Monday Poster Session
Category: Stomach and Spleen
P4169 - Comparative Efficacy of Pharmacologic Therapies for Gastroparesis: A Systematic Review and Network Meta-Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ismail Althunibat, MD
New York Medical College - Saint Michael's Medical Center
Newark, NJ
Presenting Author(s)
Award: ACG Presidential Poster Award
Ismail Althunibat, MD1, Thai Hau Koo, MD2, Muhammad Elsharkawy, MD3, Yahya Alhalalmeh, MD1, Murad Qirem, MD4, Ahmad Alomari, MD5, Mohamed Eldesouki, MD6, Byron Okwesili, MD1, Theodore DaCosta, Jr., MD1, Yatinder Bains, MD1, Ala Abdel-Jalil, MD7, Yaseen Alastal, MD8
1New York Medical College - Saint Michael's Medical Center, Newark, NJ; 2University of Sciences Malaysia Specialist Hospital, Kelantan, Kelantan, Malaysia; 3Alexandria University, Alexandria, Al Iskandariyah, Egypt; 4New York Medical College - Saint Michael's Medical Center, West Orange, NJ; 5Henry Ford Health, Detroit, MI; 6Saint Michael's Medical Center, New York Medical College, Newark, NJ; 7Case Western Reserve University / MetroHealth, Cleveland, OH; 8University of Toledo, Toledo, OH
Introduction: Gastroparesis is a chronic motility disorder with limited pharmacological options. Despite the availability of prokinetics, antiemetics, and investigational agents, clinical efficacy remains uncertain owing to limited head-to-head comparisons. We conducted a network meta-analysis to evaluate and rank the efficacy of pharmacological therapies for gastroparesis.
Methods: We systematically searched PubMed, Embase, and CENTRAL from January 1985 to present for randomized controlled trials evaluating adult patients with gastroparesis treated with pharmacologic agents. Interventions included prucalopride, cisapride, revexepride, metoclopramide, relamorelin, TZP-102, aprepitant, tradipitant, cannabidiol (CBD), and domperidone. The primary outcomes were symptomatic improvement, reported as standardized mean differences (SMDs) from validated symptom scores, and changes in gastric half-emptying time (t½). A Bayesian network meta-analysis was performed using a common effects model. Treatments were ranked by efficacy using the SUCRA values.
Results: A total of 21 trials comprising 2,452 patients were included in the study. For symptom improvement, 19 studies that compared 10 treatments contributed to the network. Cisapride (SMD, 1.88; 95% CI –2.71 to –1.06; SUCRA=0.98), relamorelin (SMD, 1.15; 95% CI –2.15 to –0.16; SUCRA=0.86), and aprepitant (SMD: 0.60; 95% CI –0.88 –0.32; SUCRA=0.76) significantly outperformed the placebo. TZP-102, prucalopride, and tradipitant showed modest benefits, whereas domperidone, metoclopramide, CBD, and revexepride had limited or non-significant effects. For gastric emptying improvement, 12 studies assessed 7 agents. Prucalopride demonstrated the most pronounced effect (MD –46.00 min; 95% CI –55.54 –36.46; SUCRA=0.98), followed by cisapride (MD –35.88 min; 95% CI –47.36 to –24.41; SUCRA=0.85) and relamorelin (MD –10.35 min; 95% CI –17.29 to –3.41; SUCRA=0.59). Other agents, including metoclopramide, revexepride, CBD, and TZP-102, showed no significant changes compared with placebo.
Discussion: Cisapride, relamorelin, and aprepitant demonstrated the highest efficacy for symptom relief, whereas prucalopride and cisapride were most effective in accelerating gastric emptying. The disconnection between symptomatic and motility-based outcomes highlights the need for individualized treatment selection and development of more robust surrogate endpoints in future gastroparesis trials.
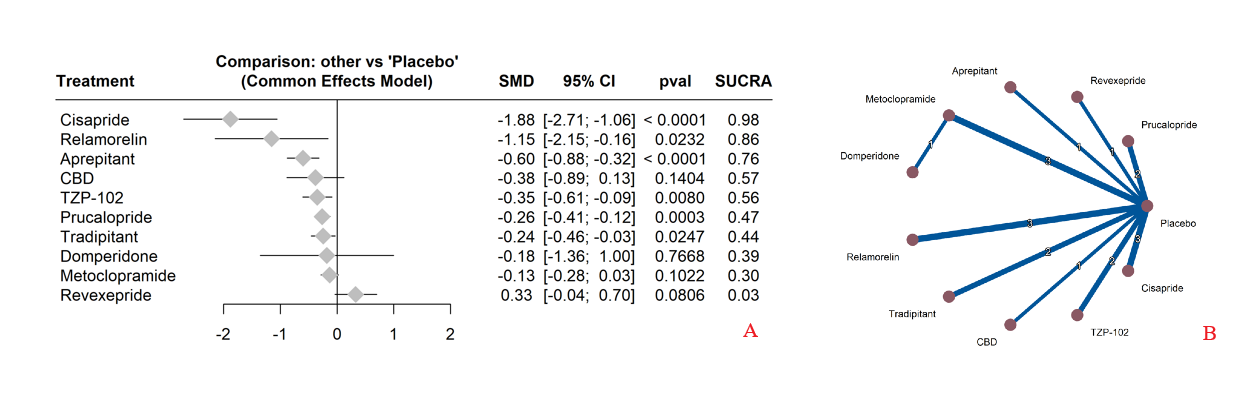
Figure: Figure (1): [A] Forest plot of pharmacologic agents vs placebo for symptom improvement in gastroparesis. Standardized mean differences (SMDs) with 95% CIs are shown. Cisapride (SMD –1.88), relamorelin (–1.15), and aprepitant (–0.60) showed significant benefit; TZP-102, prucalopride, and tradipitant showed modest effects, while others were non-significant.
[B] Network plot of pharmacologic therapies for symptom improvement in gastroparesis. Nodes represent treatments; edge thickness reflects the number of direct comparisons. Most studies compared active agents to placebo, with limited head-to-head trials.
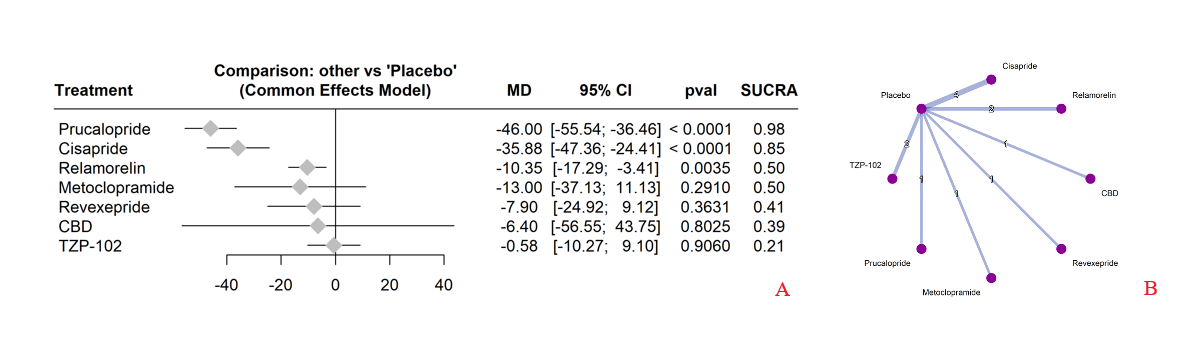
Figure: Figure (2): [A] Forest plot of pharmacologic agents vs placebo for gastric emptying (t½). Mean differences (MD) with 95% CIs are shown. Prucalopride (–46 min), cisapride (–36 min), and relamorelin (–10 min) significantly improved emptying; other agents showed non-significant effects.
[B] Network plot of pharmacologic treatments for gastric emptying improvement. Nodes represent treatments; edge thickness reflects number of studies. Most comparisons were vs placebo, with few head-to-head trials.
Disclosures:
Ismail Althunibat indicated no relevant financial relationships.
Thai Hau Koo indicated no relevant financial relationships.
Muhammad Elsharkawy indicated no relevant financial relationships.
Yahya Alhalalmeh indicated no relevant financial relationships.
Murad Qirem indicated no relevant financial relationships.
Ahmad Alomari indicated no relevant financial relationships.
Mohamed Eldesouki indicated no relevant financial relationships.
Byron Okwesili indicated no relevant financial relationships.
Theodore DaCosta, Jr. indicated no relevant financial relationships.
Yatinder Bains indicated no relevant financial relationships.
Ala Abdel-Jalil indicated no relevant financial relationships.
Yaseen Alastal indicated no relevant financial relationships.
Ismail Althunibat, MD1, Thai Hau Koo, MD2, Muhammad Elsharkawy, MD3, Yahya Alhalalmeh, MD1, Murad Qirem, MD4, Ahmad Alomari, MD5, Mohamed Eldesouki, MD6, Byron Okwesili, MD1, Theodore DaCosta, Jr., MD1, Yatinder Bains, MD1, Ala Abdel-Jalil, MD7, Yaseen Alastal, MD8. P4169 - Comparative Efficacy of Pharmacologic Therapies for Gastroparesis: A Systematic Review and Network Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Ismail Althunibat, MD1, Thai Hau Koo, MD2, Muhammad Elsharkawy, MD3, Yahya Alhalalmeh, MD1, Murad Qirem, MD4, Ahmad Alomari, MD5, Mohamed Eldesouki, MD6, Byron Okwesili, MD1, Theodore DaCosta, Jr., MD1, Yatinder Bains, MD1, Ala Abdel-Jalil, MD7, Yaseen Alastal, MD8
1New York Medical College - Saint Michael's Medical Center, Newark, NJ; 2University of Sciences Malaysia Specialist Hospital, Kelantan, Kelantan, Malaysia; 3Alexandria University, Alexandria, Al Iskandariyah, Egypt; 4New York Medical College - Saint Michael's Medical Center, West Orange, NJ; 5Henry Ford Health, Detroit, MI; 6Saint Michael's Medical Center, New York Medical College, Newark, NJ; 7Case Western Reserve University / MetroHealth, Cleveland, OH; 8University of Toledo, Toledo, OH
Introduction: Gastroparesis is a chronic motility disorder with limited pharmacological options. Despite the availability of prokinetics, antiemetics, and investigational agents, clinical efficacy remains uncertain owing to limited head-to-head comparisons. We conducted a network meta-analysis to evaluate and rank the efficacy of pharmacological therapies for gastroparesis.
Methods: We systematically searched PubMed, Embase, and CENTRAL from January 1985 to present for randomized controlled trials evaluating adult patients with gastroparesis treated with pharmacologic agents. Interventions included prucalopride, cisapride, revexepride, metoclopramide, relamorelin, TZP-102, aprepitant, tradipitant, cannabidiol (CBD), and domperidone. The primary outcomes were symptomatic improvement, reported as standardized mean differences (SMDs) from validated symptom scores, and changes in gastric half-emptying time (t½). A Bayesian network meta-analysis was performed using a common effects model. Treatments were ranked by efficacy using the SUCRA values.
Results: A total of 21 trials comprising 2,452 patients were included in the study. For symptom improvement, 19 studies that compared 10 treatments contributed to the network. Cisapride (SMD, 1.88; 95% CI –2.71 to –1.06; SUCRA=0.98), relamorelin (SMD, 1.15; 95% CI –2.15 to –0.16; SUCRA=0.86), and aprepitant (SMD: 0.60; 95% CI –0.88 –0.32; SUCRA=0.76) significantly outperformed the placebo. TZP-102, prucalopride, and tradipitant showed modest benefits, whereas domperidone, metoclopramide, CBD, and revexepride had limited or non-significant effects. For gastric emptying improvement, 12 studies assessed 7 agents. Prucalopride demonstrated the most pronounced effect (MD –46.00 min; 95% CI –55.54 –36.46; SUCRA=0.98), followed by cisapride (MD –35.88 min; 95% CI –47.36 to –24.41; SUCRA=0.85) and relamorelin (MD –10.35 min; 95% CI –17.29 to –3.41; SUCRA=0.59). Other agents, including metoclopramide, revexepride, CBD, and TZP-102, showed no significant changes compared with placebo.
Discussion: Cisapride, relamorelin, and aprepitant demonstrated the highest efficacy for symptom relief, whereas prucalopride and cisapride were most effective in accelerating gastric emptying. The disconnection between symptomatic and motility-based outcomes highlights the need for individualized treatment selection and development of more robust surrogate endpoints in future gastroparesis trials.
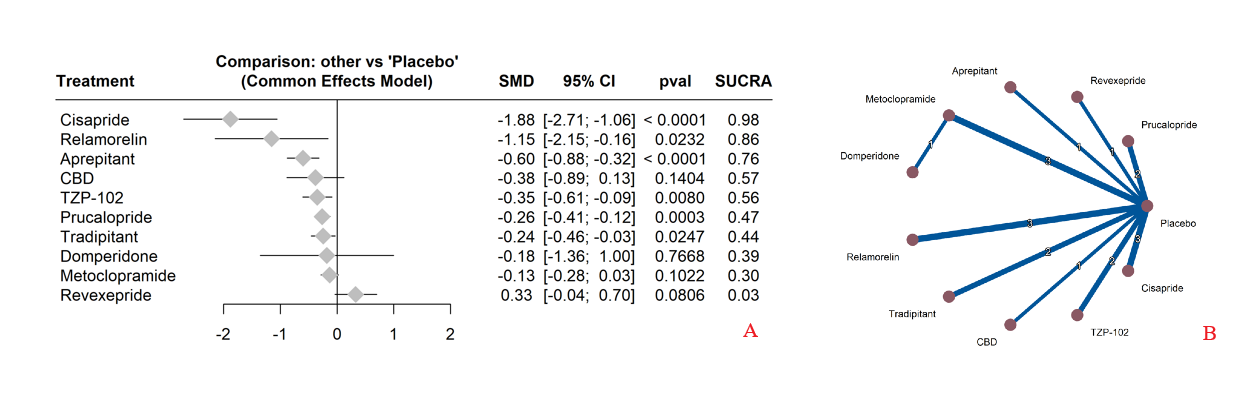
Figure: Figure (1): [A] Forest plot of pharmacologic agents vs placebo for symptom improvement in gastroparesis. Standardized mean differences (SMDs) with 95% CIs are shown. Cisapride (SMD –1.88), relamorelin (–1.15), and aprepitant (–0.60) showed significant benefit; TZP-102, prucalopride, and tradipitant showed modest effects, while others were non-significant.
[B] Network plot of pharmacologic therapies for symptom improvement in gastroparesis. Nodes represent treatments; edge thickness reflects the number of direct comparisons. Most studies compared active agents to placebo, with limited head-to-head trials.
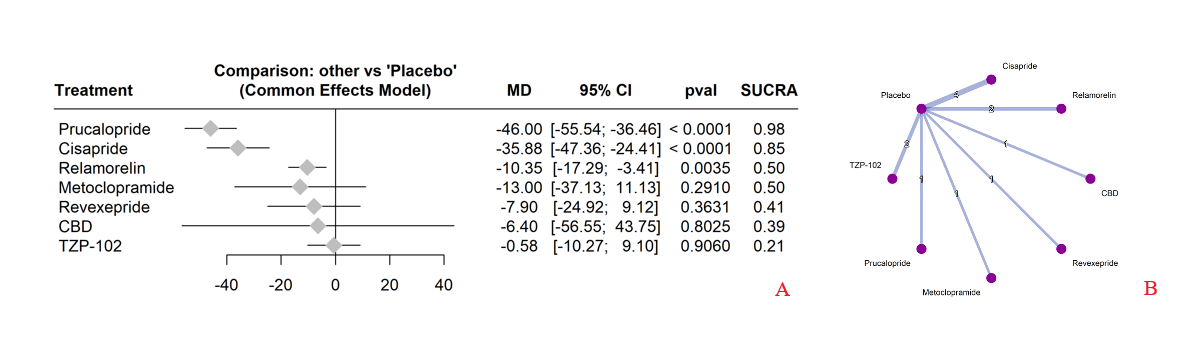
Figure: Figure (2): [A] Forest plot of pharmacologic agents vs placebo for gastric emptying (t½). Mean differences (MD) with 95% CIs are shown. Prucalopride (–46 min), cisapride (–36 min), and relamorelin (–10 min) significantly improved emptying; other agents showed non-significant effects.
[B] Network plot of pharmacologic treatments for gastric emptying improvement. Nodes represent treatments; edge thickness reflects number of studies. Most comparisons were vs placebo, with few head-to-head trials.
Disclosures:
Ismail Althunibat indicated no relevant financial relationships.
Thai Hau Koo indicated no relevant financial relationships.
Muhammad Elsharkawy indicated no relevant financial relationships.
Yahya Alhalalmeh indicated no relevant financial relationships.
Murad Qirem indicated no relevant financial relationships.
Ahmad Alomari indicated no relevant financial relationships.
Mohamed Eldesouki indicated no relevant financial relationships.
Byron Okwesili indicated no relevant financial relationships.
Theodore DaCosta, Jr. indicated no relevant financial relationships.
Yatinder Bains indicated no relevant financial relationships.
Ala Abdel-Jalil indicated no relevant financial relationships.
Yaseen Alastal indicated no relevant financial relationships.
Ismail Althunibat, MD1, Thai Hau Koo, MD2, Muhammad Elsharkawy, MD3, Yahya Alhalalmeh, MD1, Murad Qirem, MD4, Ahmad Alomari, MD5, Mohamed Eldesouki, MD6, Byron Okwesili, MD1, Theodore DaCosta, Jr., MD1, Yatinder Bains, MD1, Ala Abdel-Jalil, MD7, Yaseen Alastal, MD8. P4169 - Comparative Efficacy of Pharmacologic Therapies for Gastroparesis: A Systematic Review and Network Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

