Monday Poster Session
Category: Stomach and Spleen
P4207 - Metastatic Squamous Cell Carcinoma of the Lung Masquerading as a Gastric Ulcer
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- IR
Ibrahim Ragab, DO
St. Luke's University Hospital
Easton, PA
Presenting Author(s)
Ibrahim Ragab, DO1, Monica Dzwonkowski, DO2, Brittney Shupp, DO2, Kimberly J. Chaput, DO3
1St. Luke's University Hospital, Bethlehem, PA; 2St. Luke's University Health Network, Bethlehem, PA; 3St Luke's Gastroenterology, Center Valley, PA
Introduction: GI bleed is a common indication for inpatient EGD, with peptic ulcer disease being a common cause. Gastric metastases can present similarly and may be missed, especially in patients with non-specific systemic symptoms. Lung cancer, particularly squamous cell carcinoma, can metastasize to the gastrointestinal tract, but gastric involvement is uncommon and can lead to delayed diagnosis.
This case illustrates an unusual presentation of metastatic lung cancer initially manifesting as melena. It highlights the importance of high clinical suspicion and a thorough EGD technique, including retroflexion, in evaluating upper GI bleeding.
Case Description/
Methods: A 74-year-old woman with a history of COPD and anxiety, presenting with increasing shortness of breath over 2 weeks that she initially attributed to the flu and had intermittent ibuprofen use. Symptoms also included intermittent epigastric pain, nausea, and vomiting. She began having melena and progressed to hematemesis as well as hemoptysis. Initial differential included peptic ulcer disease, gastritis, esophagitis, and Mallory Weiss tear.
Labs were noteworthy for a hemoglobin of 6.2 g/dL from her baseline of 11–12 g/dL. CT Chest was done and revealed a 5.8 cm cavitary mass in the right upper lobe, suspicious for malignancy. Pulmonology was consulted and bronchoscopy was planned for further evaluation.
The patient had previously been evaluated by GI 4 months prior for chronic nausea and vomiting. CT at that time raised concern for gastric ulcer vs mass in the antrum. An EGD during that hospitalization did not reveal a mass. Biopsies were performed which showed mild gastritis. Follow-up MRI was normal.
In discussion with pulmonology, it was planned to do EGD followed by bronchoscopy to evaluate the patient’s symptoms and imaging findings. EGD revealed a deep, cratered ulcer in the gastric body that was initially seen on retroflexed view. Its location and appearance was highly concerning for malignancy. Biopsy revealed poorly differentiated squamous cell carcinoma of the lung.
Discussion: This case highlights the diagnostic dilemma of GI presentation of metastatic lung cancer and the requirement of thorough evaluation during EGD. Retroflexion on EGD is a valuable technique that can demonstrate lesions in anatomically challenging regions such as the gastric cardia, where pathology could be missed on forward view only. Proper technique with thorough mucosal inspection with retroflexion is required to avoid delayed or missed diagnosis.
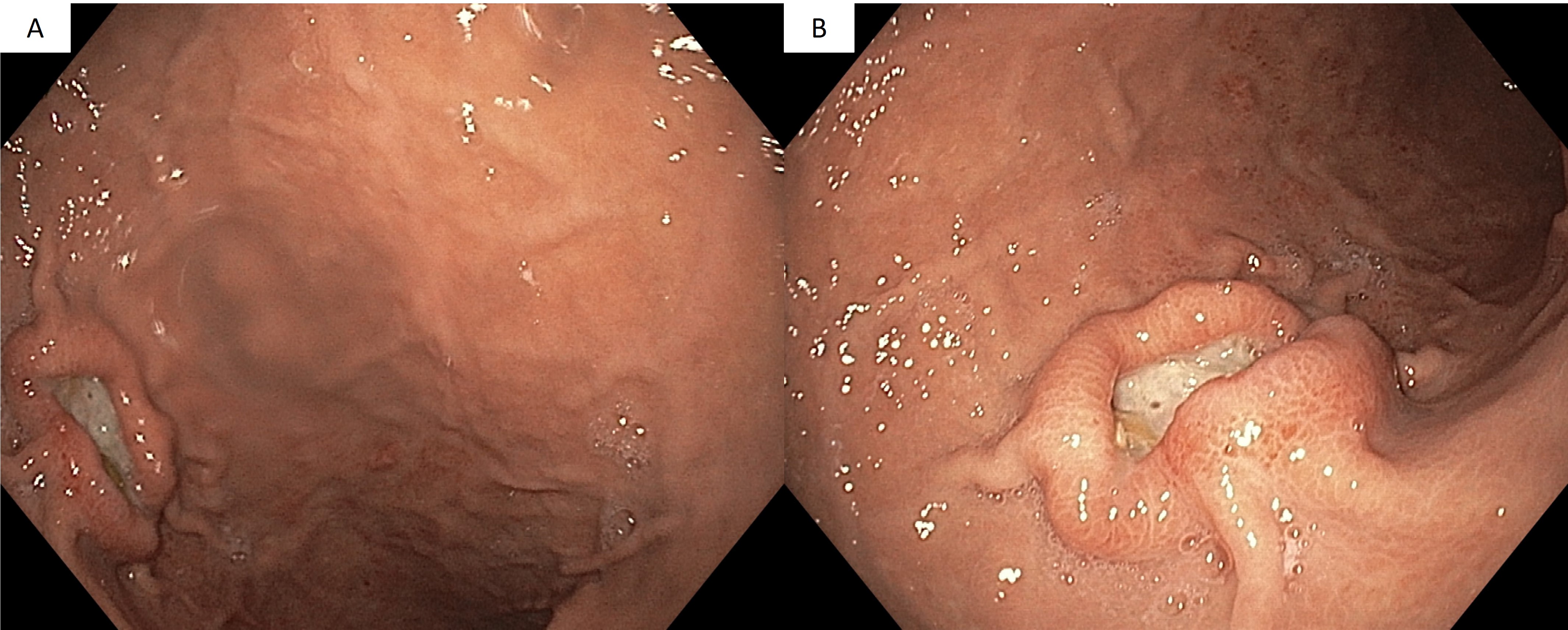
Figure: A. Deep cratered ulcer in the gastric body initially seen on retroflexion
B. Deep cratered ulcer in the gastric body
Disclosures:
Ibrahim Ragab indicated no relevant financial relationships.
Monica Dzwonkowski indicated no relevant financial relationships.
Brittney Shupp indicated no relevant financial relationships.
Kimberly Chaput indicated no relevant financial relationships.
Ibrahim Ragab, DO1, Monica Dzwonkowski, DO2, Brittney Shupp, DO2, Kimberly J. Chaput, DO3. P4207 - Metastatic Squamous Cell Carcinoma of the Lung Masquerading as a Gastric Ulcer, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1St. Luke's University Hospital, Bethlehem, PA; 2St. Luke's University Health Network, Bethlehem, PA; 3St Luke's Gastroenterology, Center Valley, PA
Introduction: GI bleed is a common indication for inpatient EGD, with peptic ulcer disease being a common cause. Gastric metastases can present similarly and may be missed, especially in patients with non-specific systemic symptoms. Lung cancer, particularly squamous cell carcinoma, can metastasize to the gastrointestinal tract, but gastric involvement is uncommon and can lead to delayed diagnosis.
This case illustrates an unusual presentation of metastatic lung cancer initially manifesting as melena. It highlights the importance of high clinical suspicion and a thorough EGD technique, including retroflexion, in evaluating upper GI bleeding.
Case Description/
Methods: A 74-year-old woman with a history of COPD and anxiety, presenting with increasing shortness of breath over 2 weeks that she initially attributed to the flu and had intermittent ibuprofen use. Symptoms also included intermittent epigastric pain, nausea, and vomiting. She began having melena and progressed to hematemesis as well as hemoptysis. Initial differential included peptic ulcer disease, gastritis, esophagitis, and Mallory Weiss tear.
Labs were noteworthy for a hemoglobin of 6.2 g/dL from her baseline of 11–12 g/dL. CT Chest was done and revealed a 5.8 cm cavitary mass in the right upper lobe, suspicious for malignancy. Pulmonology was consulted and bronchoscopy was planned for further evaluation.
The patient had previously been evaluated by GI 4 months prior for chronic nausea and vomiting. CT at that time raised concern for gastric ulcer vs mass in the antrum. An EGD during that hospitalization did not reveal a mass. Biopsies were performed which showed mild gastritis. Follow-up MRI was normal.
In discussion with pulmonology, it was planned to do EGD followed by bronchoscopy to evaluate the patient’s symptoms and imaging findings. EGD revealed a deep, cratered ulcer in the gastric body that was initially seen on retroflexed view. Its location and appearance was highly concerning for malignancy. Biopsy revealed poorly differentiated squamous cell carcinoma of the lung.
Discussion: This case highlights the diagnostic dilemma of GI presentation of metastatic lung cancer and the requirement of thorough evaluation during EGD. Retroflexion on EGD is a valuable technique that can demonstrate lesions in anatomically challenging regions such as the gastric cardia, where pathology could be missed on forward view only. Proper technique with thorough mucosal inspection with retroflexion is required to avoid delayed or missed diagnosis.
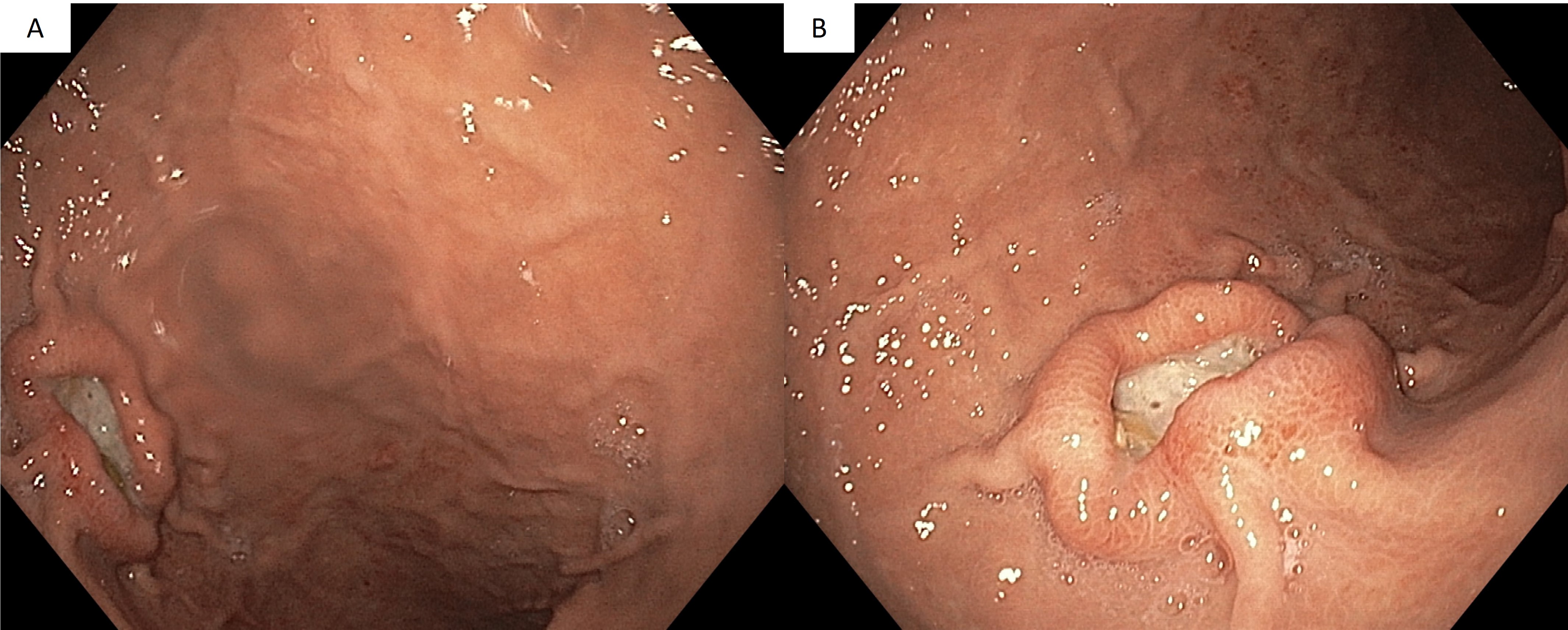
Figure: A. Deep cratered ulcer in the gastric body initially seen on retroflexion
B. Deep cratered ulcer in the gastric body
Disclosures:
Ibrahim Ragab indicated no relevant financial relationships.
Monica Dzwonkowski indicated no relevant financial relationships.
Brittney Shupp indicated no relevant financial relationships.
Kimberly Chaput indicated no relevant financial relationships.
Ibrahim Ragab, DO1, Monica Dzwonkowski, DO2, Brittney Shupp, DO2, Kimberly J. Chaput, DO3. P4207 - Metastatic Squamous Cell Carcinoma of the Lung Masquerading as a Gastric Ulcer, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
