Monday Poster Session
Category: Stomach and Spleen
P4233 - A Case of Severe Ischemic Gastritis and Duodenitis: Endoscopic Guidance for the Safe Reintroduction of Enteral Nutrition
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mark Stasiewicz, MD
Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas
Las Vegas, NV
Presenting Author(s)
Mark Stasiewicz, MD1, Yassin Naga, MD1, Gordon v. Ohning, MD, PhD2, Jose Aponte-Pieras, MD1
1Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 2Kirk Kerkorian School of Medicine at UNLV, Las Vegas, NV
Introduction: Ischemic gastritis (IG) and ischemic duodenitis (ID) are rare due to the extensive anastomotic network supplying the stomach and duodenum, requiring profound splanchnic hypoperfusion to induce injury. In states of shock, gastric perfusion may decrease by up to 90%, resulting in mucosal breakdown, ulceration, bleeding, and necrosis. Prognosis is usually poor owing to the severity of underlying illness. Management is complicated by the need to carefully time enteral feeding after bowel rest, as both delayed enteral nutrition and prolonged parenteral nutrition carry risks. We present a case of severe IG/ID in a medically complex young patient, highlighting the role of surveillance endoscopy in guiding safe refeeding.
Case Description/
Methods: An 18-year-old nonverbal male with spastic quadriplegic cerebral palsy presented with hypotension, anemia and abdominal distension. Computed tomography (CT) revealed a markedly distended stomach, and suction of gastric contents per gastrostomy tube was concerning for acute GI bleeding. Esophagogastroduodenoscopy (EGD) on hospital day (HD) 1 revealed diffuse ulceration affecting 90% of the gastric mucosa and friable mucosa in the entire bulb and second portion of the duodenum; there was no sign of active bleeding. High-dose proton pump inhibitor therapy and strict bowel rest were instituted. Total parenteral nutrition (TPN) was initiated on HD 7. Trophic enteral feeds were attempted on HD 8, with the patient developing tachycardia and lactic acidosis, prompting ICU transfer for suspected mesenteric ischemia. After clinical stabilization and unremarkable CT angiography, EGD on HD 14 showed a marked decrease in mucosal damage. Trophic feeding was resumed and gradually advanced until TPN was discontinued on HD 18. The patient was discharged on HD 35, after further treatment for an unrelated pulmonary infection.
Discussion: This case underscores the diagnostic and therapeutic complexities of IG/ID, particularly in situations where history is limited. Early EGD allowed for prompt diagnosis and ruled out alternative causes of bleeding. Surveillance EGD provided visual confirmation of mucosal recovery, allowing for the safe reintroduction of enteral nutrition, reducing the risk of further ischemic insult. As data guiding nutrition in IG/ID are limited, this case offers a unique time-line based approach to refeeding following profound ischemic insults. Further studies are needed to inform evidence-based protocols for nutritional management in these patients.
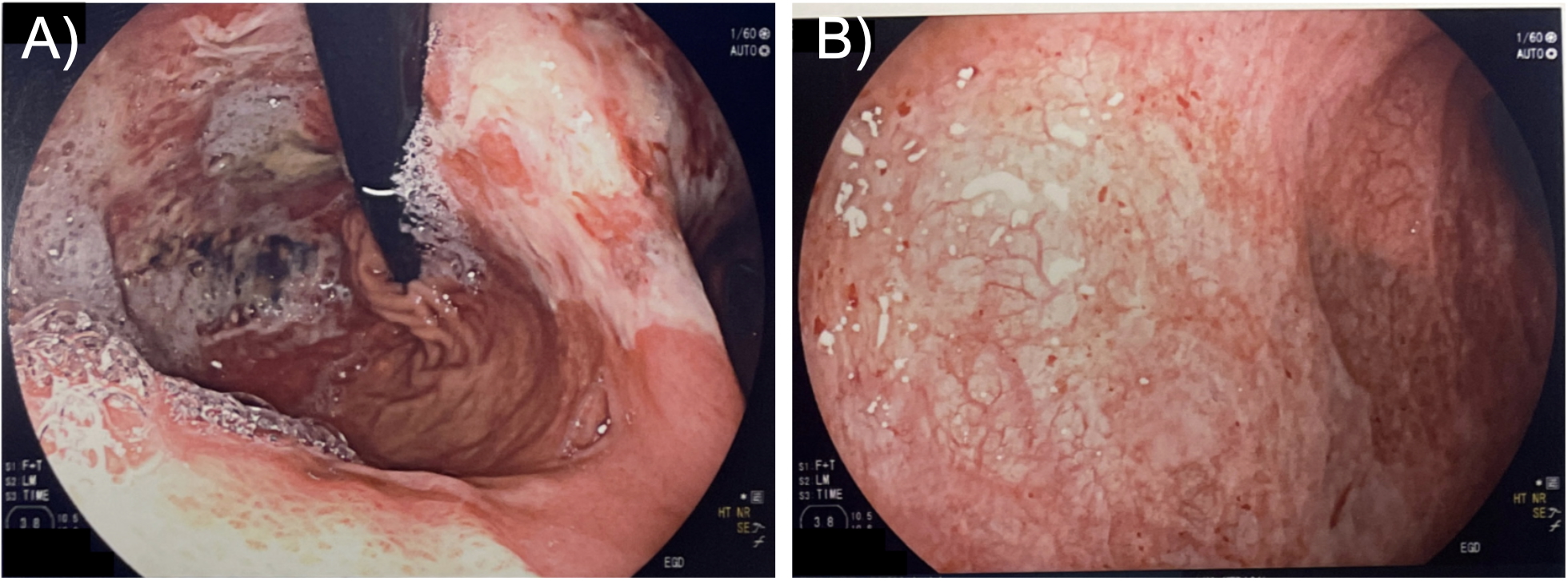
Figure: Figure 1. Images from EGD on hospital day 1. A) Normal mucosa surrounded by desquamating mucosal lining. B) Extensive heme deposition on gastric mucosa. C) Percutaneous endoscopic gastrostomy tube bumper without evidence of buried bumper syndrome or resulting ulceration. D) Mucosal desquamation and heme deposition in the duodenum.
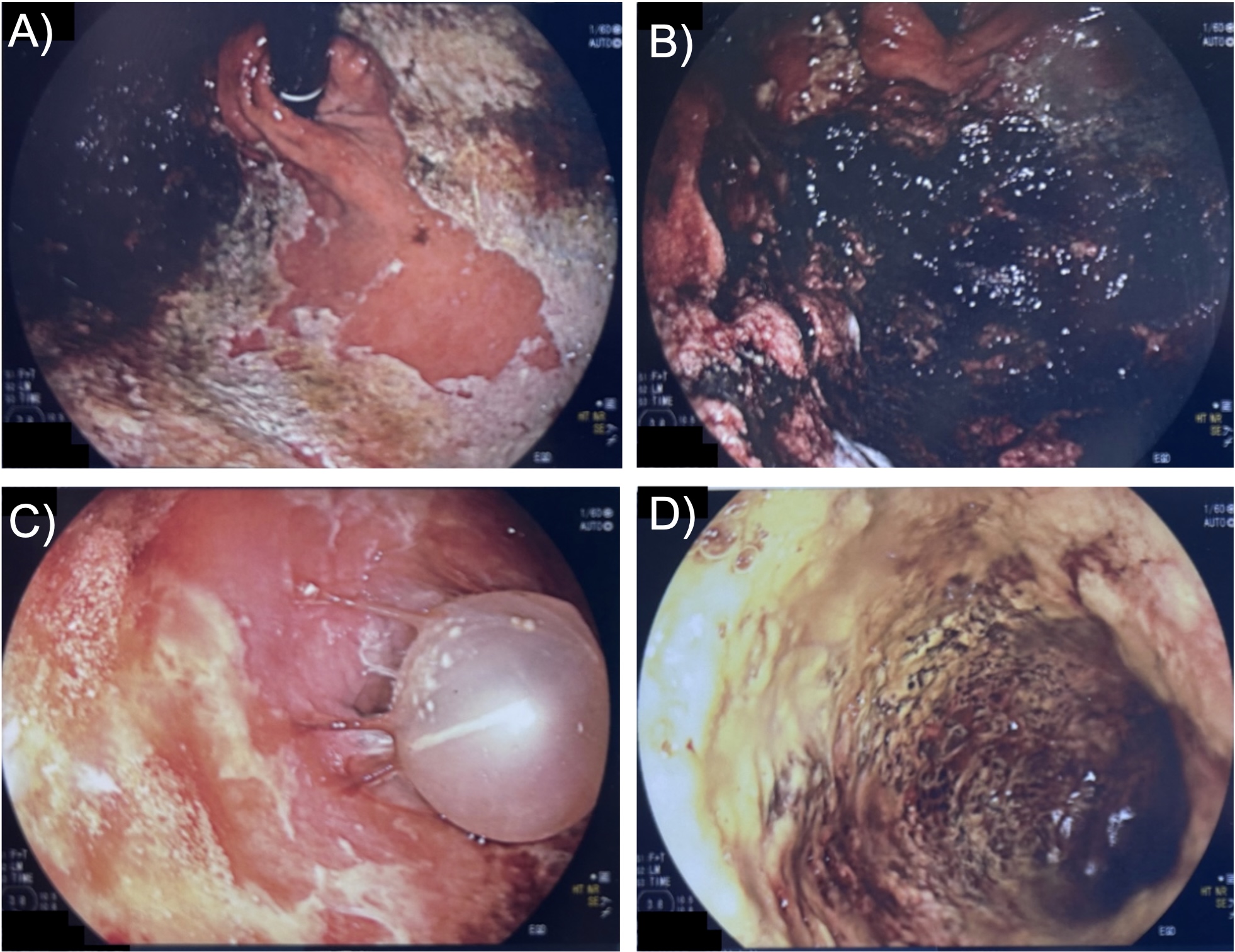
Figure: Figure 2. Images from EGD on hospital day 14. A) Superficial ulcers in gastric fundus. B) Normal mucosa within the duodenum.
Disclosures:
Mark Stasiewicz indicated no relevant financial relationships.
Yassin Naga indicated no relevant financial relationships.
Gordon Ohning indicated no relevant financial relationships.
Jose Aponte-Pieras indicated no relevant financial relationships.
Mark Stasiewicz, MD1, Yassin Naga, MD1, Gordon v. Ohning, MD, PhD2, Jose Aponte-Pieras, MD1. P4233 - A Case of Severe Ischemic Gastritis and Duodenitis: Endoscopic Guidance for the Safe Reintroduction of Enteral Nutrition, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 2Kirk Kerkorian School of Medicine at UNLV, Las Vegas, NV
Introduction: Ischemic gastritis (IG) and ischemic duodenitis (ID) are rare due to the extensive anastomotic network supplying the stomach and duodenum, requiring profound splanchnic hypoperfusion to induce injury. In states of shock, gastric perfusion may decrease by up to 90%, resulting in mucosal breakdown, ulceration, bleeding, and necrosis. Prognosis is usually poor owing to the severity of underlying illness. Management is complicated by the need to carefully time enteral feeding after bowel rest, as both delayed enteral nutrition and prolonged parenteral nutrition carry risks. We present a case of severe IG/ID in a medically complex young patient, highlighting the role of surveillance endoscopy in guiding safe refeeding.
Case Description/
Methods: An 18-year-old nonverbal male with spastic quadriplegic cerebral palsy presented with hypotension, anemia and abdominal distension. Computed tomography (CT) revealed a markedly distended stomach, and suction of gastric contents per gastrostomy tube was concerning for acute GI bleeding. Esophagogastroduodenoscopy (EGD) on hospital day (HD) 1 revealed diffuse ulceration affecting 90% of the gastric mucosa and friable mucosa in the entire bulb and second portion of the duodenum; there was no sign of active bleeding. High-dose proton pump inhibitor therapy and strict bowel rest were instituted. Total parenteral nutrition (TPN) was initiated on HD 7. Trophic enteral feeds were attempted on HD 8, with the patient developing tachycardia and lactic acidosis, prompting ICU transfer for suspected mesenteric ischemia. After clinical stabilization and unremarkable CT angiography, EGD on HD 14 showed a marked decrease in mucosal damage. Trophic feeding was resumed and gradually advanced until TPN was discontinued on HD 18. The patient was discharged on HD 35, after further treatment for an unrelated pulmonary infection.
Discussion: This case underscores the diagnostic and therapeutic complexities of IG/ID, particularly in situations where history is limited. Early EGD allowed for prompt diagnosis and ruled out alternative causes of bleeding. Surveillance EGD provided visual confirmation of mucosal recovery, allowing for the safe reintroduction of enteral nutrition, reducing the risk of further ischemic insult. As data guiding nutrition in IG/ID are limited, this case offers a unique time-line based approach to refeeding following profound ischemic insults. Further studies are needed to inform evidence-based protocols for nutritional management in these patients.
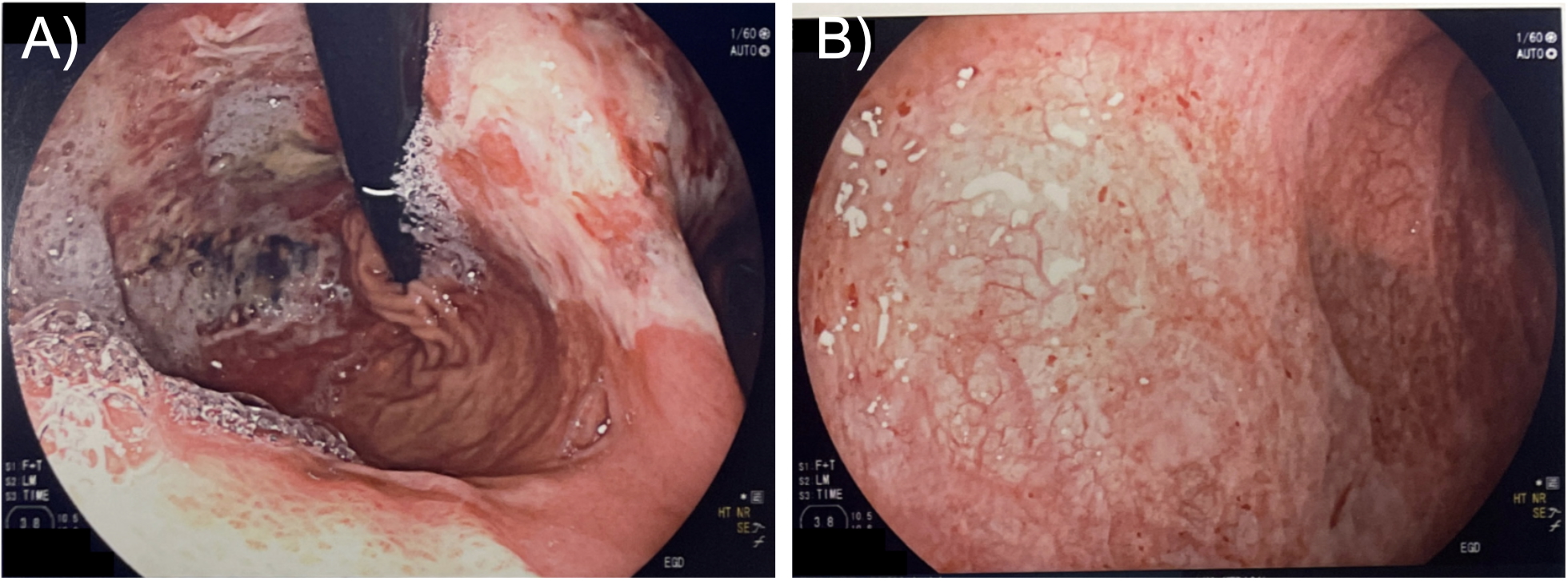
Figure: Figure 1. Images from EGD on hospital day 1. A) Normal mucosa surrounded by desquamating mucosal lining. B) Extensive heme deposition on gastric mucosa. C) Percutaneous endoscopic gastrostomy tube bumper without evidence of buried bumper syndrome or resulting ulceration. D) Mucosal desquamation and heme deposition in the duodenum.
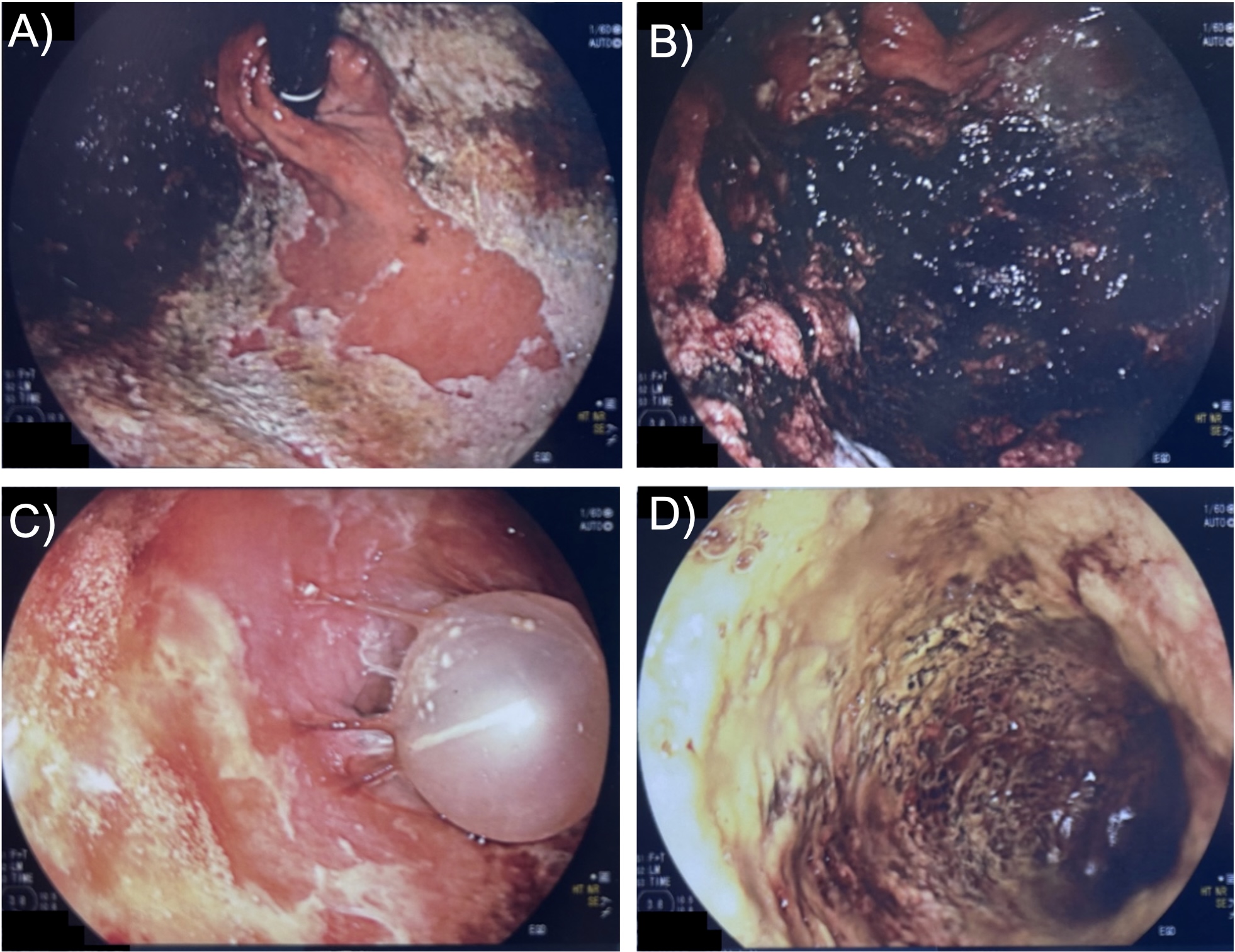
Figure: Figure 2. Images from EGD on hospital day 14. A) Superficial ulcers in gastric fundus. B) Normal mucosa within the duodenum.
Disclosures:
Mark Stasiewicz indicated no relevant financial relationships.
Yassin Naga indicated no relevant financial relationships.
Gordon Ohning indicated no relevant financial relationships.
Jose Aponte-Pieras indicated no relevant financial relationships.
Mark Stasiewicz, MD1, Yassin Naga, MD1, Gordon v. Ohning, MD, PhD2, Jose Aponte-Pieras, MD1. P4233 - A Case of Severe Ischemic Gastritis and Duodenitis: Endoscopic Guidance for the Safe Reintroduction of Enteral Nutrition, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

