Monday Poster Session
Category: Stomach and Spleen
P4238 - A Rare Outcome of Argon Plasma Coagulation (APC): Gastric Perforation
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Nisar Amin, MD
Charleston Area Medical Center
Charleston, WV
Presenting Author(s)
Nisar Amin, MD, Rama Nanah, MD, Harleen Chela, MD, Ebubekir Daglilar, MD
Charleston Area Medical Center, Charleston, WV
Introduction: Argon plasma coagulation (APC) is a minimally invasive endoscopic technique commonly used to manage gastrointestinal bleeding, ablate residual polypoid tissue, and treat gastric vascular ectasia. While generally safe, APC can occasionally result in serious complications. We present a rare case of gastric perforation following APC that necessitated extensive surgical intervention
Case Description/
Methods: A 74-year-old male nursing home resident with a history of hypertension, hyperlipidemia, hypothyroidism, dementia, and coronary artery disease presented with large-volume hemoptysis after weeks of mild bleeding. He was not on anticoagulation or NSAIDs aside from aspirin. On admission, he was hemodynamically stable, with benign abdominal findings. Labs showed hemoglobin 9 g/dL (dropping to 7.6), platelets 121 K/µL, BUN 60, and creatinine 2.9. CT abdomen unremarkable.
He was admitted to the ICU, developed acute hypoxic respiratory failure, and was intubated. Bronchoscopy revealed clots in the vocal cords, right main bronchus, and lower lobe without active bleeding. EGD showed diffuse hemorrhagic gastritis with friable mucosa, ulcerations, and angioectasias; hemostasis was achieved using argon plasma coagulation and hemostatic spray.
Within an hour, he developed abdominal rigidity and hypotension.Imaging showed pneumoperitoneum. His hemoglobin dropped to 5.5 g/dL, requiring transfusions. Emergent laparotomy revealed gastric perforation at the lesser curvature and a splenic laceration. He underwent gastric wedge resection, omental patch, and splenectomy. He received 9 units of pRBCs and 1 unit of FFP, with hemoglobin improving to 9.9 g/dL. Despite 10 days of antibiotics, he could not tolerate oral intake and required TPN. Renal function did not recover, likely due to acute tubular necrosis. He declined dialysis and feeding tube placement and was discharged home with hospice care per family decision
Discussion: APC is generally safe but can cause complications, including bleeding, ulceration, fistula, perforation, and rarely obstruction. A meta-analysis reported a 22.5% adverse event rate with APC in Barrett’s esophagus, including perforation. A study comparing 40 vs. 60 watts APC in the colon found no difference in perforation rates. Gastric perforation is rare due to the thick wall of the stomach, and incidence data are lacking. However, conditions like ischemic or atrophic gastritis that can compromise the integrity of the gastric wall may increase perforation risk, warranting caution with APC use
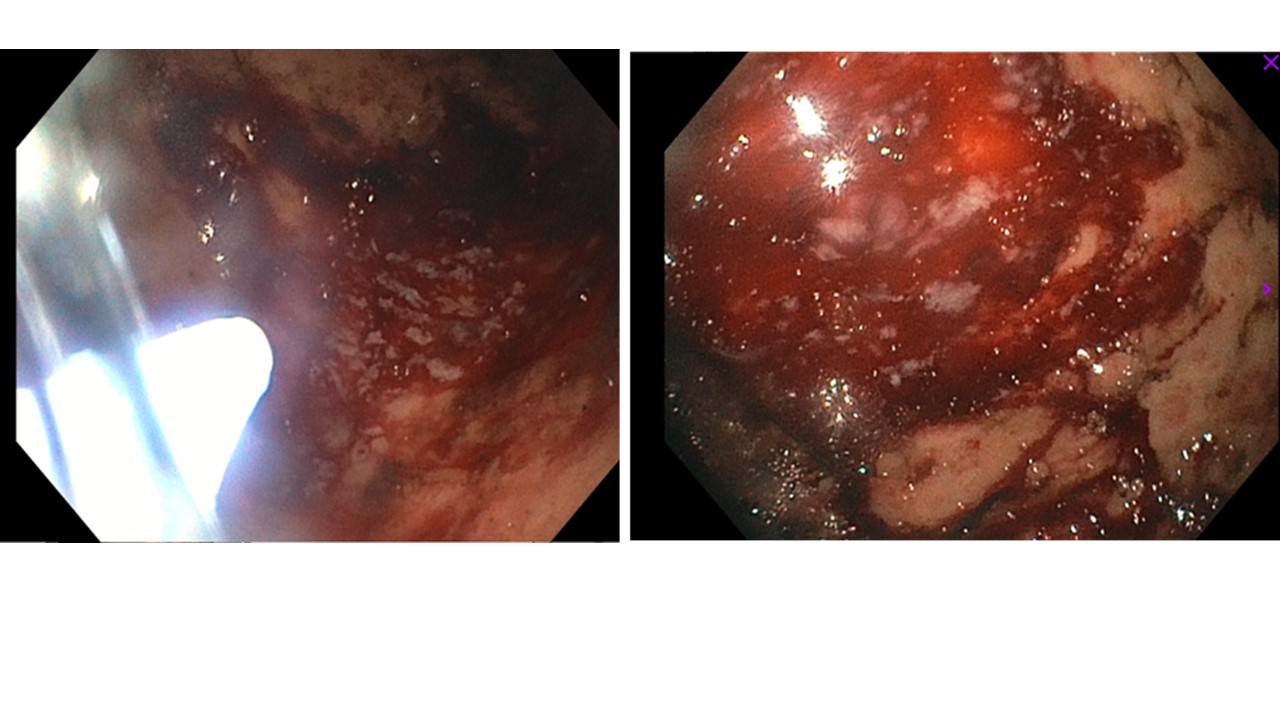
Figure: Figure-1. Diffuse hemorrhagic gastritis with friable mucosa, superficial ulcerations, and angioectasias in the fundus, body, and cardia seen on the EGD.
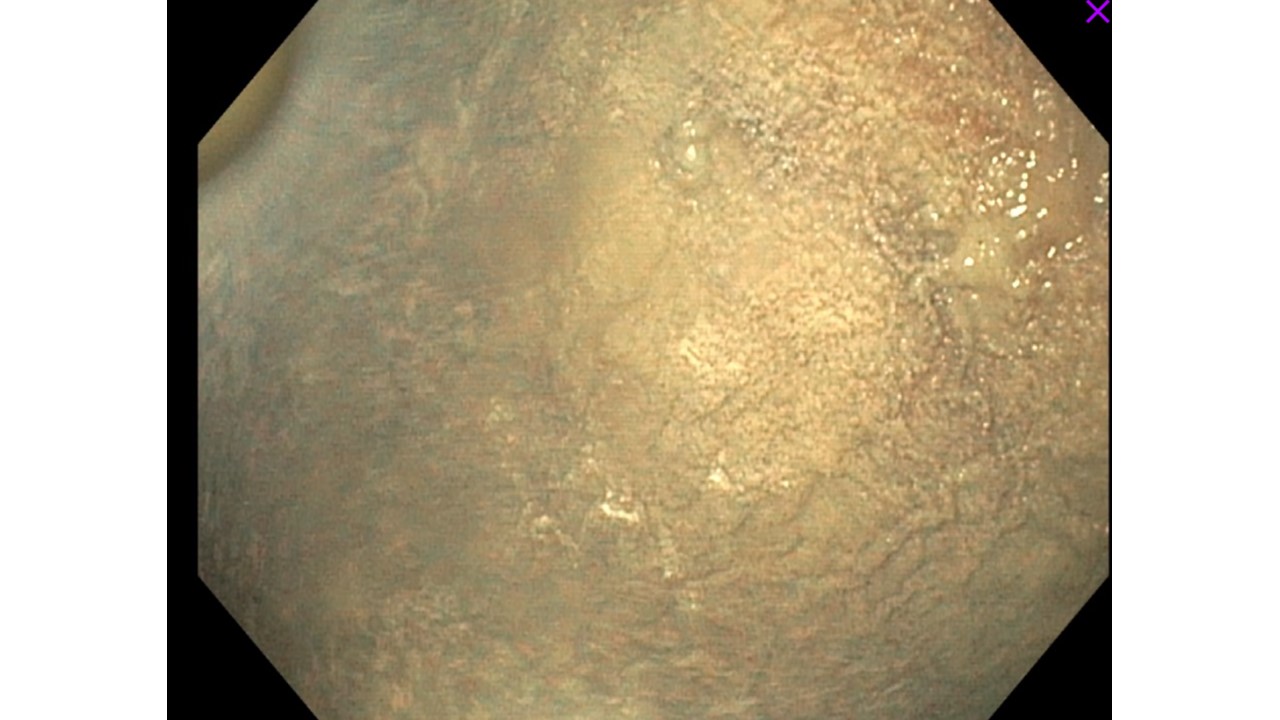
Figure: Figure-2. Gastric mucosa post treatment with hemostatic spray.
Disclosures:
Nisar Amin indicated no relevant financial relationships.
Rama Nanah indicated no relevant financial relationships.
Harleen Chela indicated no relevant financial relationships.
Ebubekir Daglilar indicated no relevant financial relationships.
Nisar Amin, MD, Rama Nanah, MD, Harleen Chela, MD, Ebubekir Daglilar, MD. P4238 - A Rare Outcome of Argon Plasma Coagulation (APC): Gastric Perforation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Charleston Area Medical Center, Charleston, WV
Introduction: Argon plasma coagulation (APC) is a minimally invasive endoscopic technique commonly used to manage gastrointestinal bleeding, ablate residual polypoid tissue, and treat gastric vascular ectasia. While generally safe, APC can occasionally result in serious complications. We present a rare case of gastric perforation following APC that necessitated extensive surgical intervention
Case Description/
Methods: A 74-year-old male nursing home resident with a history of hypertension, hyperlipidemia, hypothyroidism, dementia, and coronary artery disease presented with large-volume hemoptysis after weeks of mild bleeding. He was not on anticoagulation or NSAIDs aside from aspirin. On admission, he was hemodynamically stable, with benign abdominal findings. Labs showed hemoglobin 9 g/dL (dropping to 7.6), platelets 121 K/µL, BUN 60, and creatinine 2.9. CT abdomen unremarkable.
He was admitted to the ICU, developed acute hypoxic respiratory failure, and was intubated. Bronchoscopy revealed clots in the vocal cords, right main bronchus, and lower lobe without active bleeding. EGD showed diffuse hemorrhagic gastritis with friable mucosa, ulcerations, and angioectasias; hemostasis was achieved using argon plasma coagulation and hemostatic spray.
Within an hour, he developed abdominal rigidity and hypotension.Imaging showed pneumoperitoneum. His hemoglobin dropped to 5.5 g/dL, requiring transfusions. Emergent laparotomy revealed gastric perforation at the lesser curvature and a splenic laceration. He underwent gastric wedge resection, omental patch, and splenectomy. He received 9 units of pRBCs and 1 unit of FFP, with hemoglobin improving to 9.9 g/dL. Despite 10 days of antibiotics, he could not tolerate oral intake and required TPN. Renal function did not recover, likely due to acute tubular necrosis. He declined dialysis and feeding tube placement and was discharged home with hospice care per family decision
Discussion: APC is generally safe but can cause complications, including bleeding, ulceration, fistula, perforation, and rarely obstruction. A meta-analysis reported a 22.5% adverse event rate with APC in Barrett’s esophagus, including perforation. A study comparing 40 vs. 60 watts APC in the colon found no difference in perforation rates. Gastric perforation is rare due to the thick wall of the stomach, and incidence data are lacking. However, conditions like ischemic or atrophic gastritis that can compromise the integrity of the gastric wall may increase perforation risk, warranting caution with APC use
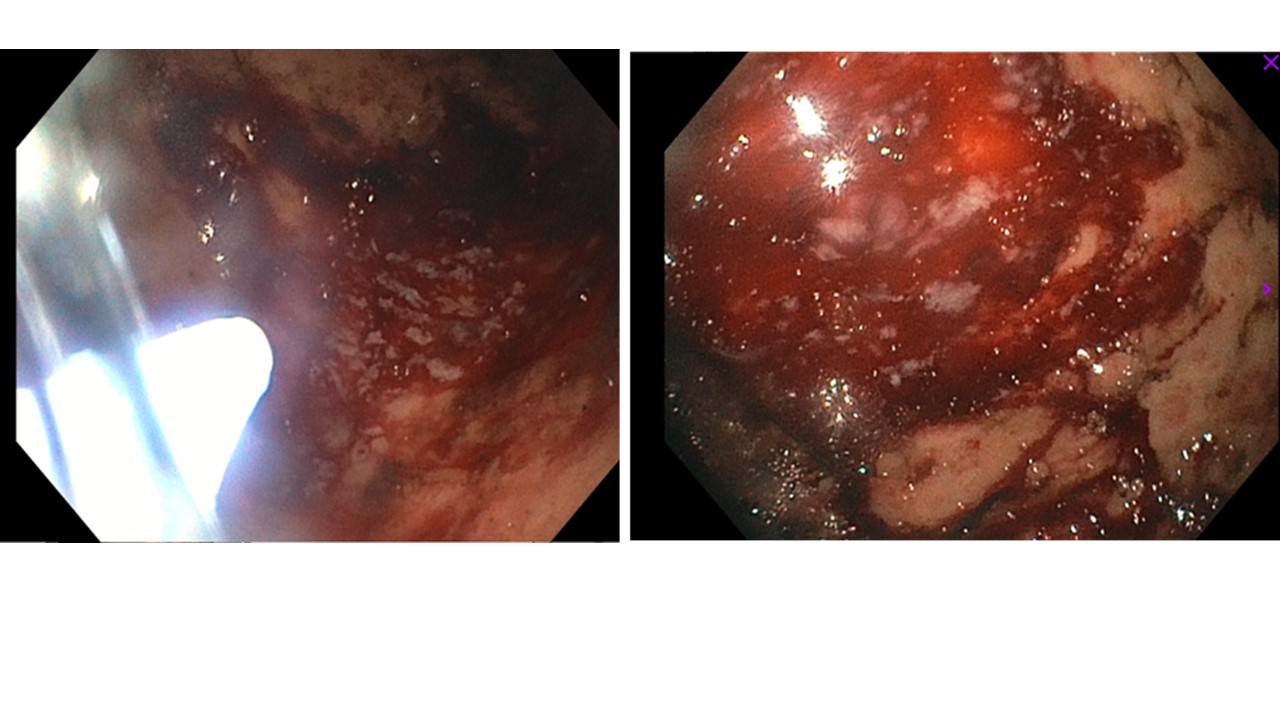
Figure: Figure-1. Diffuse hemorrhagic gastritis with friable mucosa, superficial ulcerations, and angioectasias in the fundus, body, and cardia seen on the EGD.
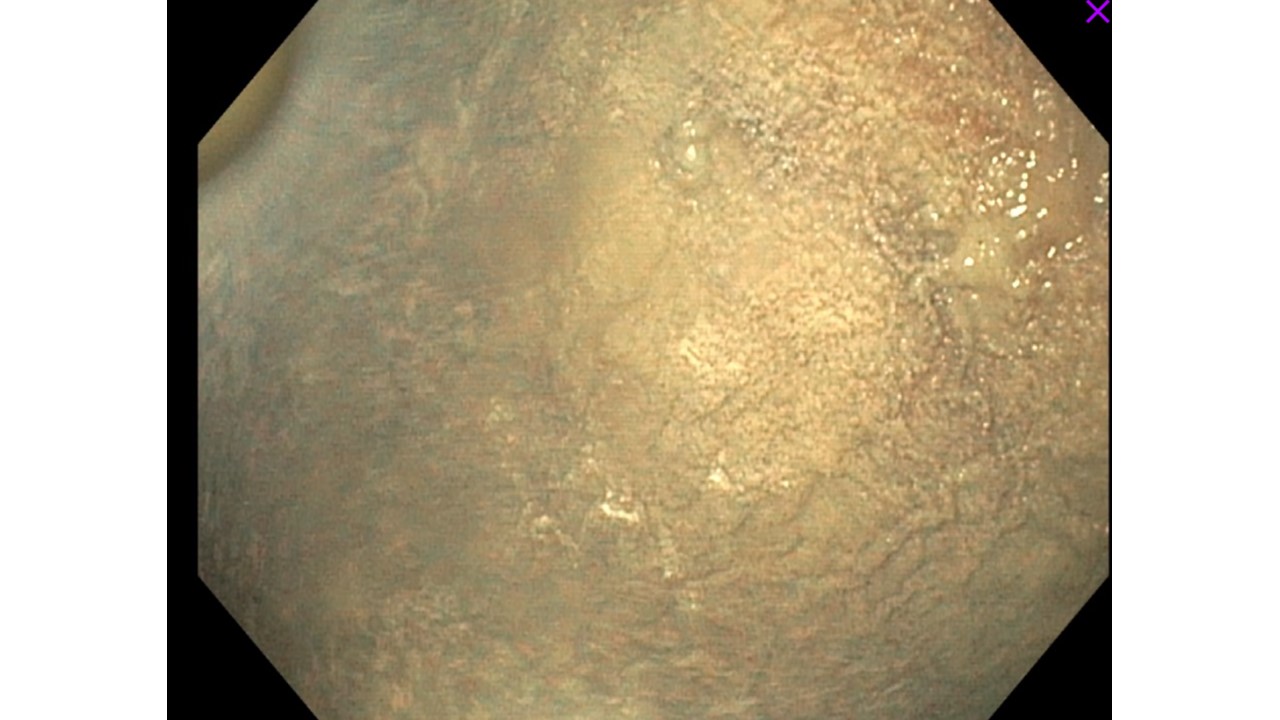
Figure: Figure-2. Gastric mucosa post treatment with hemostatic spray.
Disclosures:
Nisar Amin indicated no relevant financial relationships.
Rama Nanah indicated no relevant financial relationships.
Harleen Chela indicated no relevant financial relationships.
Ebubekir Daglilar indicated no relevant financial relationships.
Nisar Amin, MD, Rama Nanah, MD, Harleen Chela, MD, Ebubekir Daglilar, MD. P4238 - A Rare Outcome of Argon Plasma Coagulation (APC): Gastric Perforation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
