Monday Poster Session
Category: Stomach and Spleen
P4212 - A Rare Case of Gastric Metastasis From Recurrent Buccal Squamous Cell Carcinoma in a Patient With Severe Anemia
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Samantha Lujan, MD (she/her/hers)
Department of Internal Medicine, Texas Health Presbyterian Hospital Dallas, Texas Health Resources, Dallas, TX
Dallas, TX
Presenting Author(s)
Samantha Lujan, MD1, Shivangini Duggal, MD2, Alejandro Robles, MD3, Roberto Gamez, MD4
1Department of Internal Medicine, Texas Health Presbyterian Hospital Dallas, Texas Health Resources, Dallas, TX, Dallas, TX; 2Department of Internal Medicine at Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso TX, USA, El Paso, TX; 3Department of Gastroenterology, Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center El Paso, El Paso , TX, El Paso, TX; 4Department of Pathology, Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center El Paso, El Paso, TX, El Paso, TX
Introduction: While primary gastric squamous cell carcinoma (GSCC) is a rare entity, comprising less than 0.1% of gastric cancers, gastric metastases from head and neck squamous cell carcinoma (HNSCC) is exceptionally rare. Our case illustrates the uncommon occurrence of gastrointestinal (GI) metastases in a patient with recurrent buccal squamous cell carcinoma (bSCC). It highlights the importance of recognizing gastric metastasis as an atypical and aggressive pattern of HNSCC and its consideration in the evaluation of unexplained anemia in this population.
Case Description/
Methods: A 68-year-old male with a history of bSCC, previously treated with surgery, radiation, and chemotherapy, presented with severe symptomatic anemia. Labs showed critically low hemoglobin (3.6 g/dL). He reported dyspnea on exertion, progressive weakness, palpitations, and occasional bright red blood per rectum, which he attributed to constipation. He denied melena or hematemesis. On exam, he was pale and cachectic but hemodynamically stable, with oral findings consistent with known bSCC recurrence. Labs were negative for hemolysis, but positive guaiac stool test and persistent anemia prompted further evaluation. He required a total of 5 units of packed red blood cells, with hemoglobin stabilizing at 7.9 g/dL. Abdominal CT showed no acute GI pathology. Esophagogastroduodenoscopy revealed a 3 cm ulcerated mass on the gastric anterior wall, which was biopsied and confirmed SCC involving the gastric mucosa.
Discussion: Both primary and metastatic SCC of the stomach are rare. Gastric metastases from HNSCC, especially of buccal mucosa origin, is highly unusual. This type of gastric metastatic spread is unusual due to the lack of direct lymphatic or hematogenous routes. Iatrogenic seeding (e.g., PEG tube placement) is a known mechanism, but our patient had no history. Isolated cases exist of HNSCC with aggressive and atypical metastatic patterns, including one that describes duodenal involvement, lending support to the plausibility of GI metastasis. Our patient's imaging showed no other metastases, affirming the uncommon nature of gastric-only spread. Gastric metastasis should be considered in patients with a history of HNSCC and persistent unexplained anemia. While localized PGSCC may be surgically treated, gastric metastases follow systemic HNSCC treatment protocols. Both scenarios portend a poor prognosis. Recognizing the potential for atypical presentations is critical for timely diagnosis, staging, and management of these patients.
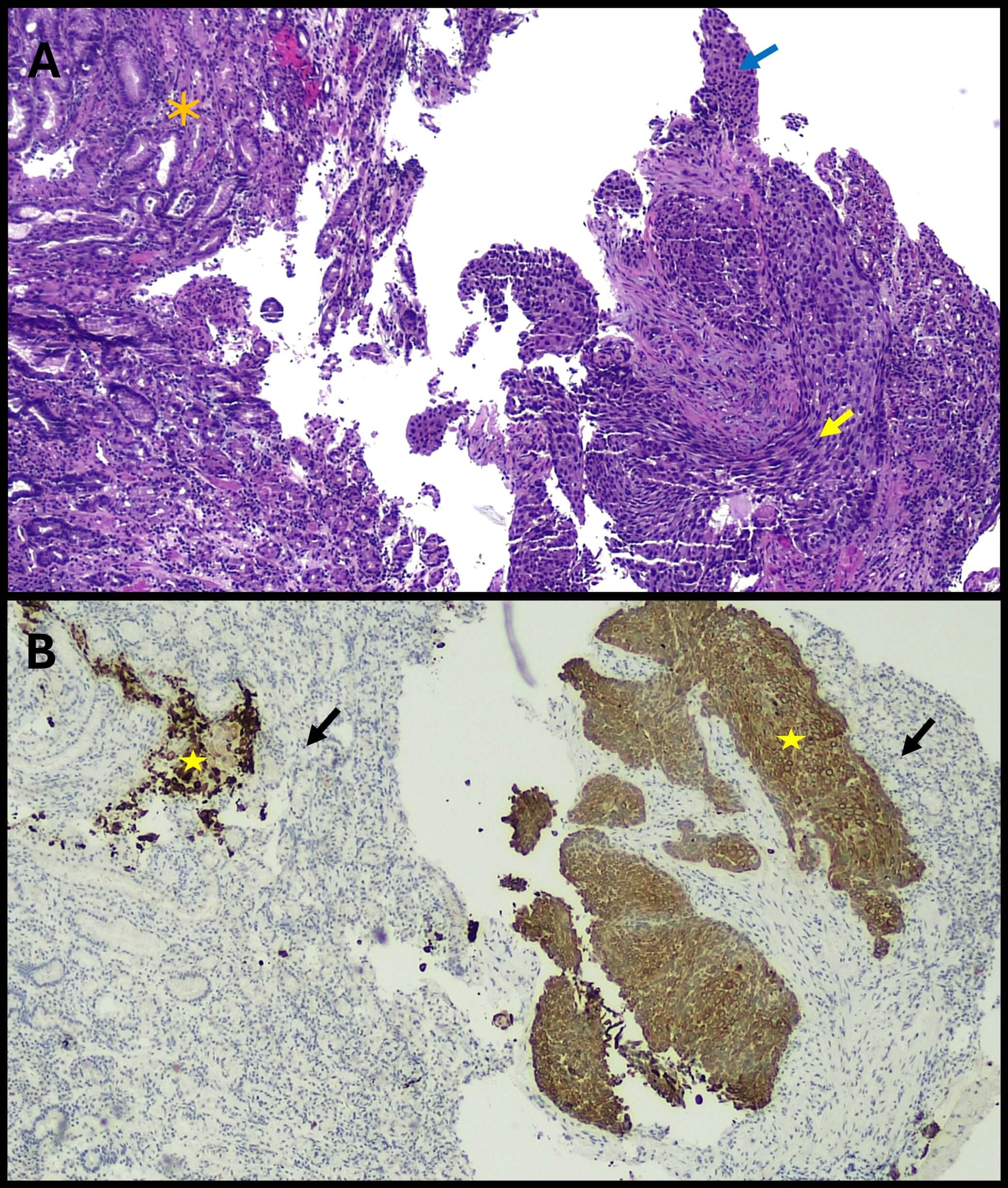
Figure: Figure 1. Endoscopic view of the proximal anterior wall of gastric body.
Image shows 3.0 cm exophytic irregular mass with central ulceration and heaped-up margins occupying the anterior wall of the stomach. Mucosa is friable with surface irregularities. Surrounding mucosa in the body and antrum showed mild-to-moderate edema and erythema.
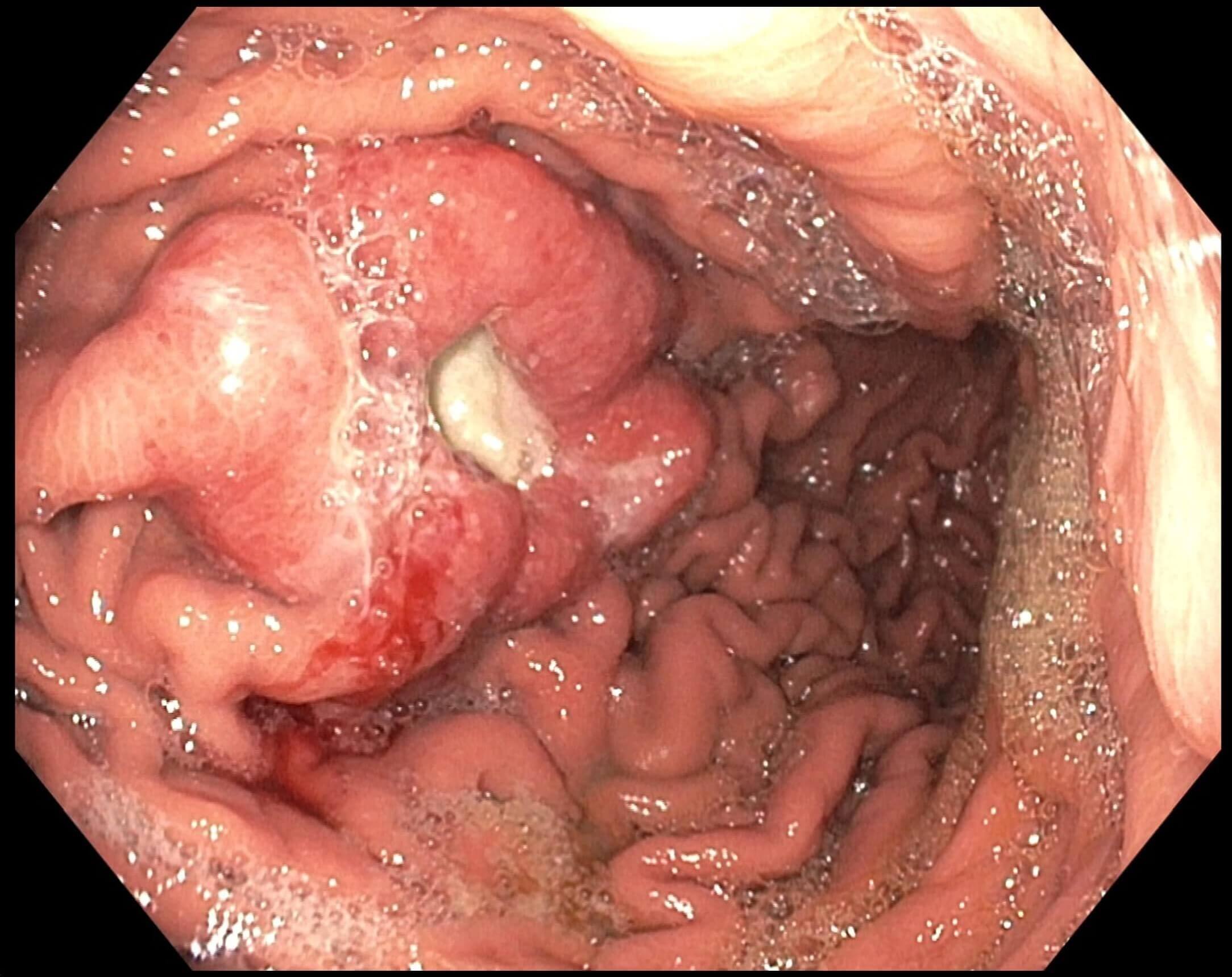
Figure: Figure 2. Endoscopic biopsy of the gastric mass
(A) Biopsy reveals gastric glandular mucosa with ulceration, acute and chronic inflammation, and reactive changes (orange asterisk), mixed with a moderately to poorly differentiated carcinoma with squamoid features. Moderately differentiated areas show focal keratinization and intercellular bridges, allowing squamous differentiation without immunohistochemical (IHC) staining (yellow arrow). Poorly differentiated areas lack keratinization and show marked atypia, making SCC diagnosis reliant on IHC markers such as CK5/6, p63, and p40 (blue arrow).
(B) CK5/6 immunostain showing diffuse cytoplasmic and perinuclear staining, supporting squamous differentiation (yellow stars). CK5/6, along with p63 and p40, helps identify squamous origin in poorly differentiated carcinomas. There is no significant CK5/6 expression in adjacent gastric glandular epithelium (black arrows).
Disclosures:
Samantha Lujan indicated no relevant financial relationships.
Shivangini Duggal indicated no relevant financial relationships.
Alejandro Robles indicated no relevant financial relationships.
Roberto Gamez indicated no relevant financial relationships.
Samantha Lujan, MD1, Shivangini Duggal, MD2, Alejandro Robles, MD3, Roberto Gamez, MD4. P4212 - A Rare Case of Gastric Metastasis From Recurrent Buccal Squamous Cell Carcinoma in a Patient With Severe Anemia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Department of Internal Medicine, Texas Health Presbyterian Hospital Dallas, Texas Health Resources, Dallas, TX, Dallas, TX; 2Department of Internal Medicine at Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso TX, USA, El Paso, TX; 3Department of Gastroenterology, Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center El Paso, El Paso , TX, El Paso, TX; 4Department of Pathology, Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center El Paso, El Paso, TX, El Paso, TX
Introduction: While primary gastric squamous cell carcinoma (GSCC) is a rare entity, comprising less than 0.1% of gastric cancers, gastric metastases from head and neck squamous cell carcinoma (HNSCC) is exceptionally rare. Our case illustrates the uncommon occurrence of gastrointestinal (GI) metastases in a patient with recurrent buccal squamous cell carcinoma (bSCC). It highlights the importance of recognizing gastric metastasis as an atypical and aggressive pattern of HNSCC and its consideration in the evaluation of unexplained anemia in this population.
Case Description/
Methods: A 68-year-old male with a history of bSCC, previously treated with surgery, radiation, and chemotherapy, presented with severe symptomatic anemia. Labs showed critically low hemoglobin (3.6 g/dL). He reported dyspnea on exertion, progressive weakness, palpitations, and occasional bright red blood per rectum, which he attributed to constipation. He denied melena or hematemesis. On exam, he was pale and cachectic but hemodynamically stable, with oral findings consistent with known bSCC recurrence. Labs were negative for hemolysis, but positive guaiac stool test and persistent anemia prompted further evaluation. He required a total of 5 units of packed red blood cells, with hemoglobin stabilizing at 7.9 g/dL. Abdominal CT showed no acute GI pathology. Esophagogastroduodenoscopy revealed a 3 cm ulcerated mass on the gastric anterior wall, which was biopsied and confirmed SCC involving the gastric mucosa.
Discussion: Both primary and metastatic SCC of the stomach are rare. Gastric metastases from HNSCC, especially of buccal mucosa origin, is highly unusual. This type of gastric metastatic spread is unusual due to the lack of direct lymphatic or hematogenous routes. Iatrogenic seeding (e.g., PEG tube placement) is a known mechanism, but our patient had no history. Isolated cases exist of HNSCC with aggressive and atypical metastatic patterns, including one that describes duodenal involvement, lending support to the plausibility of GI metastasis. Our patient's imaging showed no other metastases, affirming the uncommon nature of gastric-only spread. Gastric metastasis should be considered in patients with a history of HNSCC and persistent unexplained anemia. While localized PGSCC may be surgically treated, gastric metastases follow systemic HNSCC treatment protocols. Both scenarios portend a poor prognosis. Recognizing the potential for atypical presentations is critical for timely diagnosis, staging, and management of these patients.
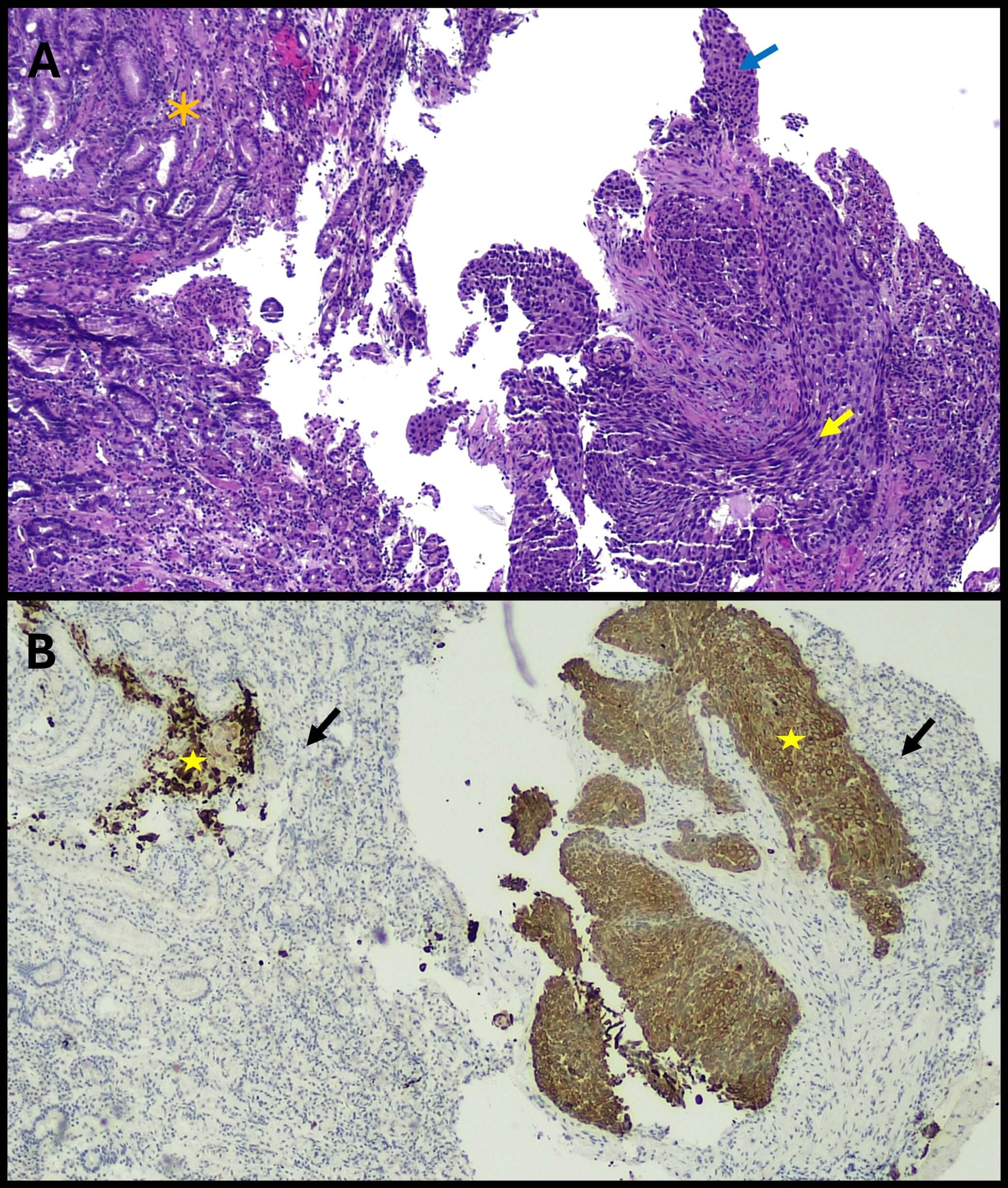
Figure: Figure 1. Endoscopic view of the proximal anterior wall of gastric body.
Image shows 3.0 cm exophytic irregular mass with central ulceration and heaped-up margins occupying the anterior wall of the stomach. Mucosa is friable with surface irregularities. Surrounding mucosa in the body and antrum showed mild-to-moderate edema and erythema.
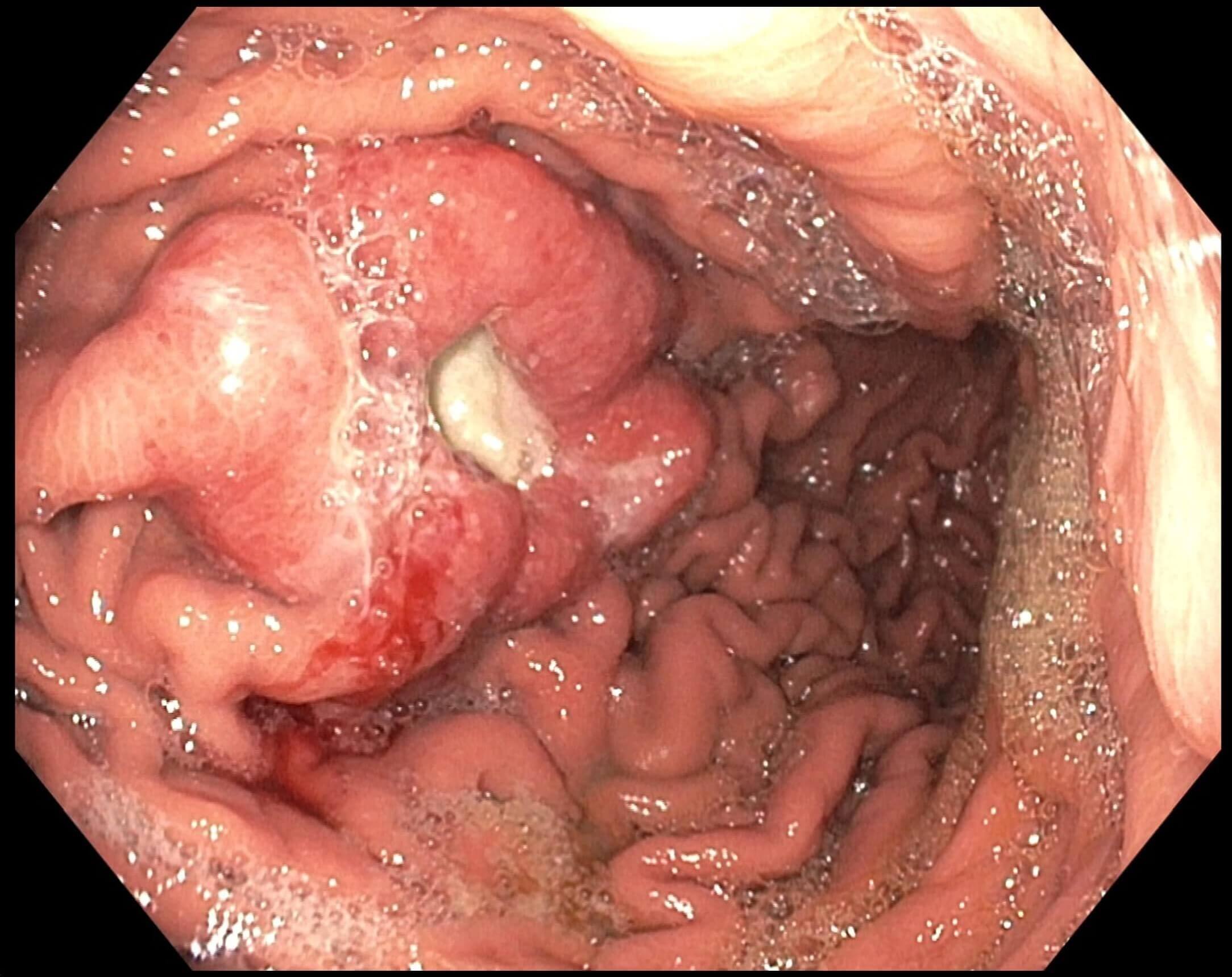
Figure: Figure 2. Endoscopic biopsy of the gastric mass
(A) Biopsy reveals gastric glandular mucosa with ulceration, acute and chronic inflammation, and reactive changes (orange asterisk), mixed with a moderately to poorly differentiated carcinoma with squamoid features. Moderately differentiated areas show focal keratinization and intercellular bridges, allowing squamous differentiation without immunohistochemical (IHC) staining (yellow arrow). Poorly differentiated areas lack keratinization and show marked atypia, making SCC diagnosis reliant on IHC markers such as CK5/6, p63, and p40 (blue arrow).
(B) CK5/6 immunostain showing diffuse cytoplasmic and perinuclear staining, supporting squamous differentiation (yellow stars). CK5/6, along with p63 and p40, helps identify squamous origin in poorly differentiated carcinomas. There is no significant CK5/6 expression in adjacent gastric glandular epithelium (black arrows).
Disclosures:
Samantha Lujan indicated no relevant financial relationships.
Shivangini Duggal indicated no relevant financial relationships.
Alejandro Robles indicated no relevant financial relationships.
Roberto Gamez indicated no relevant financial relationships.
Samantha Lujan, MD1, Shivangini Duggal, MD2, Alejandro Robles, MD3, Roberto Gamez, MD4. P4212 - A Rare Case of Gastric Metastasis From Recurrent Buccal Squamous Cell Carcinoma in a Patient With Severe Anemia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
