist NJ tube advancement.
Subsequent imaging showed continued hematoma resolution. Despite this, initial clamping trials failed but repeat imaging and monitoring of symptoms led to gradual diet advancement. She was discharged in stable condition 11 days after re-admission.
Discussion: This case illustrates a rare cause of GOO due to extrinsic duodenal compression from a traumatic hematoma. Notably, symptoms worsened despite radiologic improvement, possibly due to reactive inflammation or duodenal wall thickening. NJ tube placement allowed for enteral nutrition while avoiding surgery. Clinicians should consider delayed duodenal obstruction in trauma patients presenting with GOO-like symptoms, even after initial improvement. Careful radiologic follow-up and endoscopic assessment are important for appropriate nutritional and therapeutic planning.
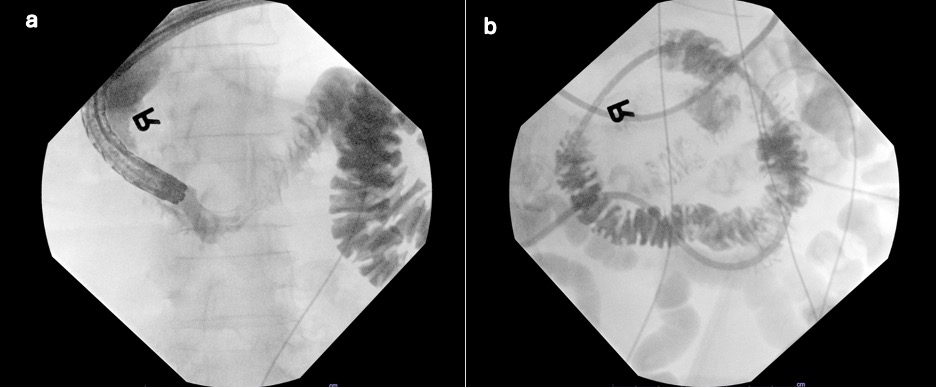
Figure: Figure 1 a) Fluoroscopy during endoscopy showing duodenal stricture. b) Wire-guided placement of nasojejunal tube traversing stricture.
Disclosures:
Tushaar Shrimanker indicated no relevant financial relationships.
Syed Hamza Sohail indicated no relevant financial relationships.
Aizaz Khan indicated no relevant financial relationships.
Cristina Batarseh indicated no relevant financial relationships.
Kevin Groudan indicated no relevant financial relationships.
Tiago Martins indicated no relevant financial relationships.
Rony Ghaoui indicated no relevant financial relationships.
Tushaar V. Shrimanker, MD, MRCP1, Syed Hamza Sohail, MD2, Aizaz Khan, MD2, Cristina Batarseh, MD3, Kevin Groudan, MD4, Tiago Martins, DO2, Rony Ghaoui, MD5. P4087 - Post-Traumatic Duodenal Compression from Retroperitoneal Hematoma Causing Delayed Gastric Outlet Obstruction: A Diagnostic and Nutritional Challenge, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Massachusetts Chan Medical School-Baystate Medical Center, Enfield, CT; 2University of Massachusetts Chan Medical School - Baystate Health, Springfield, MA; 3University of Massachusetts Chan Medical School-Baystate Medical Center, Chicopee, MA; 4University of Massachusetts Chan Medical School - Baystate Health, East Windsor, CT; 5University of Massachusetts Chan Medical School - Baystate Health, Westfield, MA
Introduction: Gastric outlet obstruction (GOO) is commonly associated with peptic ulcer disease or malignancy but may also occur due to extrinsic compression. Retroperitoneal hematomas following blunt abdominal trauma are an uncommon but important cause of delayed GOO. We present a case of GOO secondary to duodenal compression from a periduodenal hematoma following a kayaking injury.
Case Description/
Methods: A 66-year-old woman presented with progressive abdominal pain, nausea, and vomiting following blunt abdominal trauma sustained during a kayaking incident. Initial CT imaging at an outside facility showed a periduodenal hematoma and hemoperitoneum. She was transferred for trauma evaluation and initially managed conservatively with analgesia. An upper GI series showed a normal duodenal contour, and she was discharged with symptomatic improvement.
However, 8 days post-discharge, she experienced recurrent symptoms after ingesting food, followed by vomiting, back pain, and decreased bowel movements. Repeat CT revealed interval reduction in hematoma size but continued evidence of narrowing in the second/third portions of the duodenum, with mild gastric distention concerning for partial GOO.
Upper endoscopy revealed erosive esophagitis and retained food debris. The duodenum showed external compression at the D2/D3 junction, preventing endoscope passage. Fluoroscopy-guided contrast injection confirmed a 5 cm duodenal stricture (Figure 1a). A guidewire was advanced into the jejunum, and a nasojejunal (NJ) tube was placed for enteral nutrition (Figure 1b). Gastric decompression via NG tube was used to assist NJ tube advancement.
Subsequent imaging showed continued hematoma resolution. Despite this, initial clamping trials failed but repeat imaging and monitoring of symptoms led to gradual diet advancement. She was discharged in stable condition 11 days after re-admission.
Discussion: This case illustrates a rare cause of GOO due to extrinsic duodenal compression from a traumatic hematoma. Notably, symptoms worsened despite radiologic improvement, possibly due to reactive inflammation or duodenal wall thickening. NJ tube placement allowed for enteral nutrition while avoiding surgery. Clinicians should consider delayed duodenal obstruction in trauma patients presenting with GOO-like symptoms, even after initial improvement. Careful radiologic follow-up and endoscopic assessment are important for appropriate nutritional and therapeutic planning.
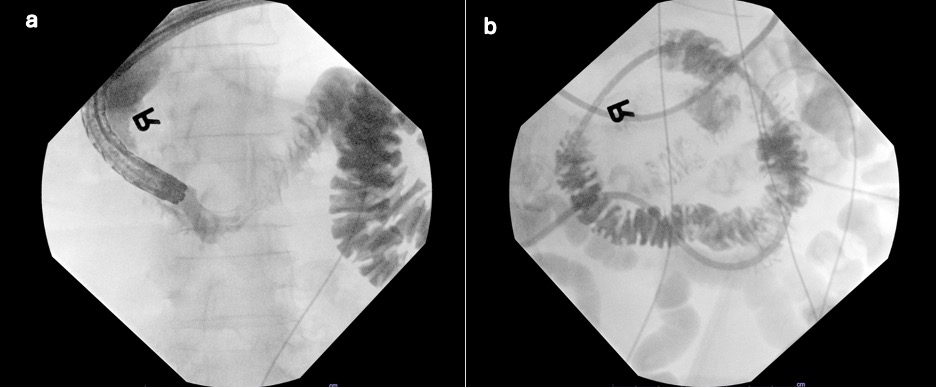
Figure: Figure 1 a) Fluoroscopy during endoscopy showing duodenal stricture. b) Wire-guided placement of nasojejunal tube traversing stricture.
Disclosures:
Tushaar Shrimanker indicated no relevant financial relationships.
Syed Hamza Sohail indicated no relevant financial relationships.
Aizaz Khan indicated no relevant financial relationships.
Cristina Batarseh indicated no relevant financial relationships.
Kevin Groudan indicated no relevant financial relationships.
Tiago Martins indicated no relevant financial relationships.
Rony Ghaoui indicated no relevant financial relationships.
Tushaar V. Shrimanker, MD, MRCP1, Syed Hamza Sohail, MD2, Aizaz Khan, MD2, Cristina Batarseh, MD3, Kevin Groudan, MD4, Tiago Martins, DO2, Rony Ghaoui, MD5. P4087 - Post-Traumatic Duodenal Compression from Retroperitoneal Hematoma Causing Delayed Gastric Outlet Obstruction: A Diagnostic and Nutritional Challenge, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
