Monday Poster Session
Category: Stomach and Spleen
P4252 - The Domino Effect: Gastric and Pancreatic Necrosis After Splenic Embolization in Abernethy Type II Malformation
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- DM
Daniel McIntyre, DO
William Beaumont Army Medical Center
Fort Bliss, TX
Presenting Author(s)
Daniel McIntyre, DO1, Phong Nguyen, MD, MPH1, Luis Contreras-Zarate, MD2, Kyler Kozacek, DO3
1William Beaumont Army Medical Center, Fort Bliss, TX; 2William Beaumont Hospital, El Paso, TX; 3William Beaumont Army Medical Center, El Paso, TX
Introduction: Congenital portosystemic shunts (CPSS), such as Abernethy malformations, are rare vascular anomalies with potential for significant multisystem sequelae. Type II Abernethy malformation allows for partial portal flow to the liver, and interventions to manage symptoms such as splenomegaly must be approached with caution as a multidisciplinary team.
Case Description/
Methods: A 35-year-old female with symptomatic splenomegaly and known Type II Abernethy malformation underwent partial splenic embolization and a trial balloon occlusion of the CPSS to enhance hepatic portal perfusion. Her post-procedural course was marked by evolving complications due to extensive necrosis. Seven days after embolization, she developed bloody nasogastric tube output prompting an EGD. This revealed a several centimeter transmural area of gastric necrosis involving the greater curvature (Fig. A & B). Seventeen days after embolization, the patient developed worsening anemia. A CT abdomen with contrast (Fig. D) demonstrated concern for gastric perforation. A repeat EGD confirmed enlargement of the previously identified necrotic area with mucosal ulceration and interval formation of a gastro-pancreatic fistula (Fig. C). Repeat endoscopies at 31 days (Fig. E) and 65 days (Fig. F) after embolization demonstrated fistula enlargement.
During an ongoing 6-month hospitalization, she developed intra-abdominal abscesses, pleural effusions, multifocal pneumonia, and nutritional deficiencies. She has undergone several procedures including percutaneous drainage, exploratory laparotomy, J-tube placements, and advanced endoscopy for attempted gastric clips placement. Clip placements were found to be ineffective after continued gastric leak demonstrated on contrasted X-rays. She is currently undergoing transfer to specialized GI rehabilitation center for continued care.
Discussion: While partial splenic embolization is a standard treatment for symptomatic splenomegaly, its use in patients with CPSS may unpredictably alter splanchnic blood flow. In this patient, the iatrogenic ischemia extended beyond the spleen to involve the pancreatic tail and the gastric greater curvature - territories that, under normal anatomy, receive some collateral flow. The necrosis, subsequent formation of a gastro-pancreatic fistula, and perforation reflect a rare, but devastating complication that highlights the need for heightened vigilance and multi-disciplinary peri-procedural planning to anticipate and respond to atypical complications.
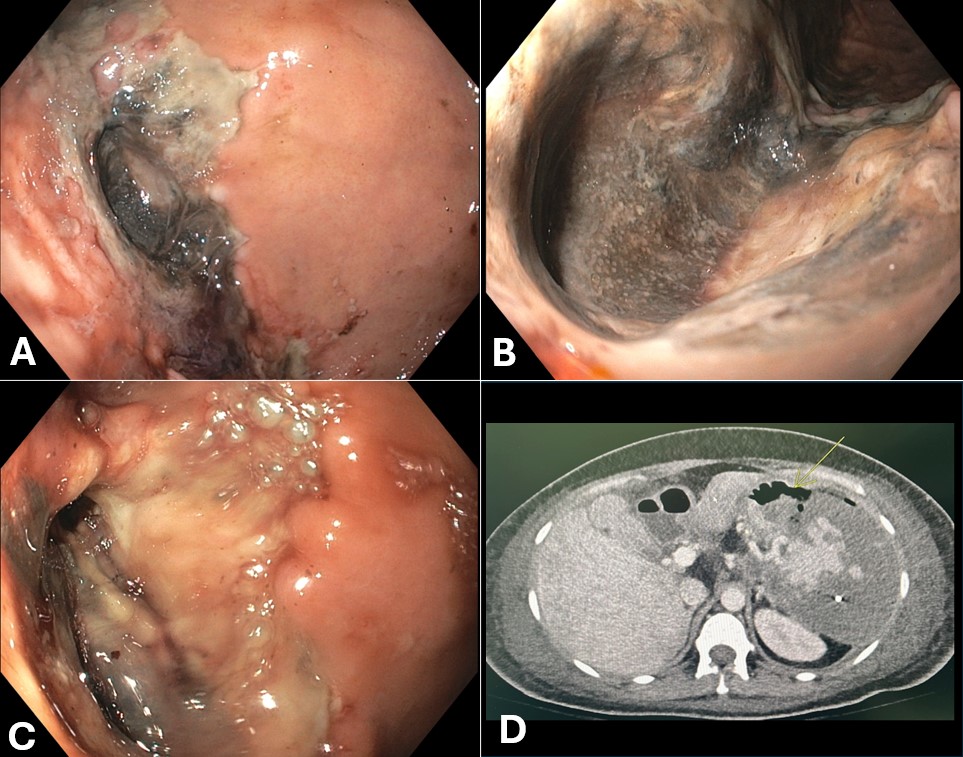
Figure: Figure A & B: EGD 7 days after embolization demonstrating gastric necrosis along the greater curvature.
Figure C: EGD 17 days after embolization demonstrating previously seen necrosis and gastro-pancreatic fistula.
Figure D: CT abdomen with contrast demonstrating gastric perforation 17 days after embolization.

Figure: Figure E: EGD 31 days after embolization demonstrating continued fistula enlargement.
Figure F: EGD 65 days after embolization demonstrating continued fistula enlargement.
Disclosures:
Daniel McIntyre indicated no relevant financial relationships.
Phong Nguyen indicated no relevant financial relationships.
Luis Contreras-Zarate indicated no relevant financial relationships.
Kyler Kozacek indicated no relevant financial relationships.
Daniel McIntyre, DO1, Phong Nguyen, MD, MPH1, Luis Contreras-Zarate, MD2, Kyler Kozacek, DO3. P4252 - The Domino Effect: Gastric and Pancreatic Necrosis After Splenic Embolization in Abernethy Type II Malformation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1William Beaumont Army Medical Center, Fort Bliss, TX; 2William Beaumont Hospital, El Paso, TX; 3William Beaumont Army Medical Center, El Paso, TX
Introduction: Congenital portosystemic shunts (CPSS), such as Abernethy malformations, are rare vascular anomalies with potential for significant multisystem sequelae. Type II Abernethy malformation allows for partial portal flow to the liver, and interventions to manage symptoms such as splenomegaly must be approached with caution as a multidisciplinary team.
Case Description/
Methods: A 35-year-old female with symptomatic splenomegaly and known Type II Abernethy malformation underwent partial splenic embolization and a trial balloon occlusion of the CPSS to enhance hepatic portal perfusion. Her post-procedural course was marked by evolving complications due to extensive necrosis. Seven days after embolization, she developed bloody nasogastric tube output prompting an EGD. This revealed a several centimeter transmural area of gastric necrosis involving the greater curvature (Fig. A & B). Seventeen days after embolization, the patient developed worsening anemia. A CT abdomen with contrast (Fig. D) demonstrated concern for gastric perforation. A repeat EGD confirmed enlargement of the previously identified necrotic area with mucosal ulceration and interval formation of a gastro-pancreatic fistula (Fig. C). Repeat endoscopies at 31 days (Fig. E) and 65 days (Fig. F) after embolization demonstrated fistula enlargement.
During an ongoing 6-month hospitalization, she developed intra-abdominal abscesses, pleural effusions, multifocal pneumonia, and nutritional deficiencies. She has undergone several procedures including percutaneous drainage, exploratory laparotomy, J-tube placements, and advanced endoscopy for attempted gastric clips placement. Clip placements were found to be ineffective after continued gastric leak demonstrated on contrasted X-rays. She is currently undergoing transfer to specialized GI rehabilitation center for continued care.
Discussion: While partial splenic embolization is a standard treatment for symptomatic splenomegaly, its use in patients with CPSS may unpredictably alter splanchnic blood flow. In this patient, the iatrogenic ischemia extended beyond the spleen to involve the pancreatic tail and the gastric greater curvature - territories that, under normal anatomy, receive some collateral flow. The necrosis, subsequent formation of a gastro-pancreatic fistula, and perforation reflect a rare, but devastating complication that highlights the need for heightened vigilance and multi-disciplinary peri-procedural planning to anticipate and respond to atypical complications.
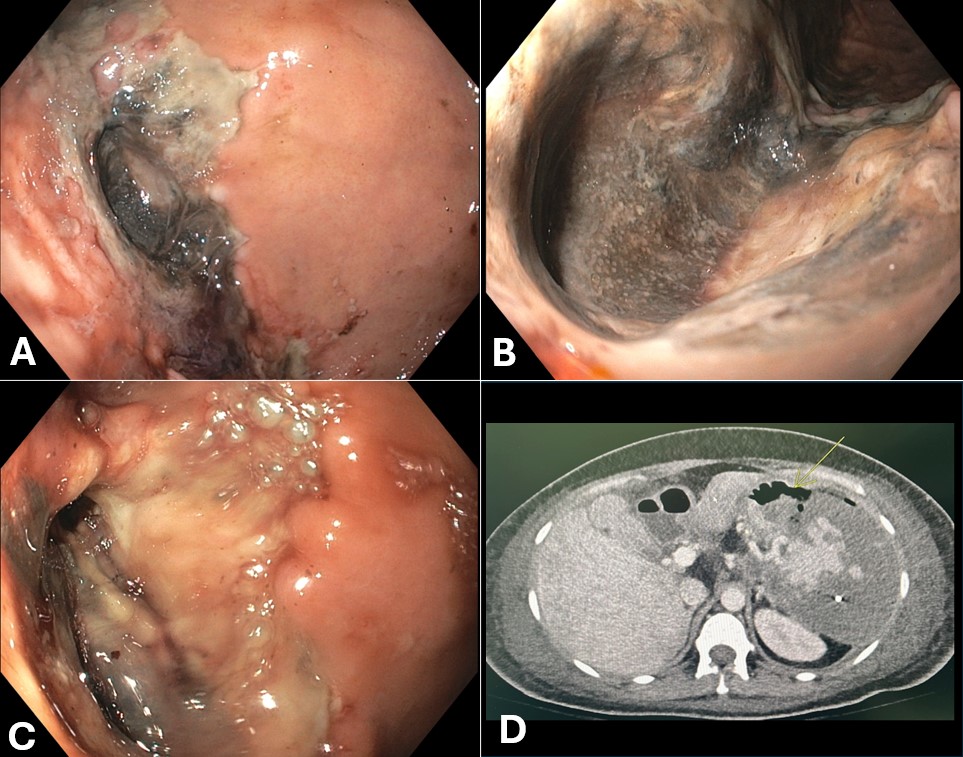
Figure: Figure A & B: EGD 7 days after embolization demonstrating gastric necrosis along the greater curvature.
Figure C: EGD 17 days after embolization demonstrating previously seen necrosis and gastro-pancreatic fistula.
Figure D: CT abdomen with contrast demonstrating gastric perforation 17 days after embolization.

Figure: Figure E: EGD 31 days after embolization demonstrating continued fistula enlargement.
Figure F: EGD 65 days after embolization demonstrating continued fistula enlargement.
Disclosures:
Daniel McIntyre indicated no relevant financial relationships.
Phong Nguyen indicated no relevant financial relationships.
Luis Contreras-Zarate indicated no relevant financial relationships.
Kyler Kozacek indicated no relevant financial relationships.
Daniel McIntyre, DO1, Phong Nguyen, MD, MPH1, Luis Contreras-Zarate, MD2, Kyler Kozacek, DO3. P4252 - The Domino Effect: Gastric and Pancreatic Necrosis After Splenic Embolization in Abernethy Type II Malformation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
