Monday Poster Session
Category: Stomach and Spleen
P4191 - Gastric Intestinal Metaplasia as a Precursor to Gastric Cancer: A Cohort Analysis of Risk Factors
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Avneet Kaur, MBBS (she/her/hers)
SUNY Upstate Medical University
Syracuse, NY
Presenting Author(s)
Avneet Kaur, MBBS1, Anjul Verma, MD2, Akhil Gupta, MBBS3, Babu P. Mohan, MD4
1SUNY Upstate Medical University, Syracuse, NY; 2Texas Tech University Health Sciences Center, Odessa, TX; 3Government Medical College, Patiala, Ambala, Haryana, India; 4Orlando Gastroenterology PA, Orlando, FL
Introduction: Gastric intestinal metaplasia (GIM) is a known precursor to gastric cancer (GC), but its absolute risk and associated factors remain incompletely defined. This study assesses the incidence of GC in patients with GIM and examines related clinical and demographic risk factors using a large population-based dataset.
Methods: A retrospective cohort study was conducted using the TriNetX Global Collaborative Network. Adult patients (≥18 years) diagnosed with GC were identified using ICD-10 codes. Two cohorts were formed: (1) GC patients with a prior diagnosis of GIM (at least one month before GC diagnosis), and (2) GC patients without any GIM history. We evaluated 36 demographic and clinical variables, including H. pylori infection, gastric/duodenal polyps, autoimmune conditions, and substance use. Fisher’s exact test was used to assess significance (alpha = 0.05).
Results: Of 204,091 GC cases identified, 203,843 involved adults. Among them, 1,018 had a prior GIM diagnosis, yielding a 0.5% incidence of GIM-associated GC. Cohort 1 (GC with prior GIM) and Cohort 2 (GC without GIM) were compared. The mean age was similar (71.5 vs. 71.2 years), but significant ethnic differences were noted: 44% White, 21% Asian, and 16% Black in Cohort 1, versus 32%, 7%, and 6% respectively in Cohort 2 (p < 0.001).
Several comorbid conditions were significantly more prevalent in the GIM group. H. pylori was present in 16% vs. 4% (OR 4.85, 95% CI: 4.04–5.81, p < 0.001), gastric/duodenal polyps in 30% vs. 4% (OR 10.01, 95% CI: 8.66–11.57, p < 0.001), and adult hypertrophic pyloric stenosis in 8% vs. 4% (OR 2.47, 95% CI: 1.94–3.14, p < 0.001). Autoimmune conditions also showed strong associations, with Sjögren’s syndrome (OR 10.32, p < 0.001) and rheumatoid arthritis (18% vs. 9%; OR 2.13, p < 0.001). Substance use was more common in Cohort 1, including cannabis (4% vs. 1%, OR 3.16) and opioids (3% vs. 1%, OR 2.43), both p < 0.001.
Discussion: This study reveals a 0.5% incidence of GC in patients with GIM and highlights key clinical and demographic differences between patients with and without GIM. The strong associations with ethnicity, H. pylori infection, gastric polyps, autoimmune diseases, and substance use suggest multifactorial contributors to cancer progression in this high-risk population.
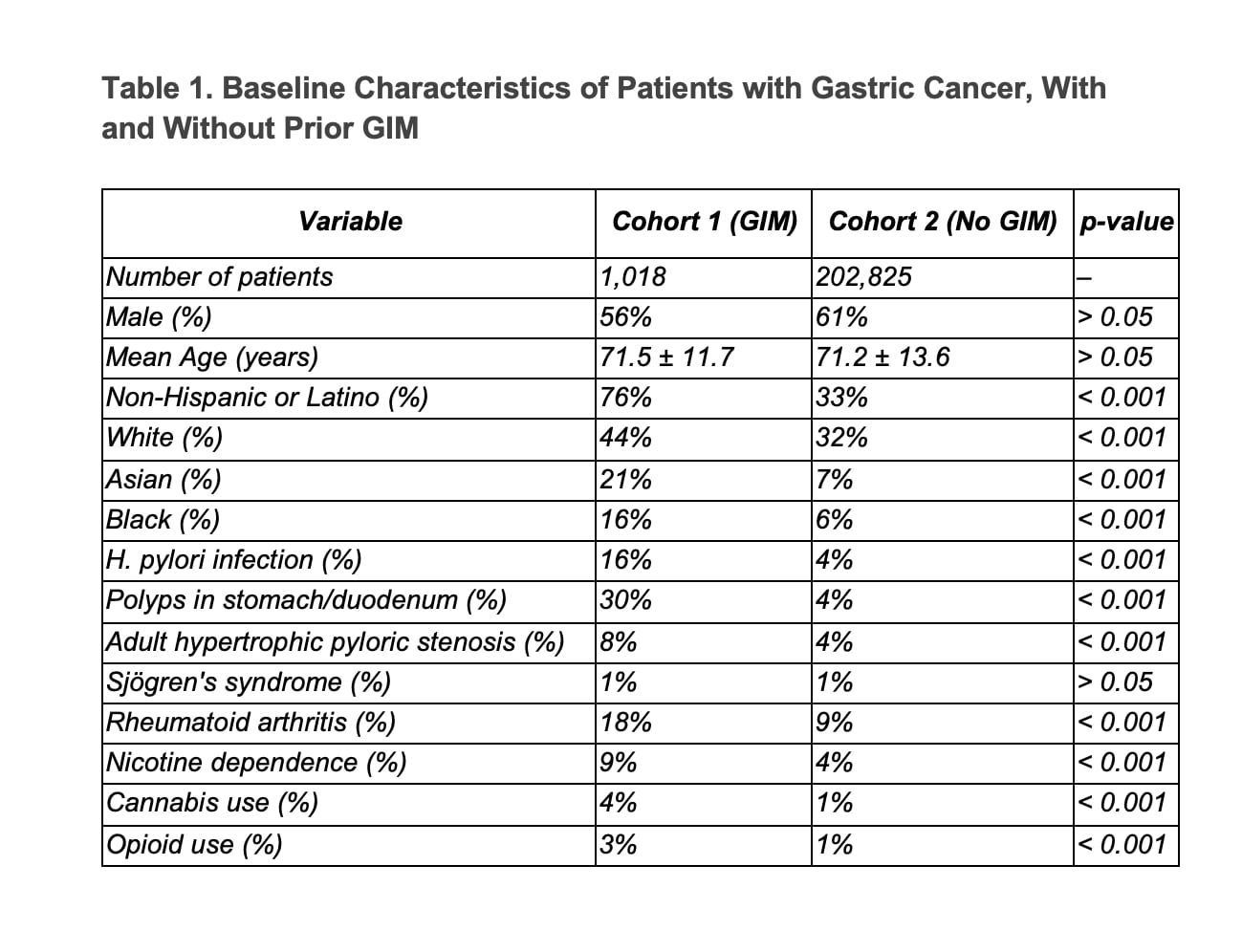
Figure: Table1. Baseline Characteristics of patients with Gastric Cancer, with and without Prior GIM
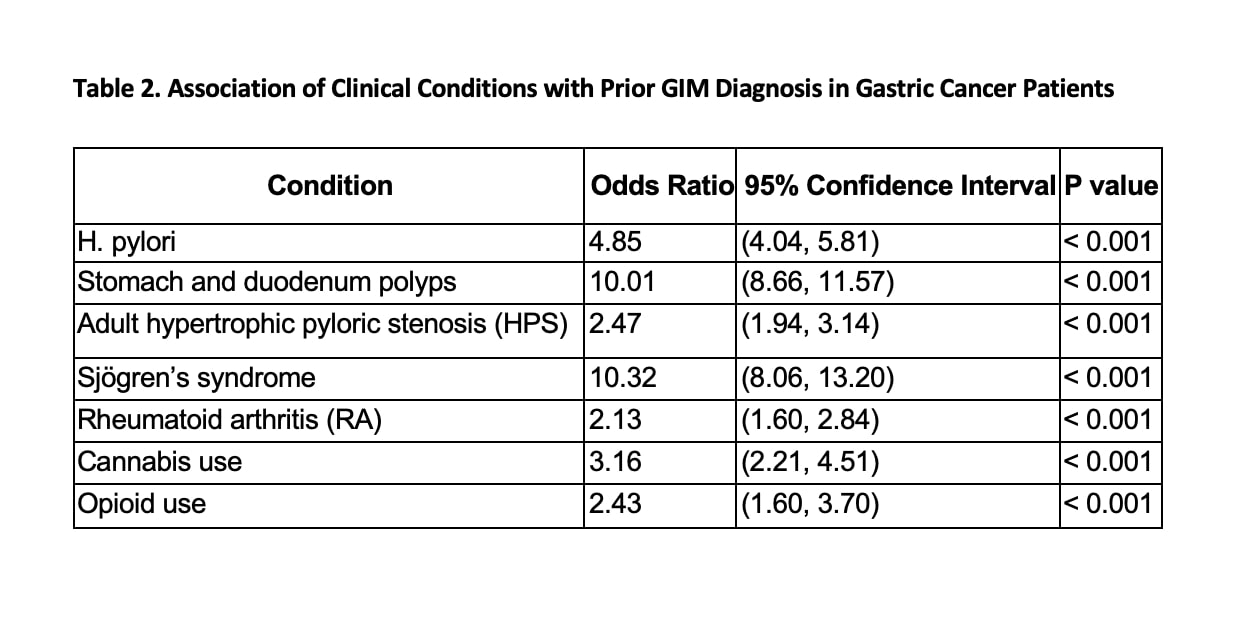
Figure: Table 2. Association of clinical conditions with Prior GIM Diagnosis in patient's with Gastric Cancer
Disclosures:
Avneet Kaur indicated no relevant financial relationships.
Anjul Verma indicated no relevant financial relationships.
Akhil Gupta indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Avneet Kaur, MBBS1, Anjul Verma, MD2, Akhil Gupta, MBBS3, Babu P. Mohan, MD4. P4191 - Gastric Intestinal Metaplasia as a Precursor to Gastric Cancer: A Cohort Analysis of Risk Factors, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1SUNY Upstate Medical University, Syracuse, NY; 2Texas Tech University Health Sciences Center, Odessa, TX; 3Government Medical College, Patiala, Ambala, Haryana, India; 4Orlando Gastroenterology PA, Orlando, FL
Introduction: Gastric intestinal metaplasia (GIM) is a known precursor to gastric cancer (GC), but its absolute risk and associated factors remain incompletely defined. This study assesses the incidence of GC in patients with GIM and examines related clinical and demographic risk factors using a large population-based dataset.
Methods: A retrospective cohort study was conducted using the TriNetX Global Collaborative Network. Adult patients (≥18 years) diagnosed with GC were identified using ICD-10 codes. Two cohorts were formed: (1) GC patients with a prior diagnosis of GIM (at least one month before GC diagnosis), and (2) GC patients without any GIM history. We evaluated 36 demographic and clinical variables, including H. pylori infection, gastric/duodenal polyps, autoimmune conditions, and substance use. Fisher’s exact test was used to assess significance (alpha = 0.05).
Results: Of 204,091 GC cases identified, 203,843 involved adults. Among them, 1,018 had a prior GIM diagnosis, yielding a 0.5% incidence of GIM-associated GC. Cohort 1 (GC with prior GIM) and Cohort 2 (GC without GIM) were compared. The mean age was similar (71.5 vs. 71.2 years), but significant ethnic differences were noted: 44% White, 21% Asian, and 16% Black in Cohort 1, versus 32%, 7%, and 6% respectively in Cohort 2 (p < 0.001).
Several comorbid conditions were significantly more prevalent in the GIM group. H. pylori was present in 16% vs. 4% (OR 4.85, 95% CI: 4.04–5.81, p < 0.001), gastric/duodenal polyps in 30% vs. 4% (OR 10.01, 95% CI: 8.66–11.57, p < 0.001), and adult hypertrophic pyloric stenosis in 8% vs. 4% (OR 2.47, 95% CI: 1.94–3.14, p < 0.001). Autoimmune conditions also showed strong associations, with Sjögren’s syndrome (OR 10.32, p < 0.001) and rheumatoid arthritis (18% vs. 9%; OR 2.13, p < 0.001). Substance use was more common in Cohort 1, including cannabis (4% vs. 1%, OR 3.16) and opioids (3% vs. 1%, OR 2.43), both p < 0.001.
Discussion: This study reveals a 0.5% incidence of GC in patients with GIM and highlights key clinical and demographic differences between patients with and without GIM. The strong associations with ethnicity, H. pylori infection, gastric polyps, autoimmune diseases, and substance use suggest multifactorial contributors to cancer progression in this high-risk population.
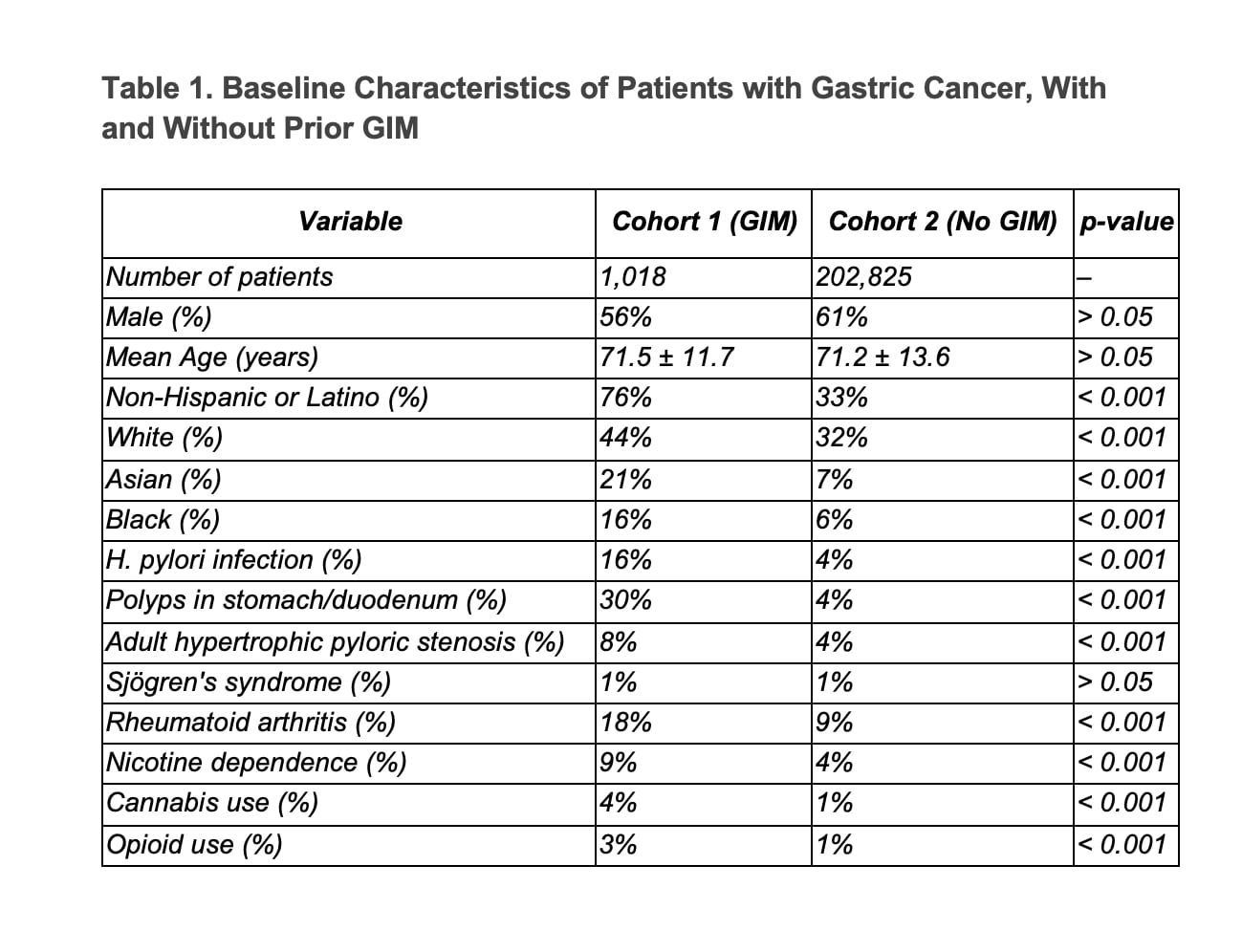
Figure: Table1. Baseline Characteristics of patients with Gastric Cancer, with and without Prior GIM
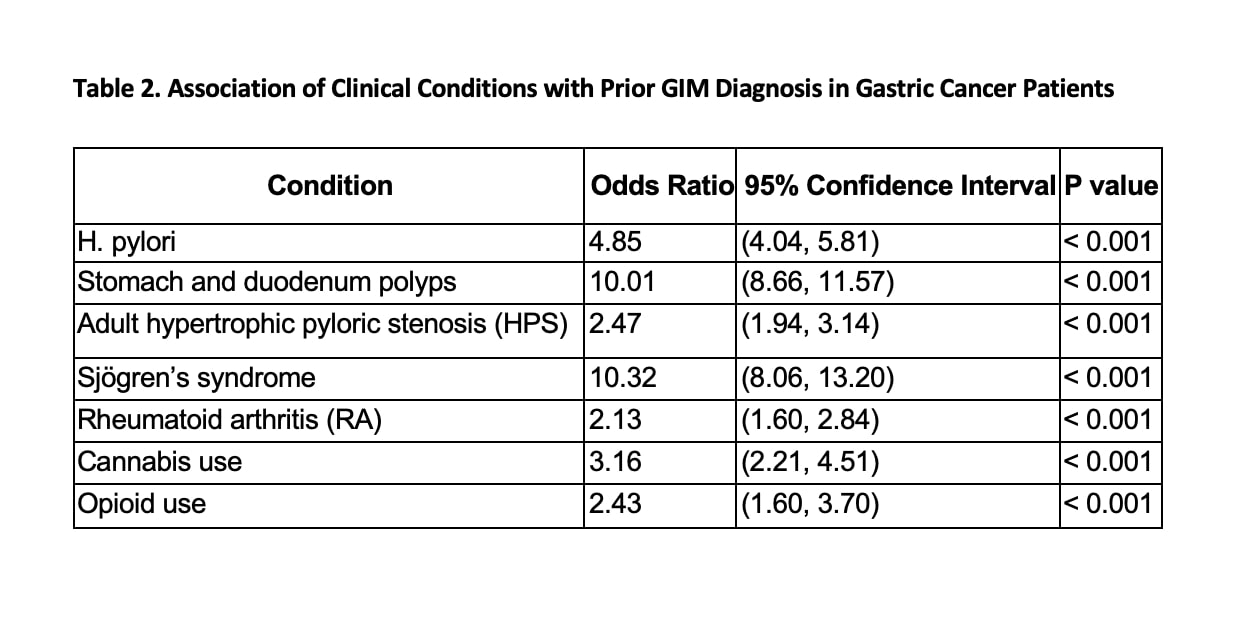
Figure: Table 2. Association of clinical conditions with Prior GIM Diagnosis in patient's with Gastric Cancer
Disclosures:
Avneet Kaur indicated no relevant financial relationships.
Anjul Verma indicated no relevant financial relationships.
Akhil Gupta indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Avneet Kaur, MBBS1, Anjul Verma, MD2, Akhil Gupta, MBBS3, Babu P. Mohan, MD4. P4191 - Gastric Intestinal Metaplasia as a Precursor to Gastric Cancer: A Cohort Analysis of Risk Factors, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
