Monday Poster Session
Category: Stomach and Spleen
P4271 - A Case of Juvenile Polyposis Syndrome Diagnosed by Genetic Testing Despite Hyperplastic Polyps and No Active Bleeding
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- VG
Virali Gulla, MD
Texas Tech University Health Sciences Center, El Paso, Texas
El Paso, TX
Presenting Author(s)
Virali Gulla, MD1, Shivangini Duggal, MD2, Swati Mahapatra, DO3, Akanksha Togra, MD4, Jesus Guzman, MD5, Alejandro Robles, MD6
1Texas Tech University Health Sciences Center, El Paso, Texas, El Paso, TX; 2Department of Internal Medicine at Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso TX, USA, El Paso, TX; 3Texas A&M, El Paso, TX; 4Texas Tech University Health Sciences Center, El Paso, El Paso, TX; 5Division of Gastroenterology, Department of Internal Medicine, Texas Tech University Health Sciences Center, El Paso, TX., El Paso, TX; 6Department of Gastroenterology, Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center El Paso, El Paso , TX, El Paso, TX
Introduction: Juvenile polyposis syndrome (JPS) is an autosomal dominant disorder characterized by multiple hamartomatous polyps throughout the gastrointestinal tract, associated with an increased risk of colorectal and gastric malignancies. SMAD4 mutations are frequently implicated, often presenting with severe GI bleeding, anemia, and hypoproteinemia. However, atypical presentations without overt bleeding may delay diagnosis. We present a case of JPS confirmed by genetic testing despite non-specific endoscopic and histologic findings.
Case Description/
Methods: A 36-year-old male with a year-long history of microcytic anemia presented with worsening fatigue, chest pain, frequent epistaxis, dizziness, and palpitations. Examination revealed pallor and dried nasal blood without active bleeding. Laboratory workup showed severe iron deficiency anemia (Hb 7.4 g/dL). He subsequently developed NSTEMI, requiring anticoagulation, which was complicated by GI bleeding. Endoscopic evaluation revealed multiple gastric, pyloric, duodenal, cecal, and colonic polyps, including a large duodenal lesion. Biopsies from multiple sites demonstrated hyperplastic polyps without dysplasia. Despite the inconclusive histology, genetic testing identified a pathogenic SMAD4 mutation, confirming JPS. Colorectal surgery planned a colectomy for the patient due to high polyp burden.
Discussion: Diagnosis of JPS requires either multiple juvenile polyps in the GI tract or a pathogenic SMAD4/BMPR1A mutation, with 25% of cases occurring sporadically. This case underscores the importance of genetic testing, particularly when endoscopic and histologic findings are ambiguous and may mimic serrated polyposis syndrome (SPS). Unlike SPS, JPS surveillance begins earlier and includes cardiac screening due to associated hereditary hemorrhagic telangiectasia. Our patient’s iron deficiency anemia occurred without active GI bleeding, further complicating management due to iron intolerance. This case highlights the need for clear genotype-guided management strategies in JPS, including timing of surgical versus endoscopic interventions.
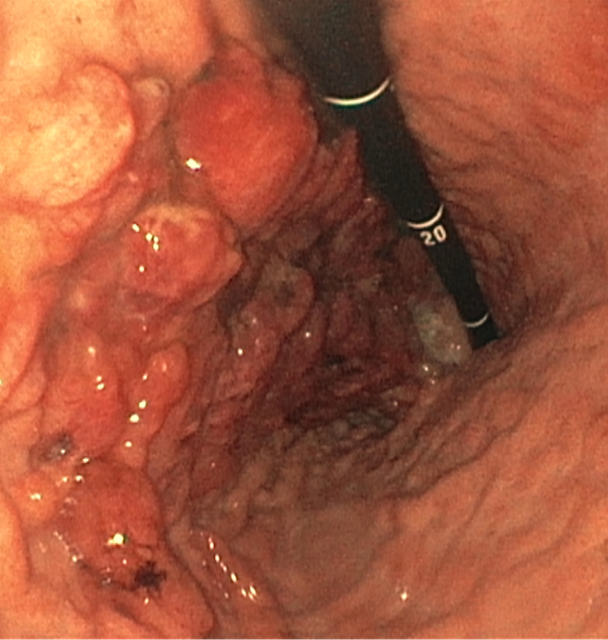
Figure: EGD with multiple gastric polyps
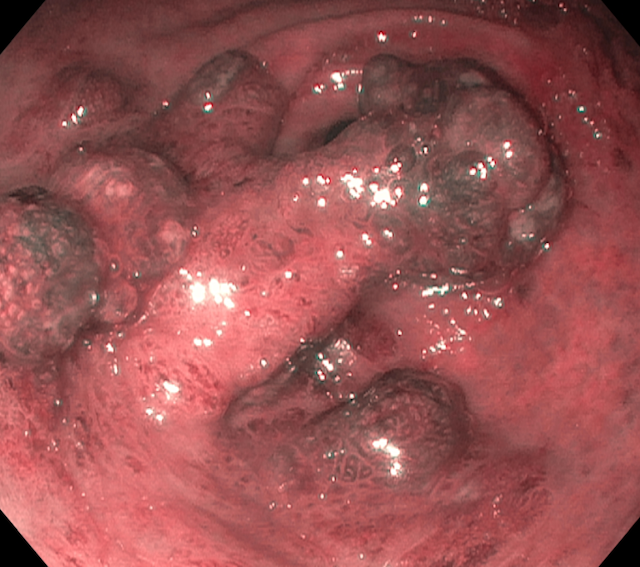
Figure: Hyperplastic polyps seen on Endoscopy
Disclosures:
Virali Gulla indicated no relevant financial relationships.
Shivangini Duggal indicated no relevant financial relationships.
Swati Mahapatra indicated no relevant financial relationships.
Akanksha Togra indicated no relevant financial relationships.
Jesus Guzman indicated no relevant financial relationships.
Alejandro Robles indicated no relevant financial relationships.
Virali Gulla, MD1, Shivangini Duggal, MD2, Swati Mahapatra, DO3, Akanksha Togra, MD4, Jesus Guzman, MD5, Alejandro Robles, MD6. P4271 - A Case of Juvenile Polyposis Syndrome Diagnosed by Genetic Testing Despite Hyperplastic Polyps and No Active Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Texas Tech University Health Sciences Center, El Paso, Texas, El Paso, TX; 2Department of Internal Medicine at Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso TX, USA, El Paso, TX; 3Texas A&M, El Paso, TX; 4Texas Tech University Health Sciences Center, El Paso, El Paso, TX; 5Division of Gastroenterology, Department of Internal Medicine, Texas Tech University Health Sciences Center, El Paso, TX., El Paso, TX; 6Department of Gastroenterology, Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center El Paso, El Paso , TX, El Paso, TX
Introduction: Juvenile polyposis syndrome (JPS) is an autosomal dominant disorder characterized by multiple hamartomatous polyps throughout the gastrointestinal tract, associated with an increased risk of colorectal and gastric malignancies. SMAD4 mutations are frequently implicated, often presenting with severe GI bleeding, anemia, and hypoproteinemia. However, atypical presentations without overt bleeding may delay diagnosis. We present a case of JPS confirmed by genetic testing despite non-specific endoscopic and histologic findings.
Case Description/
Methods: A 36-year-old male with a year-long history of microcytic anemia presented with worsening fatigue, chest pain, frequent epistaxis, dizziness, and palpitations. Examination revealed pallor and dried nasal blood without active bleeding. Laboratory workup showed severe iron deficiency anemia (Hb 7.4 g/dL). He subsequently developed NSTEMI, requiring anticoagulation, which was complicated by GI bleeding. Endoscopic evaluation revealed multiple gastric, pyloric, duodenal, cecal, and colonic polyps, including a large duodenal lesion. Biopsies from multiple sites demonstrated hyperplastic polyps without dysplasia. Despite the inconclusive histology, genetic testing identified a pathogenic SMAD4 mutation, confirming JPS. Colorectal surgery planned a colectomy for the patient due to high polyp burden.
Discussion: Diagnosis of JPS requires either multiple juvenile polyps in the GI tract or a pathogenic SMAD4/BMPR1A mutation, with 25% of cases occurring sporadically. This case underscores the importance of genetic testing, particularly when endoscopic and histologic findings are ambiguous and may mimic serrated polyposis syndrome (SPS). Unlike SPS, JPS surveillance begins earlier and includes cardiac screening due to associated hereditary hemorrhagic telangiectasia. Our patient’s iron deficiency anemia occurred without active GI bleeding, further complicating management due to iron intolerance. This case highlights the need for clear genotype-guided management strategies in JPS, including timing of surgical versus endoscopic interventions.
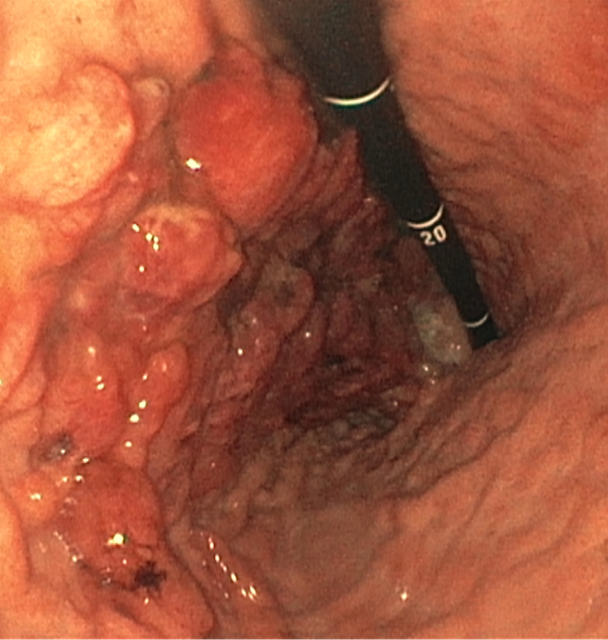
Figure: EGD with multiple gastric polyps
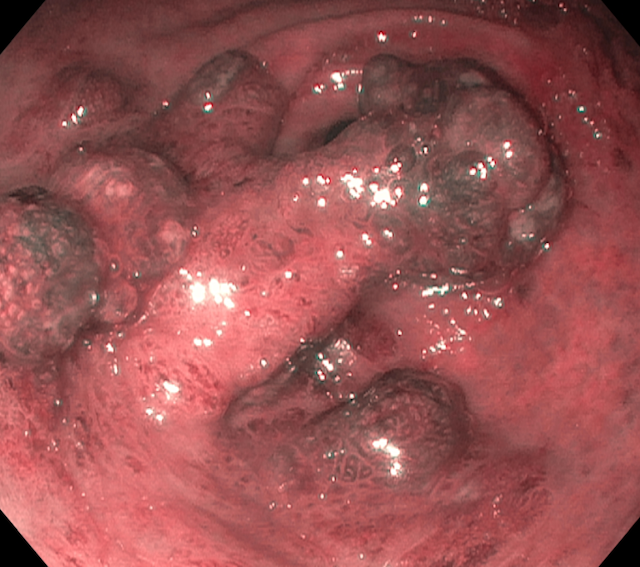
Figure: Hyperplastic polyps seen on Endoscopy
Disclosures:
Virali Gulla indicated no relevant financial relationships.
Shivangini Duggal indicated no relevant financial relationships.
Swati Mahapatra indicated no relevant financial relationships.
Akanksha Togra indicated no relevant financial relationships.
Jesus Guzman indicated no relevant financial relationships.
Alejandro Robles indicated no relevant financial relationships.
Virali Gulla, MD1, Shivangini Duggal, MD2, Swati Mahapatra, DO3, Akanksha Togra, MD4, Jesus Guzman, MD5, Alejandro Robles, MD6. P4271 - A Case of Juvenile Polyposis Syndrome Diagnosed by Genetic Testing Despite Hyperplastic Polyps and No Active Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
