Monday Poster Session
Category: Stomach and Spleen
P4245 - The Silent Stomach: Gastric Melanoma Metastasis Revealed in a Patient With Brain Hemorrhage
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- DK
Deepa Kumarjiguda, DO (she/her/hers)
Geisinger Health System
Danville, PA
Presenting Author(s)
Deepa Kumarjiguda, DO, Ghazal Ghafari, DO, MPH, Konstaninos Damiris, DO, Sunny Patel, DO, Sara West, DO
Geisinger Health System, Danville, PA
Introduction: Melanoma is an aggressive malignancy arising from melanocytes, most commonly manifesting in the skin. It carries a high metastatic potential, with a predilection for the gastrointestinal tract—most frequently affecting the small bowel (50%), large bowel (31%), and anorectum (25%), with gastric involvement being notably rare. Gastric metastases are often asymptomatic or present with vague, nonspecific symptoms, frequently eluding detection until autopsy. Here, we describe a 65-year-old man who presented with a hemorrhagic stroke secondary to brain metastasis in the context of gastric melanoma.
Case Description/
Methods: A 65-year-old man with a history of coronary artery bypass grafting and type 2 diabetes mellitus presented with left-sided facial droop. Imaging revealed a right frontal intraparenchymal hemorrhage. Further evaluation with contrast-enhanced CT demonstrated a 2-cm exophytic lesion arising from the gastric fundus, with associated soft tissue nodules along the greater curvature as well as multiple solid pulmonary nodules (Fig 1A). Upper endoscopy revealed a friable, umbilicated gastric mass (Fig 1B). He subsequently underwent craniotomy for resection of the intracerebral mass, with pathology confirming metastatic melanoma (Fig 1C and 1D). His management included perioperative seizure prophylaxis, prolonged steroid taper, and multidisciplinary care involving neurosurgery, radiation oncology, and medical oncology. Notably, there was no prior history of melanoma.
Discussion: Gastric metastases from melanoma are rare and typically present late, due to their nonspecific clinical manifestations. Most lesions are identified in the body and fundus of the stomach. The most commonly observed endoscopic findings of gastric melanoma are melanotic nodules with ulcerated lesions at their apex. The other two endoscopic patterns include submucosal tumor-like masses which are elevated lesions and also frequently show ulceration at the apex, as in this patient. The third type are mass lesions which present variable features, including areas of necrosis and melanosis, and may also appear as simple ulcers. Immunohistochemical staining for markers including S-100 and MART-1 is essential for definitive diagnosis. The aggressive nature of gastric melanoma stems from the rich vascular supply of the stomach and portends a poor prognosis if not promptly identified. Due to the wide range of endoscopic appearances, histopathological confirmation with immunohistochemistry is crucial in establishing the diagnosis.
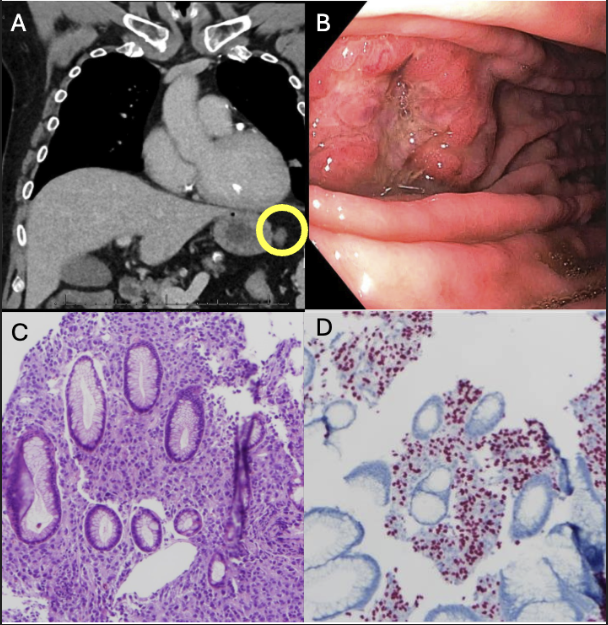
Figure: A. Exophytic mass seen protruding from stomach wall (yellow circle. B. Endoscopic image of submucosal like ulcerated mass. C. 10x H&E. Pleomorphic tumor cells confirmed as melanoma expand and infiltrate the lamina propria around pre-existing glands. D. (10x, SOX10-R): Strong distinct red nuclear staining demonstrated on the tumor cells, consistent with S100 and MART-1.
Disclosures:
Deepa Kumarjiguda indicated no relevant financial relationships.
Ghazal Ghafari indicated no relevant financial relationships.
Konstaninos Damiris indicated no relevant financial relationships.
Sunny Patel indicated no relevant financial relationships.
Sara West indicated no relevant financial relationships.
Deepa Kumarjiguda, DO, Ghazal Ghafari, DO, MPH, Konstaninos Damiris, DO, Sunny Patel, DO, Sara West, DO. P4245 - The Silent Stomach: Gastric Melanoma Metastasis Revealed in a Patient With Brain Hemorrhage, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Geisinger Health System, Danville, PA
Introduction: Melanoma is an aggressive malignancy arising from melanocytes, most commonly manifesting in the skin. It carries a high metastatic potential, with a predilection for the gastrointestinal tract—most frequently affecting the small bowel (50%), large bowel (31%), and anorectum (25%), with gastric involvement being notably rare. Gastric metastases are often asymptomatic or present with vague, nonspecific symptoms, frequently eluding detection until autopsy. Here, we describe a 65-year-old man who presented with a hemorrhagic stroke secondary to brain metastasis in the context of gastric melanoma.
Case Description/
Methods: A 65-year-old man with a history of coronary artery bypass grafting and type 2 diabetes mellitus presented with left-sided facial droop. Imaging revealed a right frontal intraparenchymal hemorrhage. Further evaluation with contrast-enhanced CT demonstrated a 2-cm exophytic lesion arising from the gastric fundus, with associated soft tissue nodules along the greater curvature as well as multiple solid pulmonary nodules (Fig 1A). Upper endoscopy revealed a friable, umbilicated gastric mass (Fig 1B). He subsequently underwent craniotomy for resection of the intracerebral mass, with pathology confirming metastatic melanoma (Fig 1C and 1D). His management included perioperative seizure prophylaxis, prolonged steroid taper, and multidisciplinary care involving neurosurgery, radiation oncology, and medical oncology. Notably, there was no prior history of melanoma.
Discussion: Gastric metastases from melanoma are rare and typically present late, due to their nonspecific clinical manifestations. Most lesions are identified in the body and fundus of the stomach. The most commonly observed endoscopic findings of gastric melanoma are melanotic nodules with ulcerated lesions at their apex. The other two endoscopic patterns include submucosal tumor-like masses which are elevated lesions and also frequently show ulceration at the apex, as in this patient. The third type are mass lesions which present variable features, including areas of necrosis and melanosis, and may also appear as simple ulcers. Immunohistochemical staining for markers including S-100 and MART-1 is essential for definitive diagnosis. The aggressive nature of gastric melanoma stems from the rich vascular supply of the stomach and portends a poor prognosis if not promptly identified. Due to the wide range of endoscopic appearances, histopathological confirmation with immunohistochemistry is crucial in establishing the diagnosis.
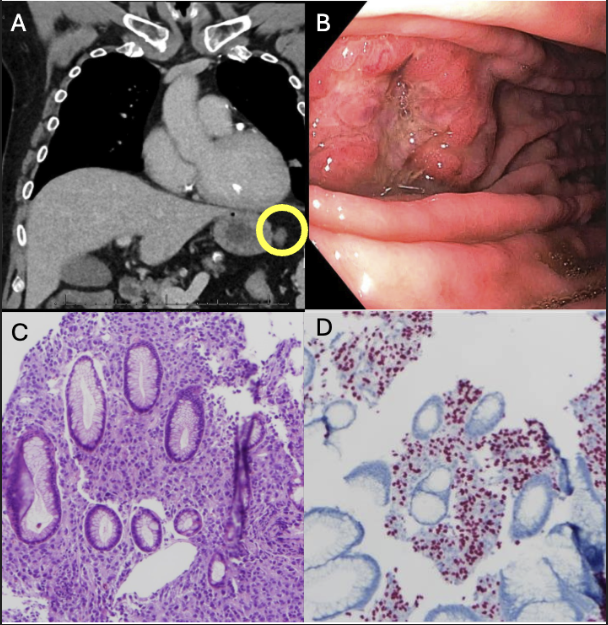
Figure: A. Exophytic mass seen protruding from stomach wall (yellow circle. B. Endoscopic image of submucosal like ulcerated mass. C. 10x H&E. Pleomorphic tumor cells confirmed as melanoma expand and infiltrate the lamina propria around pre-existing glands. D. (10x, SOX10-R): Strong distinct red nuclear staining demonstrated on the tumor cells, consistent with S100 and MART-1.
Disclosures:
Deepa Kumarjiguda indicated no relevant financial relationships.
Ghazal Ghafari indicated no relevant financial relationships.
Konstaninos Damiris indicated no relevant financial relationships.
Sunny Patel indicated no relevant financial relationships.
Sara West indicated no relevant financial relationships.
Deepa Kumarjiguda, DO, Ghazal Ghafari, DO, MPH, Konstaninos Damiris, DO, Sunny Patel, DO, Sara West, DO. P4245 - The Silent Stomach: Gastric Melanoma Metastasis Revealed in a Patient With Brain Hemorrhage, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
