Monday Poster Session
Category: Stomach and Spleen
P4195 - Clinical and Histopathological Characteristics of Patients With Autoimmune Gastritis at a US Tertiary Care Center
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Joelle Bou Saba, MD (she/her/hers)
Cleveland Clinic Foundation
Cleveland, OH
Presenting Author(s)
Joelle Bou Saba, MD1, Joseph Hajj, MD1, Joya-Rita Hindy, MD1, Tarek Souaid, MD, MPH1, John McMichael, PhD1, Kyungran Justina Cho, MD, PhD2, Michelle Kang Kim, MD, PhD3, Carol Rouphael, MD3
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic Foundation, Pepper Pike, OH; 3Cleveland Clinic, Cleveland, OH
Introduction: Autoimmune gastritis (AIG) is a chronic autoimmune condition of the stomach with a worldwide prevalence of 0.5-4.5%. AIG has been primarily studied in European and East Asian populations. To our knowledge, few studies have characterized patients with AIG in the United States (US). We describe the clinical, endoscopic and histopathological characteristics of patients with AIG at a US tertiary care center.
Methods: In this retrospective cohort study, we included a random cohort of adult patients who underwent upper endoscopy (EGD) between 2010 and 2022, and who had gastric biopsies demonstrating histopathologic features consistent with AIG, defined as corpus atrophy with enterochromaffin-like cell hyperplasia. Patients with history of reflux esophagitis, gastrectomy or Helicobacter pylori gastritis were excluded. Demographic, clinical, laboratory, endoscopic and pathology characteristics were collected. Descriptive statistics were applied.
Results: A total of 126 patients were included. 75% were female and 72% White (Table 1). Mean age at the time of EGD diagnostic of AIG was 60 ±17 years. 93 % of patients had gastrointestinal (GI) symptoms, with abdominal pain (45%) and heartburn (42%) being the most common. Among all autoimmune disorders, Hashimoto thyroiditis was the most common in 23 % of patients. 63% (62/98) and 69% (64/92) had vitamin B12 and iron deficiency, respectively. Out of 94 patients tested for AIG serologies, 83% had either a positive intrinsic factor or parietal cell antibody. 62% had gastric intestinal metaplasia, 9.5% had a gastric neuroendocrine tumor type 1, two had gastric dysplasia, and one patient had gastric adenocarcinoma.
Discussion: In our US cohort of AIG patients, most had GI symptoms with heartburn, likely functional, being a common one, suggesting that AIG may be under-recognized in patients with nonspecific upper GI complaints. Our findings of prevalent vitamin B12 and iron deficiencies, as well as pre-neoplastic and neoplastic lesions at diagnosis, emphasize the need for early disease recognition to improve neoplastic outcomes through surveillance, and implement periodic screening for thyroid disease and nutritional deficiencies.
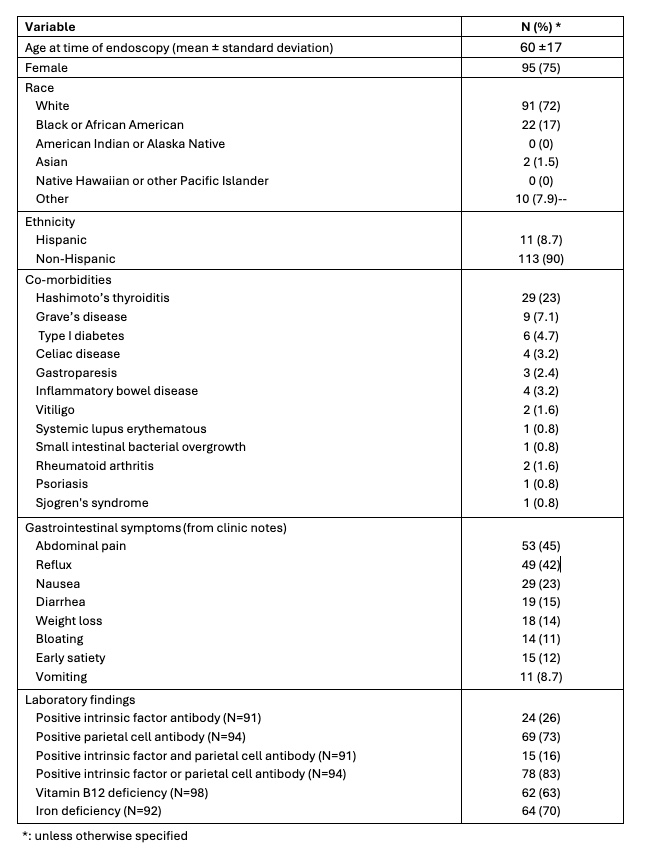
Figure: Table 1: Demographic and clinical characteristics
Disclosures:
Joelle Bou Saba indicated no relevant financial relationships.
Joseph Hajj indicated no relevant financial relationships.
Joya-Rita Hindy indicated no relevant financial relationships.
Tarek Souaid indicated no relevant financial relationships.
John McMichael indicated no relevant financial relationships.
Kyungran Justina Cho indicated no relevant financial relationships.
Michelle Kang Kim indicated no relevant financial relationships.
Carol Rouphael indicated no relevant financial relationships.
Joelle Bou Saba, MD1, Joseph Hajj, MD1, Joya-Rita Hindy, MD1, Tarek Souaid, MD, MPH1, John McMichael, PhD1, Kyungran Justina Cho, MD, PhD2, Michelle Kang Kim, MD, PhD3, Carol Rouphael, MD3. P4195 - Clinical and Histopathological Characteristics of Patients With Autoimmune Gastritis at a US Tertiary Care Center, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic Foundation, Pepper Pike, OH; 3Cleveland Clinic, Cleveland, OH
Introduction: Autoimmune gastritis (AIG) is a chronic autoimmune condition of the stomach with a worldwide prevalence of 0.5-4.5%. AIG has been primarily studied in European and East Asian populations. To our knowledge, few studies have characterized patients with AIG in the United States (US). We describe the clinical, endoscopic and histopathological characteristics of patients with AIG at a US tertiary care center.
Methods: In this retrospective cohort study, we included a random cohort of adult patients who underwent upper endoscopy (EGD) between 2010 and 2022, and who had gastric biopsies demonstrating histopathologic features consistent with AIG, defined as corpus atrophy with enterochromaffin-like cell hyperplasia. Patients with history of reflux esophagitis, gastrectomy or Helicobacter pylori gastritis were excluded. Demographic, clinical, laboratory, endoscopic and pathology characteristics were collected. Descriptive statistics were applied.
Results: A total of 126 patients were included. 75% were female and 72% White (Table 1). Mean age at the time of EGD diagnostic of AIG was 60 ±17 years. 93 % of patients had gastrointestinal (GI) symptoms, with abdominal pain (45%) and heartburn (42%) being the most common. Among all autoimmune disorders, Hashimoto thyroiditis was the most common in 23 % of patients. 63% (62/98) and 69% (64/92) had vitamin B12 and iron deficiency, respectively. Out of 94 patients tested for AIG serologies, 83% had either a positive intrinsic factor or parietal cell antibody. 62% had gastric intestinal metaplasia, 9.5% had a gastric neuroendocrine tumor type 1, two had gastric dysplasia, and one patient had gastric adenocarcinoma.
Discussion: In our US cohort of AIG patients, most had GI symptoms with heartburn, likely functional, being a common one, suggesting that AIG may be under-recognized in patients with nonspecific upper GI complaints. Our findings of prevalent vitamin B12 and iron deficiencies, as well as pre-neoplastic and neoplastic lesions at diagnosis, emphasize the need for early disease recognition to improve neoplastic outcomes through surveillance, and implement periodic screening for thyroid disease and nutritional deficiencies.
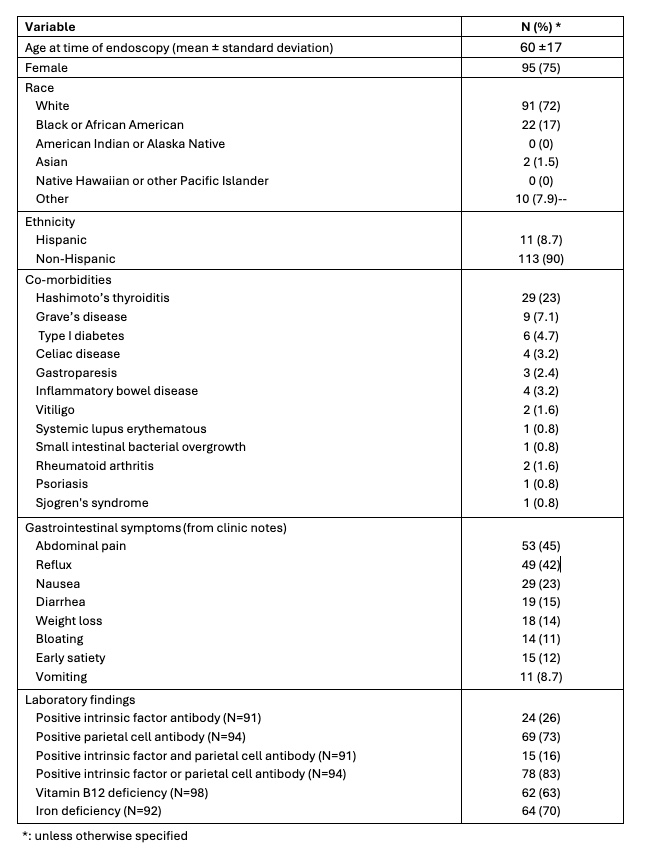
Figure: Table 1: Demographic and clinical characteristics
Disclosures:
Joelle Bou Saba indicated no relevant financial relationships.
Joseph Hajj indicated no relevant financial relationships.
Joya-Rita Hindy indicated no relevant financial relationships.
Tarek Souaid indicated no relevant financial relationships.
John McMichael indicated no relevant financial relationships.
Kyungran Justina Cho indicated no relevant financial relationships.
Michelle Kang Kim indicated no relevant financial relationships.
Carol Rouphael indicated no relevant financial relationships.
Joelle Bou Saba, MD1, Joseph Hajj, MD1, Joya-Rita Hindy, MD1, Tarek Souaid, MD, MPH1, John McMichael, PhD1, Kyungran Justina Cho, MD, PhD2, Michelle Kang Kim, MD, PhD3, Carol Rouphael, MD3. P4195 - Clinical and Histopathological Characteristics of Patients With Autoimmune Gastritis at a US Tertiary Care Center, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
