Monday Poster Session
Category: Stomach and Spleen
P4178 - Validation of ASGE Guidelines 2025 on the Modality of Gastrostomy Feeding Placement in Patients with Malignant Dysphagia
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ali Jaan, MD
Unity Hospital
Rochester, NY
Presenting Author(s)
Ali Jaan, MD1, Umer Farooq, MD2, Adam D. Farmer, MD, PhD3
1Unity Hospital, Rochester, NY; 2Saint Louis University, Saint Louis, MO; 3SSM Health Saint Louis University Hospital, Saint Louis, MO
Introduction: The 2025 American Society for Gastrointestinal Endoscopy (ASGE) guidelines recommend percutaneous endoscopic gastrostomy (PEG) and interventional radiologist-guided gastrostomy (IR-G) as preferred methods for enteral access in patients with malignant dysphagia. However, comparative outcome data remain limited. This study evaluates these recommendations using national data to assess procedural efficacy and safety in this vulnerable population.
Methods: Using the National Readmission Database (NRD), we identified adult inpatients (aged ≥18 years) with malignant dysphagia undergoing gastrostomy, based on International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) codes. Patients were categorized into three groups: PEG, IR-G and open surgical gastrostomy. Outcomes were compared using multivariable regression analysis.
Results: Of 34,059 adult patients with malignant dysphagia undergoing gastrostomy, 85.4% received IR-G, 9.0% underwent open surgical gastrostomy, and 5.6% had PEG. Compared to PEG, open surgical gastrostomy was associated with significantly higher odds of inpatient mortality (aOR: 1.57, p=0.041), gastrostomy tube malfunction (aOR: 2.57, p< 0.001), gastrostomy-related infection (aOR: 5.47, p< 0.001) and viscus perforation (aOR: 5.29, p< 0.01). PEG and IR-G demonstrated comparable clinical outcomes and complication rates, indicating procedural equivalence. The surgical cohort had a longer length of stay by a mean of 1.5 days compared to PEG (p=0.041), while IR-G was associated with the lowest mean total hospitalization charges.
Discussion: This study supports the 2025 ASGE guidelines, confirming superior safety and mortality outcomes for PEG and IR-G compared to open surgical gastrostomy in patients with malignant dysphagia. IR-gastrostomy also offers reduced complication rates and lower hospitalization costs. Further studies are needed to investigate long-term outcomes and patient-reported experiences across these gastrostomy methods.
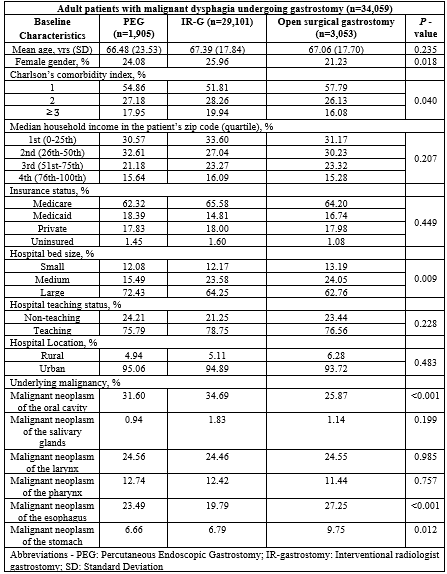
Figure: Table 1: Baseline demographic and clinical characteristics of patients with malignant dysphagia undergoing gastrostomy, stratified by procedural modality.
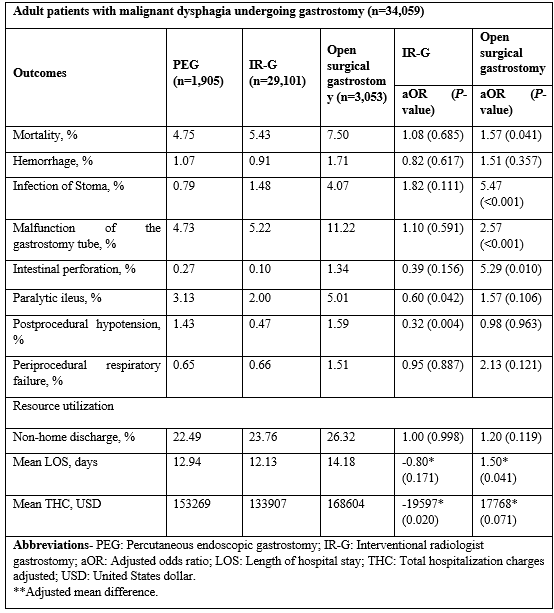
Figure: Table 2: Clinical outcomes and resource utilization in adult patients with malignant dysphagia undergoing gastrostomy, stratified by procedural modality.
Disclosures:
Ali Jaan indicated no relevant financial relationships.
Umer Farooq indicated no relevant financial relationships.
Adam D. Farmer indicated no relevant financial relationships.
Ali Jaan, MD1, Umer Farooq, MD2, Adam D. Farmer, MD, PhD3. P4178 - Validation of ASGE Guidelines 2025 on the Modality of Gastrostomy Feeding Placement in Patients with Malignant Dysphagia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Unity Hospital, Rochester, NY; 2Saint Louis University, Saint Louis, MO; 3SSM Health Saint Louis University Hospital, Saint Louis, MO
Introduction: The 2025 American Society for Gastrointestinal Endoscopy (ASGE) guidelines recommend percutaneous endoscopic gastrostomy (PEG) and interventional radiologist-guided gastrostomy (IR-G) as preferred methods for enteral access in patients with malignant dysphagia. However, comparative outcome data remain limited. This study evaluates these recommendations using national data to assess procedural efficacy and safety in this vulnerable population.
Methods: Using the National Readmission Database (NRD), we identified adult inpatients (aged ≥18 years) with malignant dysphagia undergoing gastrostomy, based on International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) codes. Patients were categorized into three groups: PEG, IR-G and open surgical gastrostomy. Outcomes were compared using multivariable regression analysis.
Results: Of 34,059 adult patients with malignant dysphagia undergoing gastrostomy, 85.4% received IR-G, 9.0% underwent open surgical gastrostomy, and 5.6% had PEG. Compared to PEG, open surgical gastrostomy was associated with significantly higher odds of inpatient mortality (aOR: 1.57, p=0.041), gastrostomy tube malfunction (aOR: 2.57, p< 0.001), gastrostomy-related infection (aOR: 5.47, p< 0.001) and viscus perforation (aOR: 5.29, p< 0.01). PEG and IR-G demonstrated comparable clinical outcomes and complication rates, indicating procedural equivalence. The surgical cohort had a longer length of stay by a mean of 1.5 days compared to PEG (p=0.041), while IR-G was associated with the lowest mean total hospitalization charges.
Discussion: This study supports the 2025 ASGE guidelines, confirming superior safety and mortality outcomes for PEG and IR-G compared to open surgical gastrostomy in patients with malignant dysphagia. IR-gastrostomy also offers reduced complication rates and lower hospitalization costs. Further studies are needed to investigate long-term outcomes and patient-reported experiences across these gastrostomy methods.
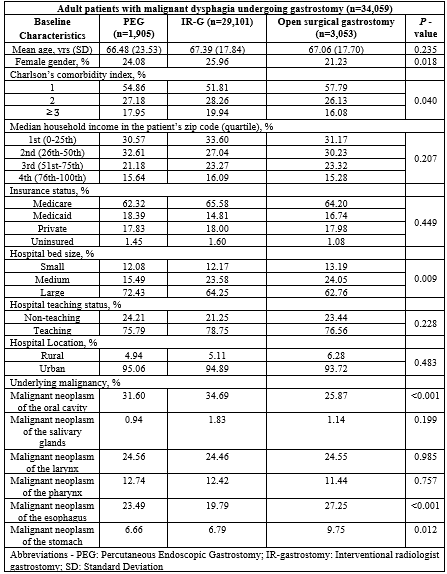
Figure: Table 1: Baseline demographic and clinical characteristics of patients with malignant dysphagia undergoing gastrostomy, stratified by procedural modality.
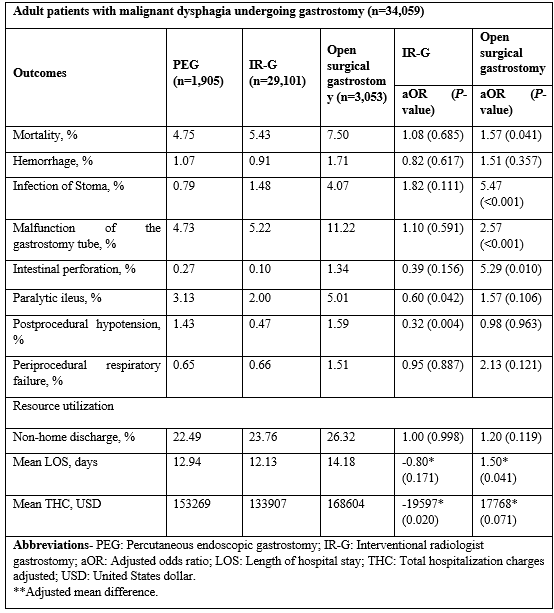
Figure: Table 2: Clinical outcomes and resource utilization in adult patients with malignant dysphagia undergoing gastrostomy, stratified by procedural modality.
Disclosures:
Ali Jaan indicated no relevant financial relationships.
Umer Farooq indicated no relevant financial relationships.
Adam D. Farmer indicated no relevant financial relationships.
Ali Jaan, MD1, Umer Farooq, MD2, Adam D. Farmer, MD, PhD3. P4178 - Validation of ASGE Guidelines 2025 on the Modality of Gastrostomy Feeding Placement in Patients with Malignant Dysphagia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
