Monday Poster Session
Category: Stomach and Spleen
P4170 - Comparative Efficacy of Endoscopic and Surgical Interventions for Gastroparesis: A Systematic Review and Network Meta-Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ismail Althunibat, MD
New York Medical College - Saint Michael's Medical Center
Newark, NJ
Presenting Author(s)
Ismail Althunibat, MD1, Yahya Alhalalmeh, MD1, Thai Hau Koo, MD2, Muhammad Elsharkawy, MD3, Ahmad Alomari, MD4, Murad Qirem, MD5, Mohamed Eldesouki, MD6, Theodore DaCosta, Jr., MD1, Yatinder Bains, MD1, Brian Ginnebaugh, MD4, Ala Abdel-Jalil, MD7, Yaseen Alastal, MD8
1New York Medical College - Saint Michael's Medical Center, Newark, NJ; 2University of Sciences Malaysia Specialist Hospital, Kelantan, Kelantan, Malaysia; 3Alexandria University, Alexandria, Al Iskandariyah, Egypt; 4Henry Ford Health, Detroit, MI; 5New York Medical College - Saint Michael's Medical Center, West Orange, NJ; 6Saint Michael's Medical Center, New York Medical College, Newark, NJ; 7Case Western Reserve University / MetroHealth, Cleveland, OH; 8University of Toledo, Toledo, OH
Introduction: Gastroparesis is a chronic gastrointestinal motility disorder with limited response to pharmacologic therapy. Procedural interventions—including endoscopic and surgical approaches—have emerged as alternatives, but comparative data remain sparse. This network meta-analysis evaluated the relative efficacy of these procedural options for gastroparesis.
Methods: We systematically searched PubMed, Embase, and CENTRAL from January 2000 to present for randomized and observational studies assessing procedural interventions in adults with gastroparesis. Interventions included gastric peroral endoscopic myotomy (GPOEM), pyloroplasty/pyloromyotomy, gastric neuronal stimulation (GNS), botulinum toxin injection (BTI), and combination therapies. Primary outcomes were clinical success and gastric emptying study (GES) improvement. A Bayesian network meta-analysis with a common-effects model was used. SUCRA values ranked treatment efficacy.
Results: 49 studies comprising 2722 patients were included in the study. For clinical success, 12 studies (k=12) across 6 treatments (n=6) and 6 unique study designs (d=6) contributed 12 pairwise comparisons (m=12). Compared to placebo, GPOEM showed the highest odds of clinical success (OR 5.72, 95% CI 2.02–16.18, p=0.0010; SUCRA=0.85), followed closely by GPOEM + GES (OR 5.42, 95% CI 1.47–19.99, p=0.0111; SUCRA=0.79) and pyloroplasty (OR 4.64, 95% CI 1.46–14.75, p=0.0093; SUCRA=0.71). BTI and GNS did not demonstrate a statistically significant benefit. For GES improvement, 8 studies (k=8) evaluated 7 treatments (n=7) with 6 designs (d=6), contributing 8 pairwise comparisons (m=8). In comparisons against sham procedures for gastric emptying improvement, pyloroplasty + GES ranked the highest (OR 100.0, 95% CI, 5.79–1728.15; p=0.0015; SUCRA=0.97), followed by GPOEM (OR 13.33, 95% CI 2.82–63.11, p=0.0011; SUCRA=0.69), and GPOEM+GES (OR 11.93, 95% CI 1.47–96.76, p=0.0203; SUCRA=0.63). BTI and GES remained the lowest-performing interventions across both primary outcomes.
Discussion: GPOEM, either alone or combined with GNS, offers the strongest evidence for symptom relief and significant improvement in gastric emptying. Pyloroplasty-based therapies also demonstrate high efficacy, particularly for GES outcomes. In contrast, BTI and GNS rank lowest, suggesting limited utility.These findings support GPOEM and pyloroplasty as preferred procedural options in refractory gastroparesis.GES improvement didn’t consistently match symptom relief, limiting its surrogate value.
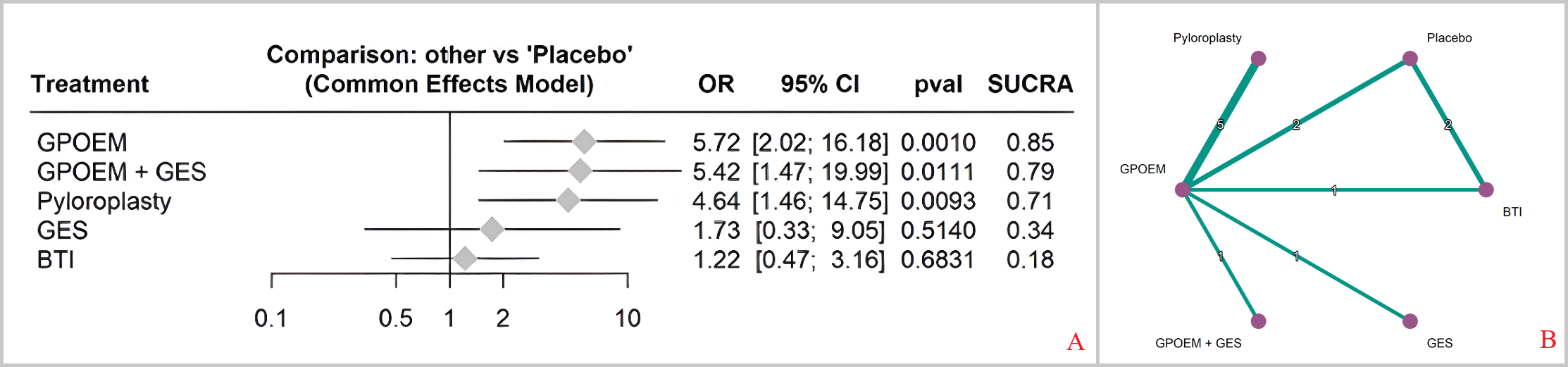
Figure: Figure (1): [A] Forest plot of clinical success (ORs vs Placebo) comparing interventions against placebo. GPOEM and GPOEM+GES were associated with the highest odds of clinical response.
[B] Network geometry of procedural interventions for gastroparesis with clinical success as the primary outcome
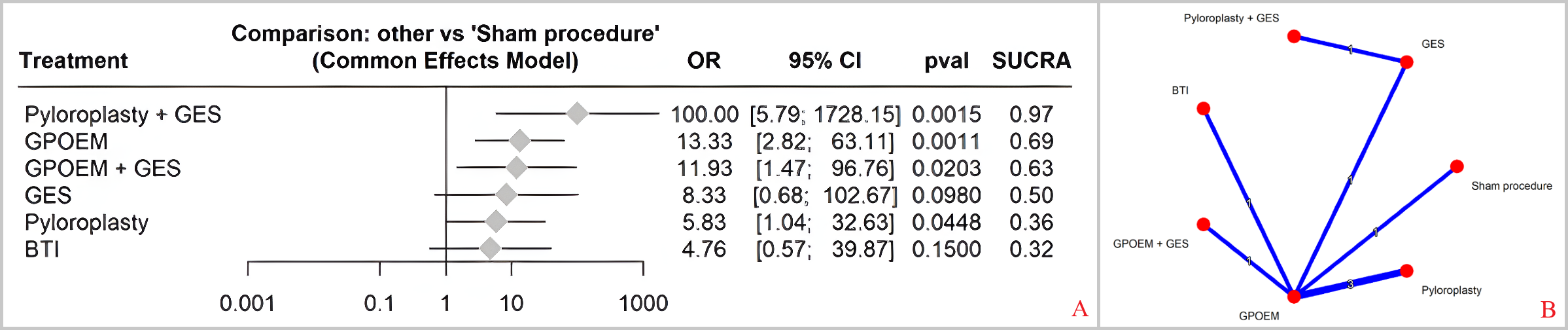
Figure: Figure (2): [A] Forest plot comparing improvement in gastric emptying among interventions relative to sham (ORs vs Sham). Pyloroplasty + GES and GPOEM demonstrated the greatest effect sizes.
[B] Network Plot: Gastric Emptying Improvement. Network plot of interventions evaluated for gastric emptying test (GET) improvement.
Disclosures:
Ismail Althunibat indicated no relevant financial relationships.
Yahya Alhalalmeh indicated no relevant financial relationships.
Thai Hau Koo indicated no relevant financial relationships.
Muhammad Elsharkawy indicated no relevant financial relationships.
Ahmad Alomari indicated no relevant financial relationships.
Murad Qirem indicated no relevant financial relationships.
Mohamed Eldesouki indicated no relevant financial relationships.
Theodore DaCosta, Jr. indicated no relevant financial relationships.
Yatinder Bains indicated no relevant financial relationships.
Brian Ginnebaugh: Ardelyx – Speakers Bureau.
Ala Abdel-Jalil indicated no relevant financial relationships.
Yaseen Alastal indicated no relevant financial relationships.
Ismail Althunibat, MD1, Yahya Alhalalmeh, MD1, Thai Hau Koo, MD2, Muhammad Elsharkawy, MD3, Ahmad Alomari, MD4, Murad Qirem, MD5, Mohamed Eldesouki, MD6, Theodore DaCosta, Jr., MD1, Yatinder Bains, MD1, Brian Ginnebaugh, MD4, Ala Abdel-Jalil, MD7, Yaseen Alastal, MD8. P4170 - Comparative Efficacy of Endoscopic and Surgical Interventions for Gastroparesis: A Systematic Review and Network Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1New York Medical College - Saint Michael's Medical Center, Newark, NJ; 2University of Sciences Malaysia Specialist Hospital, Kelantan, Kelantan, Malaysia; 3Alexandria University, Alexandria, Al Iskandariyah, Egypt; 4Henry Ford Health, Detroit, MI; 5New York Medical College - Saint Michael's Medical Center, West Orange, NJ; 6Saint Michael's Medical Center, New York Medical College, Newark, NJ; 7Case Western Reserve University / MetroHealth, Cleveland, OH; 8University of Toledo, Toledo, OH
Introduction: Gastroparesis is a chronic gastrointestinal motility disorder with limited response to pharmacologic therapy. Procedural interventions—including endoscopic and surgical approaches—have emerged as alternatives, but comparative data remain sparse. This network meta-analysis evaluated the relative efficacy of these procedural options for gastroparesis.
Methods: We systematically searched PubMed, Embase, and CENTRAL from January 2000 to present for randomized and observational studies assessing procedural interventions in adults with gastroparesis. Interventions included gastric peroral endoscopic myotomy (GPOEM), pyloroplasty/pyloromyotomy, gastric neuronal stimulation (GNS), botulinum toxin injection (BTI), and combination therapies. Primary outcomes were clinical success and gastric emptying study (GES) improvement. A Bayesian network meta-analysis with a common-effects model was used. SUCRA values ranked treatment efficacy.
Results: 49 studies comprising 2722 patients were included in the study. For clinical success, 12 studies (k=12) across 6 treatments (n=6) and 6 unique study designs (d=6) contributed 12 pairwise comparisons (m=12). Compared to placebo, GPOEM showed the highest odds of clinical success (OR 5.72, 95% CI 2.02–16.18, p=0.0010; SUCRA=0.85), followed closely by GPOEM + GES (OR 5.42, 95% CI 1.47–19.99, p=0.0111; SUCRA=0.79) and pyloroplasty (OR 4.64, 95% CI 1.46–14.75, p=0.0093; SUCRA=0.71). BTI and GNS did not demonstrate a statistically significant benefit. For GES improvement, 8 studies (k=8) evaluated 7 treatments (n=7) with 6 designs (d=6), contributing 8 pairwise comparisons (m=8). In comparisons against sham procedures for gastric emptying improvement, pyloroplasty + GES ranked the highest (OR 100.0, 95% CI, 5.79–1728.15; p=0.0015; SUCRA=0.97), followed by GPOEM (OR 13.33, 95% CI 2.82–63.11, p=0.0011; SUCRA=0.69), and GPOEM+GES (OR 11.93, 95% CI 1.47–96.76, p=0.0203; SUCRA=0.63). BTI and GES remained the lowest-performing interventions across both primary outcomes.
Discussion: GPOEM, either alone or combined with GNS, offers the strongest evidence for symptom relief and significant improvement in gastric emptying. Pyloroplasty-based therapies also demonstrate high efficacy, particularly for GES outcomes. In contrast, BTI and GNS rank lowest, suggesting limited utility.These findings support GPOEM and pyloroplasty as preferred procedural options in refractory gastroparesis.GES improvement didn’t consistently match symptom relief, limiting its surrogate value.
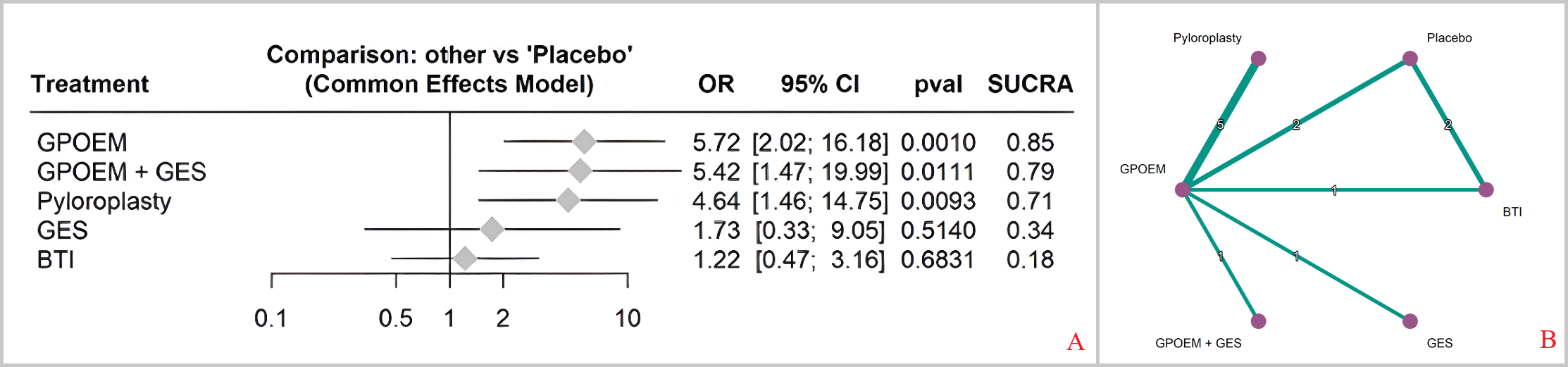
Figure: Figure (1): [A] Forest plot of clinical success (ORs vs Placebo) comparing interventions against placebo. GPOEM and GPOEM+GES were associated with the highest odds of clinical response.
[B] Network geometry of procedural interventions for gastroparesis with clinical success as the primary outcome
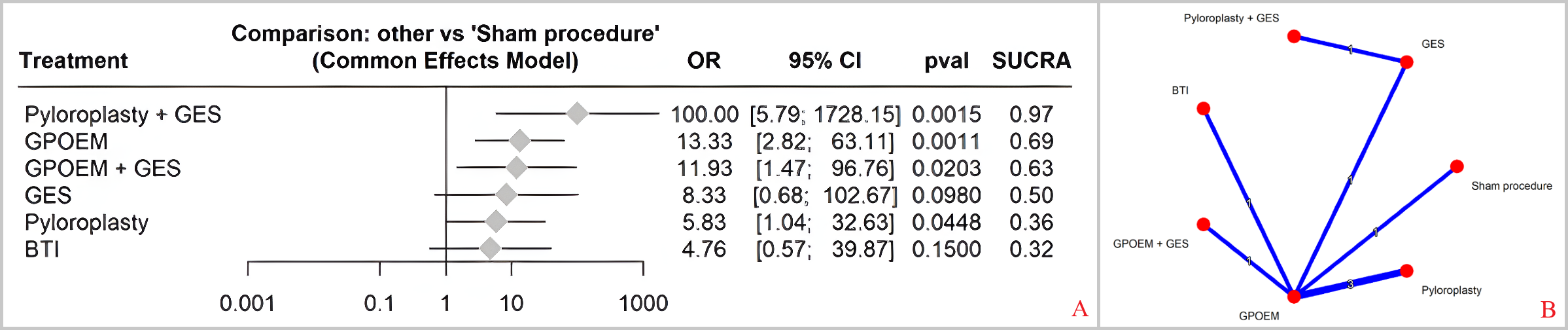
Figure: Figure (2): [A] Forest plot comparing improvement in gastric emptying among interventions relative to sham (ORs vs Sham). Pyloroplasty + GES and GPOEM demonstrated the greatest effect sizes.
[B] Network Plot: Gastric Emptying Improvement. Network plot of interventions evaluated for gastric emptying test (GET) improvement.
Disclosures:
Ismail Althunibat indicated no relevant financial relationships.
Yahya Alhalalmeh indicated no relevant financial relationships.
Thai Hau Koo indicated no relevant financial relationships.
Muhammad Elsharkawy indicated no relevant financial relationships.
Ahmad Alomari indicated no relevant financial relationships.
Murad Qirem indicated no relevant financial relationships.
Mohamed Eldesouki indicated no relevant financial relationships.
Theodore DaCosta, Jr. indicated no relevant financial relationships.
Yatinder Bains indicated no relevant financial relationships.
Brian Ginnebaugh: Ardelyx – Speakers Bureau.
Ala Abdel-Jalil indicated no relevant financial relationships.
Yaseen Alastal indicated no relevant financial relationships.
Ismail Althunibat, MD1, Yahya Alhalalmeh, MD1, Thai Hau Koo, MD2, Muhammad Elsharkawy, MD3, Ahmad Alomari, MD4, Murad Qirem, MD5, Mohamed Eldesouki, MD6, Theodore DaCosta, Jr., MD1, Yatinder Bains, MD1, Brian Ginnebaugh, MD4, Ala Abdel-Jalil, MD7, Yaseen Alastal, MD8. P4170 - Comparative Efficacy of Endoscopic and Surgical Interventions for Gastroparesis: A Systematic Review and Network Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
