Monday Poster Session
Category: Stomach and Spleen
P4259 - Encapsulated Splenic Hemorrhage in Chronic Pancreatitis: A Rare Sequela of Endogenous Zymogen Release
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Nadine Abul-Khoudoud, DO (she/her/hers)
HCA Florida Healthcare
New Port Richey, FL
Presenting Author(s)
Nadine Abul-Khoudoud, DO1, Nosakhare Idemudia, MD2, Faraz Eshaghi, DO2, Alexander Davis, DO2, Dilip Ghanekar, MD2
1HCA Florida Healthcare, New Port Richey, FL; 2HCA Florida Healthcare, Hudson, FL
Introduction: Chronic pancreatitis (CP) is a progressive inflammatory disorder characterized by irreversible destruction of pancreatic tissue. Splenic hemorrhage is a rare complication of pancreatitis, typically resulting from direct enzymatic digestion of the splenic parenchyma by activated pancreatic enzymes. Pseudocysts near the pancreatic tail may erode into the splenic capsule or vessels, leading to either acute rupture or encapsulated hemorrhage.
Case Description/
Methods: A 54-year-old male with alcohol use and CP of three years presented to the hospital with tachycardia, epigastric and left upper quadrant pain, abdominal distension, and a serum lipase of >600 U/L. A computed tomography (CT) scan with contrast of the abdomen and pelvis showed a complex subacute splenic subcapsular hematoma and a large pancreatic pseudocyst, see Figure 1. The patient was treated with intravenous fluids and pain control. The next day, the patient’s hemoglobin decreased from 14.5g/dL to 7.4 g/dL and he reported worsening abdominal pain and distention. Repeat CT imaging showed new hemoperitoneum and the spleen had increased in size, which was concerning for active hemorrhage or rupture. He was transfused two units of packed red blood cells and underwent splenic angiography that identified active extravasation, which was managed with embolization of the splenic artery. The patient was transferred for advanced endoscopic ultrasound (EUS) and esophagogastroduodenoscopy (EGD) that identified a large pancreatic pseudocyst with hematin debris. An AXIOS stent was placed to facilitate drainage, see Figure 2. Repeat endoscopy after stent removal showed collapse of the pseudocyst and a persistent large splenic hematoma.
Discussion: In this case, the development of a splenic hemorrhage was likely due to the extravasation of activated zymogens into adjacent tissues. The AXIOS stent system is an advanced endoscopic technique that uses a cautery-enhanced delivery catheter and lumen-apposing metal stent to facilitate direct, internal drainage between the gastrointestinal lumen and the target collection under EUS. Once the fluid collection is accessed, the stent deploys in a saddle shape to secure both walls and allow drainage. In cases of walled-off necrosis or infected pseudocysts, AXIOS allows for immediate decompression and provides a conduit for direct endoscopic necrosectomy if needed. This case demonstrates the necessity of early recognition of vascular complications, advanced imaging, and interventional techniques.
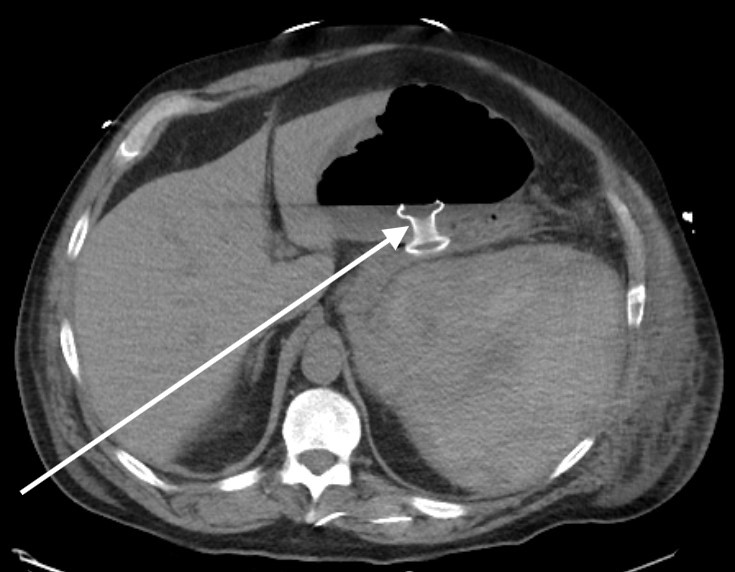
Figure: Figure 1. CT of the abdomen and pelvis with contrast. There is a white arrow to the large pancreatic pseudocyst. There is a red arrow to the 13 x 9 x 14 cm subcapsular splenic collection with compressive mass effect upon the enhancing splenic parenchyma.
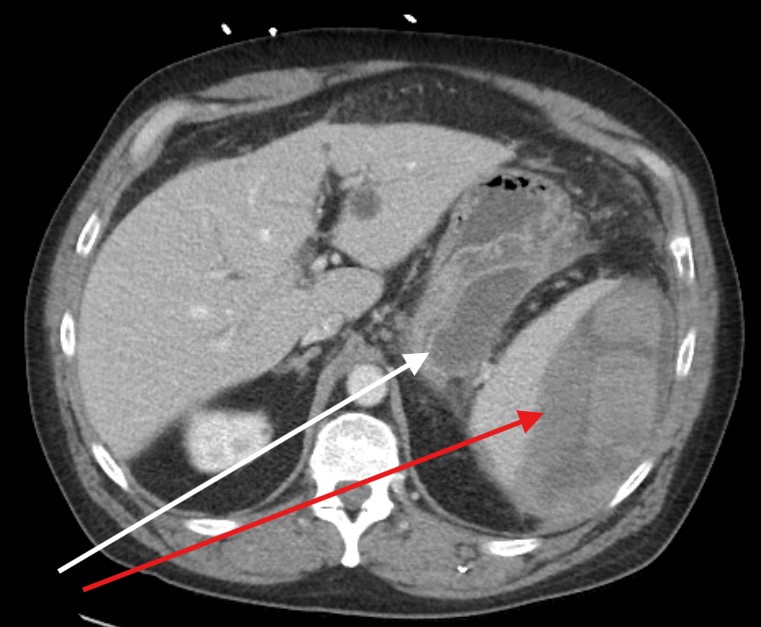
Figure: Figure 2. CT of the abdomen and pelvis with a white arrow to the Axios lumen apposing metal stent between the stomach and the pancreatic pseudocyst.
Disclosures:
Nadine Abul-Khoudoud indicated no relevant financial relationships.
Nosakhare Idemudia indicated no relevant financial relationships.
Faraz Eshaghi indicated no relevant financial relationships.
Alexander Davis indicated no relevant financial relationships.
Dilip Ghanekar indicated no relevant financial relationships.
Nadine Abul-Khoudoud, DO1, Nosakhare Idemudia, MD2, Faraz Eshaghi, DO2, Alexander Davis, DO2, Dilip Ghanekar, MD2. P4259 - Encapsulated Splenic Hemorrhage in Chronic Pancreatitis: A Rare Sequela of Endogenous Zymogen Release, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1HCA Florida Healthcare, New Port Richey, FL; 2HCA Florida Healthcare, Hudson, FL
Introduction: Chronic pancreatitis (CP) is a progressive inflammatory disorder characterized by irreversible destruction of pancreatic tissue. Splenic hemorrhage is a rare complication of pancreatitis, typically resulting from direct enzymatic digestion of the splenic parenchyma by activated pancreatic enzymes. Pseudocysts near the pancreatic tail may erode into the splenic capsule or vessels, leading to either acute rupture or encapsulated hemorrhage.
Case Description/
Methods: A 54-year-old male with alcohol use and CP of three years presented to the hospital with tachycardia, epigastric and left upper quadrant pain, abdominal distension, and a serum lipase of >600 U/L. A computed tomography (CT) scan with contrast of the abdomen and pelvis showed a complex subacute splenic subcapsular hematoma and a large pancreatic pseudocyst, see Figure 1. The patient was treated with intravenous fluids and pain control. The next day, the patient’s hemoglobin decreased from 14.5g/dL to 7.4 g/dL and he reported worsening abdominal pain and distention. Repeat CT imaging showed new hemoperitoneum and the spleen had increased in size, which was concerning for active hemorrhage or rupture. He was transfused two units of packed red blood cells and underwent splenic angiography that identified active extravasation, which was managed with embolization of the splenic artery. The patient was transferred for advanced endoscopic ultrasound (EUS) and esophagogastroduodenoscopy (EGD) that identified a large pancreatic pseudocyst with hematin debris. An AXIOS stent was placed to facilitate drainage, see Figure 2. Repeat endoscopy after stent removal showed collapse of the pseudocyst and a persistent large splenic hematoma.
Discussion: In this case, the development of a splenic hemorrhage was likely due to the extravasation of activated zymogens into adjacent tissues. The AXIOS stent system is an advanced endoscopic technique that uses a cautery-enhanced delivery catheter and lumen-apposing metal stent to facilitate direct, internal drainage between the gastrointestinal lumen and the target collection under EUS. Once the fluid collection is accessed, the stent deploys in a saddle shape to secure both walls and allow drainage. In cases of walled-off necrosis or infected pseudocysts, AXIOS allows for immediate decompression and provides a conduit for direct endoscopic necrosectomy if needed. This case demonstrates the necessity of early recognition of vascular complications, advanced imaging, and interventional techniques.
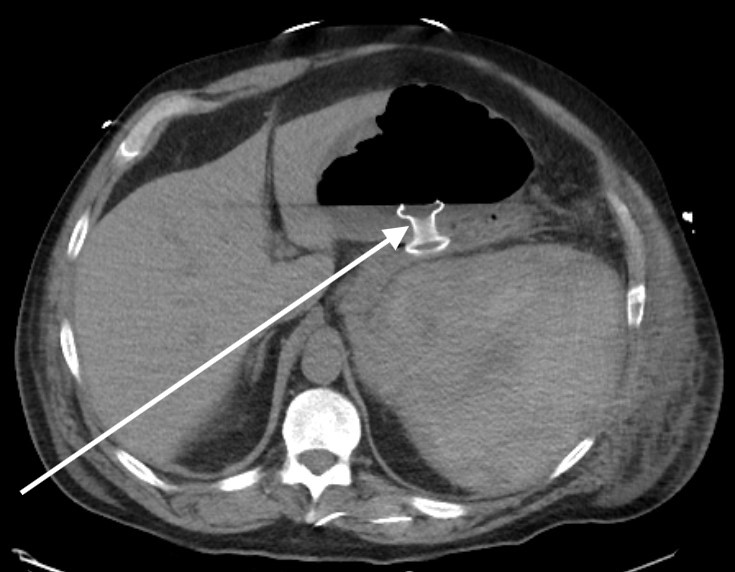
Figure: Figure 1. CT of the abdomen and pelvis with contrast. There is a white arrow to the large pancreatic pseudocyst. There is a red arrow to the 13 x 9 x 14 cm subcapsular splenic collection with compressive mass effect upon the enhancing splenic parenchyma.
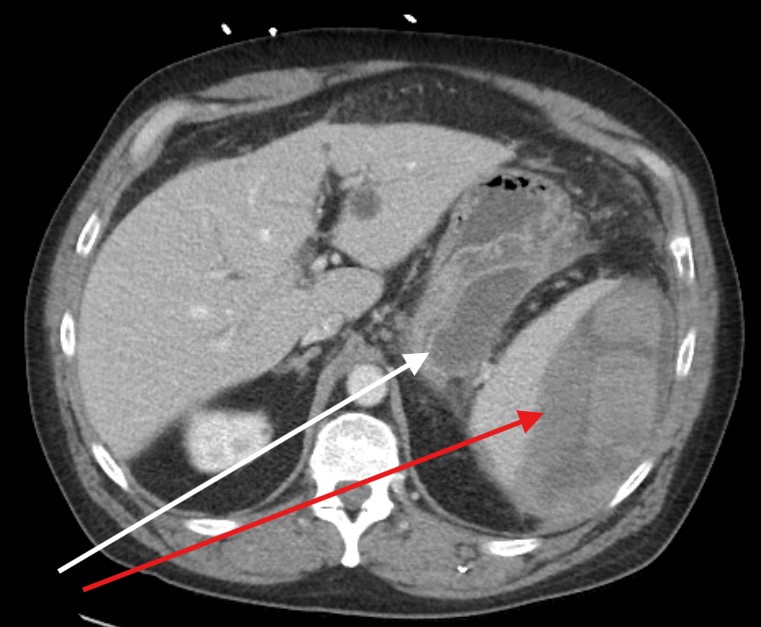
Figure: Figure 2. CT of the abdomen and pelvis with a white arrow to the Axios lumen apposing metal stent between the stomach and the pancreatic pseudocyst.
Disclosures:
Nadine Abul-Khoudoud indicated no relevant financial relationships.
Nosakhare Idemudia indicated no relevant financial relationships.
Faraz Eshaghi indicated no relevant financial relationships.
Alexander Davis indicated no relevant financial relationships.
Dilip Ghanekar indicated no relevant financial relationships.
Nadine Abul-Khoudoud, DO1, Nosakhare Idemudia, MD2, Faraz Eshaghi, DO2, Alexander Davis, DO2, Dilip Ghanekar, MD2. P4259 - Encapsulated Splenic Hemorrhage in Chronic Pancreatitis: A Rare Sequela of Endogenous Zymogen Release, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
