Monday Poster Session
Category: Stomach and Spleen
P4209 - Strongyloides: A Case Report
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Juliana Pava-De Los Rios, MD
Community Medical Center, Rutgers University
New Jersey, NJ
Presenting Author(s)
Juliana Pava-De Los Rios, MD1, Randy Rueda, MD2, Arbaaz Rao, MD2, Shreya Shambhavi, MD2, Neil Nagaria, MD2
1Community Medical Center, Rutgers University, New Jersey, NJ; 2Rutgers Health/Community Medical Center, Toms River, NJ
Introduction: Strongyloides is a soil-transmitted nematode capable of causing a wide spectrum of clinical manifestations, ranging from asymptomatic chronic infection to life-threatening hyperinfection syndrome. The diagnosis can be challenging due to its nonspecific GI and constitutional symptoms including nausea, vomiting, diarrhea, abdominal pain, and weakness, which may mimic more common conditions. Our case presents a 72-year-old male with a complex medical history, including recently diagnosed retroperitoneal fibrosis with IgG4-related disease and nephrostomy for hydronephrosis, who developed persistent GI symptoms and failure to thrive. Despite initial management for presumed gastritis and Helicobacter heilmannii infection, the patient’s condition deteriorated, which led to the discovery of Strongyloides during histopathological examination of duodenal and gastric biopsies.
Case Description/
Methods: A 72 year old male with past medical history of retroperitoneal fibrosis, nephrostomy placed 3 months prior due to hydronephrosis from the retroperitoneal mass which showed IgG4 cells. Went to the ED due to nausea, vomiting and diarrhea, burning sensation on his stomach and chest. In ED labs 127, ALT 51 AST 19, lipase 78, WBC 10.6 neutrophils 80%, HgB 14.5, Plt 285. Scheduled for EGD which showed erythematous mucosa in the gastric body and antrum. Pathology showed superficial and minimal acute inflammation with reactive changes. Helicobacter Heilmannii found. 2 weeks later patient presented to ED again due to fatigue and poor oral intake, patient got PEG tube due to failure to thrive, during the procedure found to have bleeding friable duodenal mucosa which were biopsied, the results showed ulcerated duodenal and gastric mucosa with parasites (calcified eggs), consistent with strongyloides. Patient started on Ivermectin. Patient with significant improvement after treatment, PEG tube was removed 3 months after, no recurrence of symptoms after treatment.
Discussion: Incidence of strongyloides changes widely due to geographic location. (4) The infection has a wide range of symptoms. (4) GI symptoms are usually with heartburn, vomiting and upper abdominal pain, less common patients present with diarrhea. (4) We describe a case of strongyloides infection that presents with nausea and vomiting, and associate failure to thrive, in this case the patient had no risk factors to develop the infection. Treatment for strongyloides is ivermectin, after which the patient had significant improvement of his symptoms. (4)
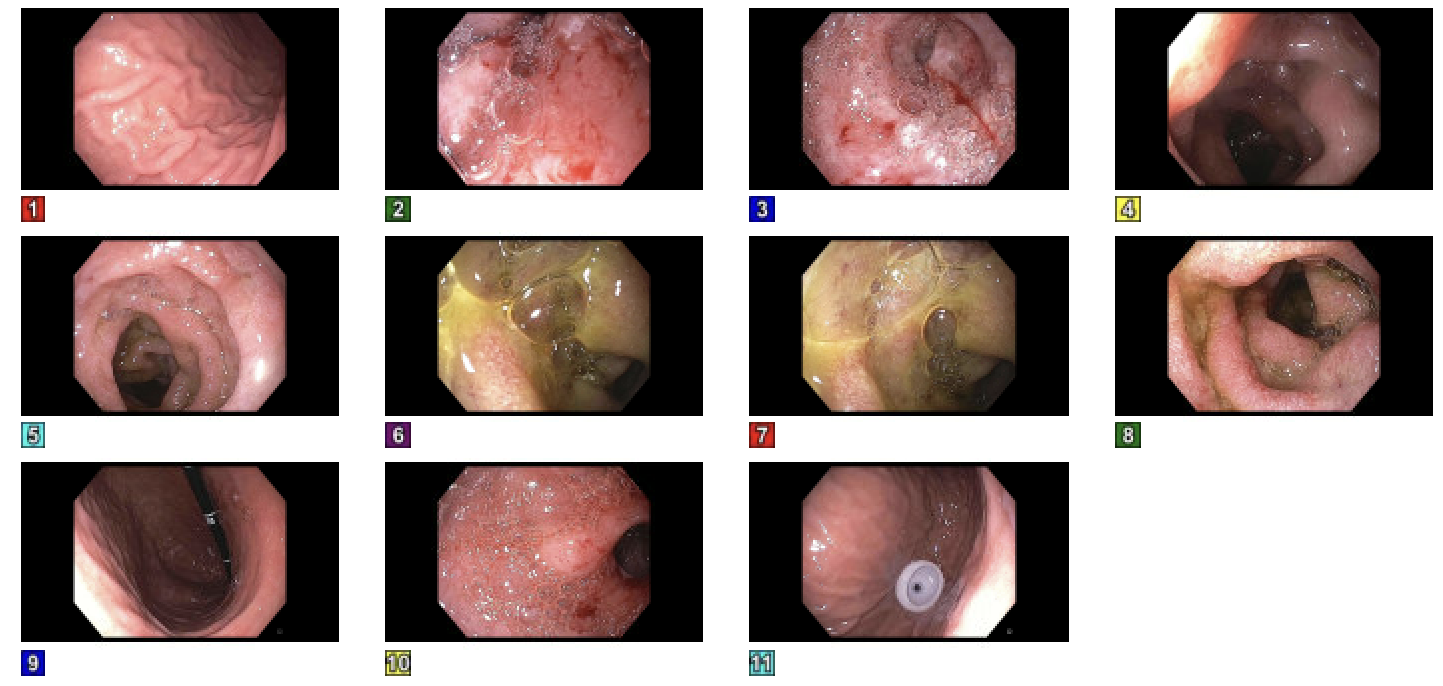
Figure: EGD with evidence of diffuse severely friable mucosa in the duodenum
Disclosures:
Juliana Pava-De Los Rios indicated no relevant financial relationships.
Randy Rueda indicated no relevant financial relationships.
Arbaaz Rao indicated no relevant financial relationships.
Shreya Shambhavi indicated no relevant financial relationships.
Neil Nagaria indicated no relevant financial relationships.
Juliana Pava-De Los Rios, MD1, Randy Rueda, MD2, Arbaaz Rao, MD2, Shreya Shambhavi, MD2, Neil Nagaria, MD2. P4209 - <i>Strongyloides</i>: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Community Medical Center, Rutgers University, New Jersey, NJ; 2Rutgers Health/Community Medical Center, Toms River, NJ
Introduction: Strongyloides is a soil-transmitted nematode capable of causing a wide spectrum of clinical manifestations, ranging from asymptomatic chronic infection to life-threatening hyperinfection syndrome. The diagnosis can be challenging due to its nonspecific GI and constitutional symptoms including nausea, vomiting, diarrhea, abdominal pain, and weakness, which may mimic more common conditions. Our case presents a 72-year-old male with a complex medical history, including recently diagnosed retroperitoneal fibrosis with IgG4-related disease and nephrostomy for hydronephrosis, who developed persistent GI symptoms and failure to thrive. Despite initial management for presumed gastritis and Helicobacter heilmannii infection, the patient’s condition deteriorated, which led to the discovery of Strongyloides during histopathological examination of duodenal and gastric biopsies.
Case Description/
Methods: A 72 year old male with past medical history of retroperitoneal fibrosis, nephrostomy placed 3 months prior due to hydronephrosis from the retroperitoneal mass which showed IgG4 cells. Went to the ED due to nausea, vomiting and diarrhea, burning sensation on his stomach and chest. In ED labs 127, ALT 51 AST 19, lipase 78, WBC 10.6 neutrophils 80%, HgB 14.5, Plt 285. Scheduled for EGD which showed erythematous mucosa in the gastric body and antrum. Pathology showed superficial and minimal acute inflammation with reactive changes. Helicobacter Heilmannii found. 2 weeks later patient presented to ED again due to fatigue and poor oral intake, patient got PEG tube due to failure to thrive, during the procedure found to have bleeding friable duodenal mucosa which were biopsied, the results showed ulcerated duodenal and gastric mucosa with parasites (calcified eggs), consistent with strongyloides. Patient started on Ivermectin. Patient with significant improvement after treatment, PEG tube was removed 3 months after, no recurrence of symptoms after treatment.
Discussion: Incidence of strongyloides changes widely due to geographic location. (4) The infection has a wide range of symptoms. (4) GI symptoms are usually with heartburn, vomiting and upper abdominal pain, less common patients present with diarrhea. (4) We describe a case of strongyloides infection that presents with nausea and vomiting, and associate failure to thrive, in this case the patient had no risk factors to develop the infection. Treatment for strongyloides is ivermectin, after which the patient had significant improvement of his symptoms. (4)
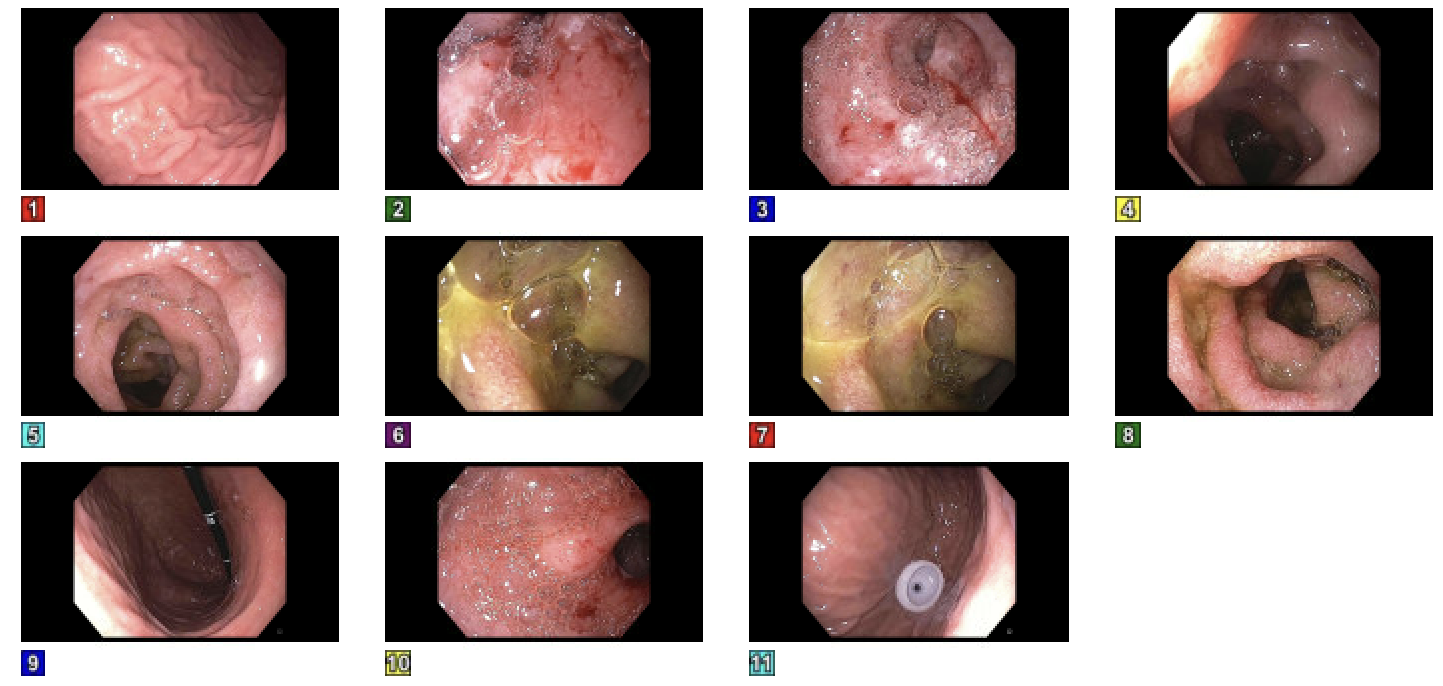
Figure: EGD with evidence of diffuse severely friable mucosa in the duodenum
Disclosures:
Juliana Pava-De Los Rios indicated no relevant financial relationships.
Randy Rueda indicated no relevant financial relationships.
Arbaaz Rao indicated no relevant financial relationships.
Shreya Shambhavi indicated no relevant financial relationships.
Neil Nagaria indicated no relevant financial relationships.
Juliana Pava-De Los Rios, MD1, Randy Rueda, MD2, Arbaaz Rao, MD2, Shreya Shambhavi, MD2, Neil Nagaria, MD2. P4209 - <i>Strongyloides</i>: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
