Monday Poster Session
Category: Stomach and Spleen
P4257 - Dubious Danger – A Case Report of Gastric DLBCL Hiding in Plain Sight
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Porsha Okiye, MD
Medical College of Georgia at Augusta University
Augusta, GA
Presenting Author(s)
Hrithik Dakssesh Putta Nagarajan, MBBS1, Amit Hudgi, MD2, Viveksandeep Thoguluva Chandrasekar, MBBS1, Brandol Wolfenbarger, MD1, Mei Zheng, MD, PhD1, Porsha Okiye, MD1
1Medical College of Georgia at Augusta University, Augusta, GA; 2Augusta University, Augusta, GA
Introduction: Diffuse large B-cell lymphoma (DLBCL) is a notably aggressive subtype lymphoma, often exhibiting extra-nodal involvement of the gastrointestinal tract. The stomach, small intestine, and ileocecal region are the most frequently affected sites. We present a case of a patient with stage III high-grade follicular lymphoma, subsequently transformed to refractory DLBCL with complications arising from splenic metastasis.
Case Description/
Methods:
A 78-year-old woman with PMHx significant for stage III high-grade follicular lymphoma, received six cycles of bendamustine and rituximab and mini-R-CHOP regimen presented with new-onset dysphagia and significant weight loss over 3 months. Two months prior, the patient presented with left upper quadrant pain, and splenomegaly was observed on imaging. PET scan at that time demonstrated increased uptake in an 8 × 8 cm splenic lesion (Standardized Uptake Value [SUV] 19) however, there was no uptake elsewhere. The pain was attributed to splenomegaly, and a splenectomy was planned and a exploratory laparotomy was performed. However, the procedure was aborted due to significant disease progression. The stomach cardia and fundus were densely adherent to the diaphragm, liver, and other underlying structures.
EGD done later showed patchy white plaques in the esophagus, consistent with Candida. A large, ulcerated mass devoid of bleeding was seen in the gastric fundus (Fig 1). Biopsies were obtained which confirmed DLBCL (Fig 2). A repeat CT scan done a month later, now revealed the lesion in the stomach. The patient was initiated on salvage chemotherapy. Upon follow-up, the patient reported improvement in her dysphagia, appetite and abdominal pain.
Discussion: An intriguing aspect of this case is the absence of the gastric involvement on prior imaging despite ongoing symptoms of weight loss and abdominal pain initially attributed to splenomegaly. Unfortunately, gastric invasion was not suspected until laparotomy was performed. Follicular lymphoma can transform to DLBCL, characterized by its highly aggressive nature and typically exhibits a high SUV on PET scans. However, cases of DLBCL that are "invisible" on PET-CT, indicated by a low SUV, have also been reported . Currently, there is no surveillance guidelines for evaluating GI involvement in patients with DLBCL. This case highlights the utility of EGD in patients with upper GI symptoms and not responding to treatment, potentially avoiding more invasive procedures.
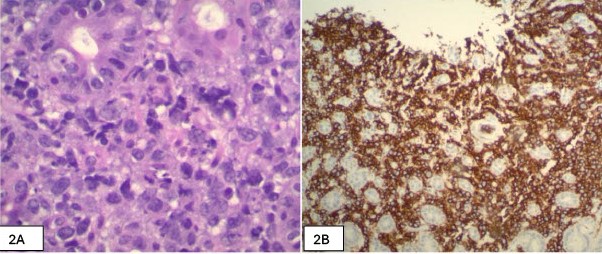
Figure: Figure 1: EGD image showing a large, ulcerated mass in the gastric fundus
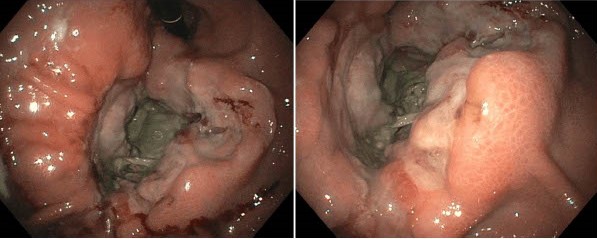
Figure: Figure 2A: H&E-stained section shows a sheet of medium to large atypical lymphoid cells infiltrating the glandular structure. Columnar-lined gastric glands are visible at the periphery of the infiltrate, highlighting the gastric mucosa amidst extensive involvement by the lymphoma.
Figure 2B: View of CD20 immunohistochemical staining, a B-cell lineage marker. The stain highlights strong membranous positivity in the intermediate to large atypical lymphoid cells, confirming their B-cell origin.
Disclosures:
Hrithik Dakssesh Putta Nagarajan indicated no relevant financial relationships.
Amit Hudgi indicated no relevant financial relationships.
Viveksandeep Thoguluva Chandrasekar indicated no relevant financial relationships.
Brandol Wolfenbarger indicated no relevant financial relationships.
Mei Zheng indicated no relevant financial relationships.
Porsha Okiye indicated no relevant financial relationships.
Hrithik Dakssesh Putta Nagarajan, MBBS1, Amit Hudgi, MD2, Viveksandeep Thoguluva Chandrasekar, MBBS1, Brandol Wolfenbarger, MD1, Mei Zheng, MD, PhD1, Porsha Okiye, MD1. P4257 - Dubious Danger – A Case Report of Gastric DLBCL Hiding in Plain Sight, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Medical College of Georgia at Augusta University, Augusta, GA; 2Augusta University, Augusta, GA
Introduction: Diffuse large B-cell lymphoma (DLBCL) is a notably aggressive subtype lymphoma, often exhibiting extra-nodal involvement of the gastrointestinal tract. The stomach, small intestine, and ileocecal region are the most frequently affected sites. We present a case of a patient with stage III high-grade follicular lymphoma, subsequently transformed to refractory DLBCL with complications arising from splenic metastasis.
Case Description/
Methods:
A 78-year-old woman with PMHx significant for stage III high-grade follicular lymphoma, received six cycles of bendamustine and rituximab and mini-R-CHOP regimen presented with new-onset dysphagia and significant weight loss over 3 months. Two months prior, the patient presented with left upper quadrant pain, and splenomegaly was observed on imaging. PET scan at that time demonstrated increased uptake in an 8 × 8 cm splenic lesion (Standardized Uptake Value [SUV] 19) however, there was no uptake elsewhere. The pain was attributed to splenomegaly, and a splenectomy was planned and a exploratory laparotomy was performed. However, the procedure was aborted due to significant disease progression. The stomach cardia and fundus were densely adherent to the diaphragm, liver, and other underlying structures.
EGD done later showed patchy white plaques in the esophagus, consistent with Candida. A large, ulcerated mass devoid of bleeding was seen in the gastric fundus (Fig 1). Biopsies were obtained which confirmed DLBCL (Fig 2). A repeat CT scan done a month later, now revealed the lesion in the stomach. The patient was initiated on salvage chemotherapy. Upon follow-up, the patient reported improvement in her dysphagia, appetite and abdominal pain.
Discussion: An intriguing aspect of this case is the absence of the gastric involvement on prior imaging despite ongoing symptoms of weight loss and abdominal pain initially attributed to splenomegaly. Unfortunately, gastric invasion was not suspected until laparotomy was performed. Follicular lymphoma can transform to DLBCL, characterized by its highly aggressive nature and typically exhibits a high SUV on PET scans. However, cases of DLBCL that are "invisible" on PET-CT, indicated by a low SUV, have also been reported . Currently, there is no surveillance guidelines for evaluating GI involvement in patients with DLBCL. This case highlights the utility of EGD in patients with upper GI symptoms and not responding to treatment, potentially avoiding more invasive procedures.
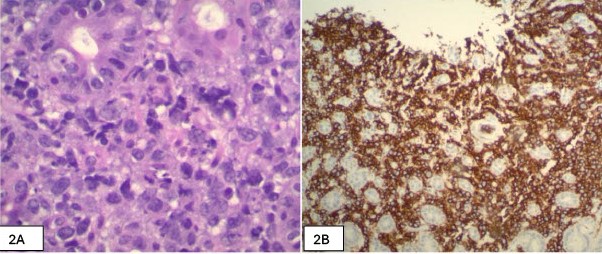
Figure: Figure 1: EGD image showing a large, ulcerated mass in the gastric fundus
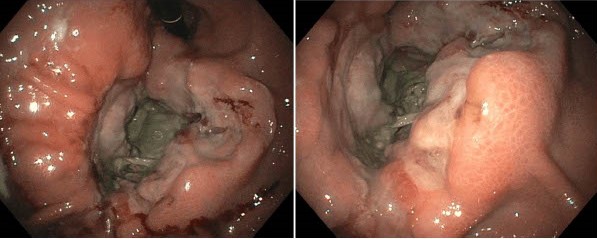
Figure: Figure 2A: H&E-stained section shows a sheet of medium to large atypical lymphoid cells infiltrating the glandular structure. Columnar-lined gastric glands are visible at the periphery of the infiltrate, highlighting the gastric mucosa amidst extensive involvement by the lymphoma.
Figure 2B: View of CD20 immunohistochemical staining, a B-cell lineage marker. The stain highlights strong membranous positivity in the intermediate to large atypical lymphoid cells, confirming their B-cell origin.
Disclosures:
Hrithik Dakssesh Putta Nagarajan indicated no relevant financial relationships.
Amit Hudgi indicated no relevant financial relationships.
Viveksandeep Thoguluva Chandrasekar indicated no relevant financial relationships.
Brandol Wolfenbarger indicated no relevant financial relationships.
Mei Zheng indicated no relevant financial relationships.
Porsha Okiye indicated no relevant financial relationships.
Hrithik Dakssesh Putta Nagarajan, MBBS1, Amit Hudgi, MD2, Viveksandeep Thoguluva Chandrasekar, MBBS1, Brandol Wolfenbarger, MD1, Mei Zheng, MD, PhD1, Porsha Okiye, MD1. P4257 - Dubious Danger – A Case Report of Gastric DLBCL Hiding in Plain Sight, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
