Monday Poster Session
Category: Stomach and Spleen
P4230 - AFP-Negative Gastroesophageal Yolk Sac Tumor: An Atypical Extragonadal Presentation
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Kavya Sudireddy, MD
UMass Chan Medical School
Worcester, MA
Presenting Author(s)
Kavya Sudireddy, MD, Kathryn Addonizio, MD, Brian Midkiff, MD, MPH, Salwa Khedr, MD, MSc, William White, MD
UMass Chan Medical School, Worcester, MA
Introduction: Yolk sac tumors (YST) are aggressive malignant germ cell tumors with a bimodal age distribution, commonly occurring in early childhood or post-pubertal adulthood. Extragonadal occurrences are rare, comprising of 5.7% cases in males and typically involve the mediastinum, nervous system, and retroperitoneum. We present an atypical case of a primary extragonadal yolk sac tumor (EGYST) arising at the gastroesophageal (GE) junction.
Case Description/
Methods: A 32-year-old male with a past medical history of GERD presented to the primary care clinic with one month of epigastric abdominal pain, progressive dysphagia, and a ten-pound weight loss. Physical exam revealed a tender, mildly distended abdomen with a palpable epigastric mass.
An expedited outpatient esophagogastroduodenoscopy showed a large circumferential ulcerating mass in the lower third of the esophagus and a smaller noncircumferential ulcerating mass in the gastric cardia. Biopsy revealed YST, with immunohistochemistry positive for SALL4, AE1/AE3, Glypican-3, and CDX2, but negative for alpha-fetoprotein (AFP) staining. Serum AFP levels and beta-human chorionic gonadotropin were normal. Laboratory testing revealed transaminitis and elevated lactate dehydrogenase of 661U/L. Scrotal ultrasound was unremarkable. Staging scans confirmed a gastro-esophageal junction mass with liver invasion, thereby confirming the diagnosis of primary EGYST of the GE junction.
The patient was admitted for symptom management and initiated on chemotherapy with etoposide, ifosfamide, and cisplatin (VIP). Definitive resection was not pursued in discussion with surgical consulting services. Following Cycle 3 of chemotherapy, PET/CT showed a reduction in the size of the mass from 20 cm to 15 cm without significant FDG-avid disease, improvement in liver enzymes, and marked symptomatic improvement.
Discussion: EGYST primaries of the GE junction without adenomatous elements are exceedingly rare, with only a handful of cases reported in literature. Early diagnosis and treatment are crucial but challenging due to their atypical location and tendency to be mistaken for adenocarcinoma, gastrointestinal stromal tumor, or lymphoma.
While an elevated AFP level is a key diagnostic marker, in rare instances, tumors may demonstrate negative AFP staining on pathology and negative serum AFP. This case emphasizes the importance of consideration of EGYST in the differential diagnosis of upper GE junction tumors in young patients and the role of timely pathological confirmation.
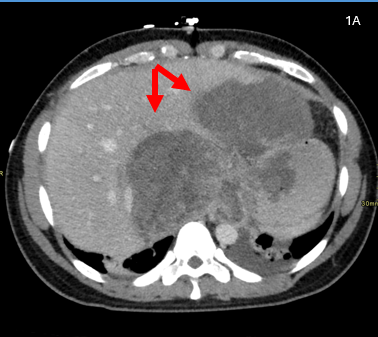
Figure: Axial contrast-enhanced CT image shows large, hypoenhancing regions of tumor extending into both the left and right hepatic lobes, as well as involving the stomach and gastroesophageal junction. Extension into the lower mediastinum was also present, as well as a small left pleural effusion.

Figure: Coronal reconstruction from a contrast-enhanced CT shows a large, 20+ cm mass centered near the upper abdominal midline involving multiple structures, including both the stomach and liver. Disease is also seen involving the distal esophagus and lower mediastinum.
Disclosures:
Kavya Sudireddy indicated no relevant financial relationships.
Kathryn Addonizio indicated no relevant financial relationships.
Brian Midkiff indicated no relevant financial relationships.
Salwa Khedr indicated no relevant financial relationships.
William White indicated no relevant financial relationships.
Kavya Sudireddy, MD, Kathryn Addonizio, MD, Brian Midkiff, MD, MPH, Salwa Khedr, MD, MSc, William White, MD. P4230 - AFP-Negative Gastroesophageal Yolk Sac Tumor: An Atypical Extragonadal Presentation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
UMass Chan Medical School, Worcester, MA
Introduction: Yolk sac tumors (YST) are aggressive malignant germ cell tumors with a bimodal age distribution, commonly occurring in early childhood or post-pubertal adulthood. Extragonadal occurrences are rare, comprising of 5.7% cases in males and typically involve the mediastinum, nervous system, and retroperitoneum. We present an atypical case of a primary extragonadal yolk sac tumor (EGYST) arising at the gastroesophageal (GE) junction.
Case Description/
Methods: A 32-year-old male with a past medical history of GERD presented to the primary care clinic with one month of epigastric abdominal pain, progressive dysphagia, and a ten-pound weight loss. Physical exam revealed a tender, mildly distended abdomen with a palpable epigastric mass.
An expedited outpatient esophagogastroduodenoscopy showed a large circumferential ulcerating mass in the lower third of the esophagus and a smaller noncircumferential ulcerating mass in the gastric cardia. Biopsy revealed YST, with immunohistochemistry positive for SALL4, AE1/AE3, Glypican-3, and CDX2, but negative for alpha-fetoprotein (AFP) staining. Serum AFP levels and beta-human chorionic gonadotropin were normal. Laboratory testing revealed transaminitis and elevated lactate dehydrogenase of 661U/L. Scrotal ultrasound was unremarkable. Staging scans confirmed a gastro-esophageal junction mass with liver invasion, thereby confirming the diagnosis of primary EGYST of the GE junction.
The patient was admitted for symptom management and initiated on chemotherapy with etoposide, ifosfamide, and cisplatin (VIP). Definitive resection was not pursued in discussion with surgical consulting services. Following Cycle 3 of chemotherapy, PET/CT showed a reduction in the size of the mass from 20 cm to 15 cm without significant FDG-avid disease, improvement in liver enzymes, and marked symptomatic improvement.
Discussion: EGYST primaries of the GE junction without adenomatous elements are exceedingly rare, with only a handful of cases reported in literature. Early diagnosis and treatment are crucial but challenging due to their atypical location and tendency to be mistaken for adenocarcinoma, gastrointestinal stromal tumor, or lymphoma.
While an elevated AFP level is a key diagnostic marker, in rare instances, tumors may demonstrate negative AFP staining on pathology and negative serum AFP. This case emphasizes the importance of consideration of EGYST in the differential diagnosis of upper GE junction tumors in young patients and the role of timely pathological confirmation.
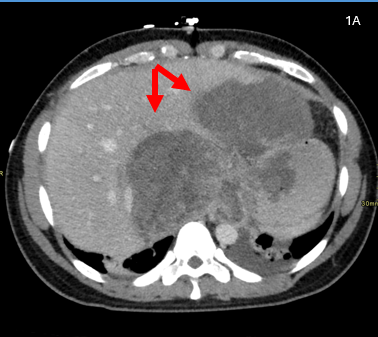
Figure: Axial contrast-enhanced CT image shows large, hypoenhancing regions of tumor extending into both the left and right hepatic lobes, as well as involving the stomach and gastroesophageal junction. Extension into the lower mediastinum was also present, as well as a small left pleural effusion.

Figure: Coronal reconstruction from a contrast-enhanced CT shows a large, 20+ cm mass centered near the upper abdominal midline involving multiple structures, including both the stomach and liver. Disease is also seen involving the distal esophagus and lower mediastinum.
Disclosures:
Kavya Sudireddy indicated no relevant financial relationships.
Kathryn Addonizio indicated no relevant financial relationships.
Brian Midkiff indicated no relevant financial relationships.
Salwa Khedr indicated no relevant financial relationships.
William White indicated no relevant financial relationships.
Kavya Sudireddy, MD, Kathryn Addonizio, MD, Brian Midkiff, MD, MPH, Salwa Khedr, MD, MSc, William White, MD. P4230 - AFP-Negative Gastroesophageal Yolk Sac Tumor: An Atypical Extragonadal Presentation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
