Monday Poster Session
Category: Stomach and Spleen
P4251 - A Case of Double Pylorus
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Tarek Jaber, DO
Medical College of Wisconsin
Milwaukee, WI
Presenting Author(s)
Tarek Jaber, DO, Tavia Buysse, MD, Benson Massey, MD
Medical College of Wisconsin, Milwaukee, WI
Introduction: Double pylorus (DP) is a rare condition characterized by a fistula between the stomach and the duodenal bulb. DP can be congenital or acquired but is typically the result of a penetrating peptic ulcer. We present a case of DP diagnosed with esophagogastroduodenoscopy (EGD); a consequence of a penetrating peptic ulcer disease secondary to NSAID use.
Case Description/
Methods: A 61-year-old woman with recent cervical spinal trauma from a motor vehicle accident was admitted for progressive weakness. The day prior, she experienced tarry, black stool. Since the accident, which is about 2 weeks prior, she had been using various NSAIDs for pain relief.
On physical examination, the patient had tachycardia with minimal abdominal tenderness. Digital rectal examination showed melena. Laboratory analysis showed a hemoglobin level of 9.1 g/dL from a baseline of 11 g/dL, a white blood cell count of 13,300 cells/µL, and a platelet count of 261,000 cells/µL. Her prothrombin time, hepatic, and renal function tests were within normal limits. The gastroenterology team was consulted, and the patient was started on intravenous proton pump inhibitor (PPI) therapy and fluids.
EGD revealed a severe peptic ulcer diathesis. There was an antral ulcer along the lesser curvature with a protruding visible vessel. The ulcer had eroded through the gastric wall, creating a fistula between the antrum and the duodenal bulb. The vessel was treated with epinephrine injection and bipolar cautery. Gastric biopsy pathology showed mild active chronic gastritis and was negative for Helicobacter pylori infection. The patient was advised on strict cessation of NSAIDs and was discharged with stable hemoglobin levels. Follow-up endoscopy three months later showed a healing ulcer with persistent gastroduodenal fistula.
Discussion: Double pylorus is a rare disorder characterized by a gastroduodenal fistula. Excessive NSAID usage is identified as the primary cause in many cases. Other cases have been associated with Helicobacter pylori infection. More rarely, this phenomenon has also been described as a congenital anomaly. The mechanism behind this condition involves the formation of an accessory pyloric channel because of a penetrating gastric antral ulcer. Presentations range from asymptomatic incidental finding to upper gastrointestinal bleeding. Definitive treatment targets the ulcer's cause. Management is typically conservative, with rare need for surgery. The fistula often persists and rarely closes spontaneously.
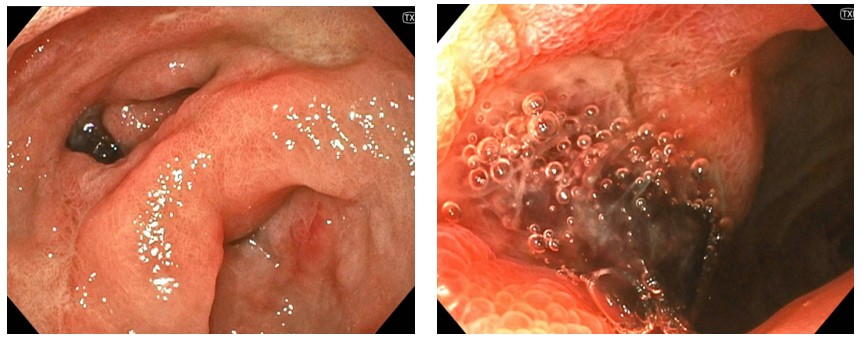
Figure: Figure (Left) demonstrates on endoscopic view of the antrum of the stomach . Antrum with visible erythema and scattered erosion. Also with a fistula within the lesser curvature of the stomach.
Figure (Right) demonstrates the duodenal bulb with visible ulceration and a bleeding vessel.
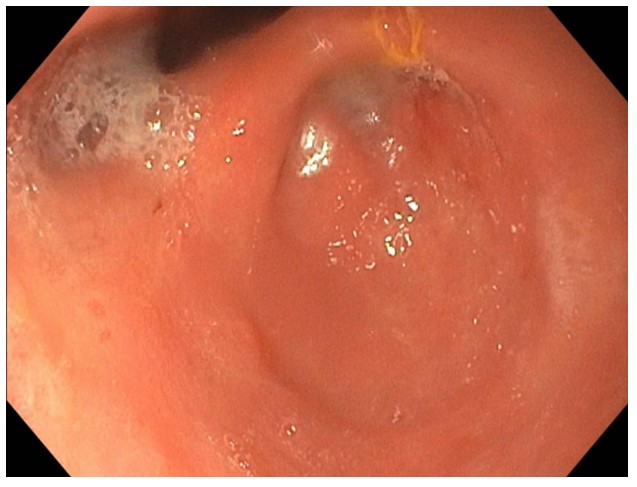
Figure: Endoscopic view of the antrum of the stomach three months later with persistent fistula and resolution of gastric erythema and erosions after NSAID cessation.
Disclosures:
Tarek Jaber indicated no relevant financial relationships.
Tavia Buysse indicated no relevant financial relationships.
Benson Massey indicated no relevant financial relationships.
Tarek Jaber, DO, Tavia Buysse, MD, Benson Massey, MD. P4251 - A Case of Double Pylorus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Medical College of Wisconsin, Milwaukee, WI
Introduction: Double pylorus (DP) is a rare condition characterized by a fistula between the stomach and the duodenal bulb. DP can be congenital or acquired but is typically the result of a penetrating peptic ulcer. We present a case of DP diagnosed with esophagogastroduodenoscopy (EGD); a consequence of a penetrating peptic ulcer disease secondary to NSAID use.
Case Description/
Methods: A 61-year-old woman with recent cervical spinal trauma from a motor vehicle accident was admitted for progressive weakness. The day prior, she experienced tarry, black stool. Since the accident, which is about 2 weeks prior, she had been using various NSAIDs for pain relief.
On physical examination, the patient had tachycardia with minimal abdominal tenderness. Digital rectal examination showed melena. Laboratory analysis showed a hemoglobin level of 9.1 g/dL from a baseline of 11 g/dL, a white blood cell count of 13,300 cells/µL, and a platelet count of 261,000 cells/µL. Her prothrombin time, hepatic, and renal function tests were within normal limits. The gastroenterology team was consulted, and the patient was started on intravenous proton pump inhibitor (PPI) therapy and fluids.
EGD revealed a severe peptic ulcer diathesis. There was an antral ulcer along the lesser curvature with a protruding visible vessel. The ulcer had eroded through the gastric wall, creating a fistula between the antrum and the duodenal bulb. The vessel was treated with epinephrine injection and bipolar cautery. Gastric biopsy pathology showed mild active chronic gastritis and was negative for Helicobacter pylori infection. The patient was advised on strict cessation of NSAIDs and was discharged with stable hemoglobin levels. Follow-up endoscopy three months later showed a healing ulcer with persistent gastroduodenal fistula.
Discussion: Double pylorus is a rare disorder characterized by a gastroduodenal fistula. Excessive NSAID usage is identified as the primary cause in many cases. Other cases have been associated with Helicobacter pylori infection. More rarely, this phenomenon has also been described as a congenital anomaly. The mechanism behind this condition involves the formation of an accessory pyloric channel because of a penetrating gastric antral ulcer. Presentations range from asymptomatic incidental finding to upper gastrointestinal bleeding. Definitive treatment targets the ulcer's cause. Management is typically conservative, with rare need for surgery. The fistula often persists and rarely closes spontaneously.
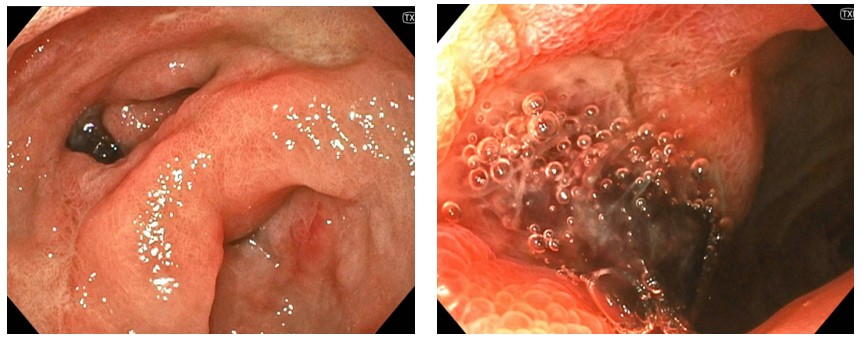
Figure: Figure (Left) demonstrates on endoscopic view of the antrum of the stomach . Antrum with visible erythema and scattered erosion. Also with a fistula within the lesser curvature of the stomach.
Figure (Right) demonstrates the duodenal bulb with visible ulceration and a bleeding vessel.
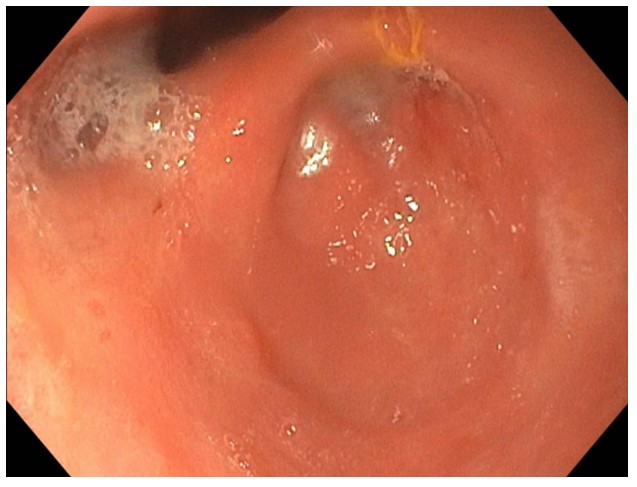
Figure: Endoscopic view of the antrum of the stomach three months later with persistent fistula and resolution of gastric erythema and erosions after NSAID cessation.
Disclosures:
Tarek Jaber indicated no relevant financial relationships.
Tavia Buysse indicated no relevant financial relationships.
Benson Massey indicated no relevant financial relationships.
Tarek Jaber, DO, Tavia Buysse, MD, Benson Massey, MD. P4251 - A Case of Double Pylorus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
